Voriconazole Dosage
Medically reviewed by Drugs.com. Last updated on Jan 10, 2025.
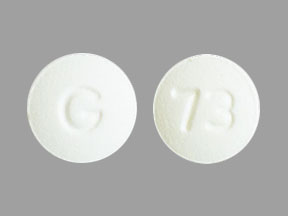
Applies to the following strengths: 40 mg/mL; 50 mg; 200 mg
Usual Adult Dose for:
- Aspergillosis - Invasive
- Candidemia
- Fungal Pneumonia
- Pseudoallescheriosis
- Systemic Fungal Infection
- Cutaneous Fungal Infection
- Fungal Infection - Disseminated
- Fungal Meningitis
- Fusariosis
- Esophageal Candidiasis
- Blastomycosis
Usual Pediatric Dose for:
- Aspergillosis - Invasive
- Candidemia
- Fungal Pneumonia
- Pseudoallescheriosis
- Systemic Fungal Infection
- Cutaneous Fungal Infection
- Fungal Infection - Disseminated
- Fungal Meningitis
- Fusariosis
- Esophageal Candidiasis
Additional dosage information:
Usual Adult Dose for Aspergillosis - Invasive
Loading Dose: 6 mg/kg IV every 12 hours for the first 24 hours
Maintenance Dose (after first 24 hours):
IV:
- Candidemia in nonneutropenic patients and other deep tissue Candida infections: 3 to 4 mg/kg IV every 12 hours
- Invasive aspergillosis: 4 mg/kg IV every 12 hours
- Scedosporiosis and fusariosis: 4 mg/kg IV every 12 hours
Oral:
- Less than 40 kg: 100 mg orally every 12 hours
- At least 40 kg: 200 mg orally every 12 hours
Comments:
- The IV formulation should be administered by IV infusion over 1 to 3 hours only, at a maximum rate of 3 mg/kg/hour.
- In healthy subject studies, 200 mg orally every 12 hours provided an exposure similar to 3 mg/kg IV every 12 hours and 300 mg orally every 12 hours provided an exposure similar to 4 mg/kg IV every 12 hours.
- Candidemia in nonneutropenic patients and other deep tissue Candida infections: Patients should be treated for at least 14 days after symptoms resolve or after last positive culture, whichever is longer.
- Candidemia in nonneutropenic patients and other deep tissue Candida infections: In clinical trials, patients with candidemia were treated using 3 mg/kg IV every 12 hours as primary therapy, while patients with other deep tissue Candida infections were treated using 4 mg/kg IV every 12 hours as salvage therapy; appropriate dose should be based on the nature and severity of the infection.
- Invasive aspergillosis and serious fungal infections due to Fusarium species and Scedosporium apiospermum: Therapy must start with the specified IV loading dose on Day 1 followed by the recommended maintenance dose; IV therapy should continue for at least 7 days. Once the patient has clinically improved and can tolerate oral medication, the oral tablet or oral suspension formulation may be used.
- Invasive aspergillosis: In a clinical trial, the median duration of IV therapy was 10 days (range: 2 to 85 days) and oral therapy was 76 days (range: 2 to 232 days).
Uses:
- For the treatment of candidemia in nonneutropenic patients and the following Candida infections: disseminated infections in skin and infections in abdomen, kidney, bladder wall, and wounds
- For the treatment of invasive aspergillosis
- For the treatment of serious fungal infections due to S apiospermum (asexual form of Pseudallescheria boydii) and Fusarium species (including Fusarium solani) in patients intolerant of (or refractory to) other therapy
Infectious Diseases Society of America (IDSA) Recommendations: 6 mg/kg IV every 12 hours for 1 day, followed by 4 mg/kg IV every 12 hours
- Oral therapy can be used at: 200 to 300 mg orally every 12 hours (or 3 to 4 mg/kg orally every 12 hours)
Comments:
- In general, recommended as primary therapy for invasive syndromes of Aspergillus
- Current guidelines should be consulted for additional information.
Usual Adult Dose for Candidemia
Loading Dose: 6 mg/kg IV every 12 hours for the first 24 hours
Maintenance Dose (after first 24 hours):
IV:
- Candidemia in nonneutropenic patients and other deep tissue Candida infections: 3 to 4 mg/kg IV every 12 hours
- Invasive aspergillosis: 4 mg/kg IV every 12 hours
- Scedosporiosis and fusariosis: 4 mg/kg IV every 12 hours
Oral:
- Less than 40 kg: 100 mg orally every 12 hours
- At least 40 kg: 200 mg orally every 12 hours
Comments:
- The IV formulation should be administered by IV infusion over 1 to 3 hours only, at a maximum rate of 3 mg/kg/hour.
- In healthy subject studies, 200 mg orally every 12 hours provided an exposure similar to 3 mg/kg IV every 12 hours and 300 mg orally every 12 hours provided an exposure similar to 4 mg/kg IV every 12 hours.
- Candidemia in nonneutropenic patients and other deep tissue Candida infections: Patients should be treated for at least 14 days after symptoms resolve or after last positive culture, whichever is longer.
- Candidemia in nonneutropenic patients and other deep tissue Candida infections: In clinical trials, patients with candidemia were treated using 3 mg/kg IV every 12 hours as primary therapy, while patients with other deep tissue Candida infections were treated using 4 mg/kg IV every 12 hours as salvage therapy; appropriate dose should be based on the nature and severity of the infection.
- Invasive aspergillosis and serious fungal infections due to Fusarium species and Scedosporium apiospermum: Therapy must start with the specified IV loading dose on Day 1 followed by the recommended maintenance dose; IV therapy should continue for at least 7 days. Once the patient has clinically improved and can tolerate oral medication, the oral tablet or oral suspension formulation may be used.
- Invasive aspergillosis: In a clinical trial, the median duration of IV therapy was 10 days (range: 2 to 85 days) and oral therapy was 76 days (range: 2 to 232 days).
Uses:
- For the treatment of candidemia in nonneutropenic patients and the following Candida infections: disseminated infections in skin and infections in abdomen, kidney, bladder wall, and wounds
- For the treatment of invasive aspergillosis
- For the treatment of serious fungal infections due to S apiospermum (asexual form of Pseudallescheria boydii) and Fusarium species (including Fusarium solani) in patients intolerant of (or refractory to) other therapy
Infectious Diseases Society of America (IDSA) Recommendations: 6 mg/kg IV every 12 hours for 1 day, followed by 4 mg/kg IV every 12 hours
- Oral therapy can be used at: 200 to 300 mg orally every 12 hours (or 3 to 4 mg/kg orally every 12 hours)
Comments:
- In general, recommended as primary therapy for invasive syndromes of Aspergillus
- Current guidelines should be consulted for additional information.
Usual Adult Dose for Fungal Pneumonia
Loading Dose: 6 mg/kg IV every 12 hours for the first 24 hours
Maintenance Dose (after first 24 hours):
IV:
- Candidemia in nonneutropenic patients and other deep tissue Candida infections: 3 to 4 mg/kg IV every 12 hours
- Invasive aspergillosis: 4 mg/kg IV every 12 hours
- Scedosporiosis and fusariosis: 4 mg/kg IV every 12 hours
Oral:
- Less than 40 kg: 100 mg orally every 12 hours
- At least 40 kg: 200 mg orally every 12 hours
Comments:
- The IV formulation should be administered by IV infusion over 1 to 3 hours only, at a maximum rate of 3 mg/kg/hour.
- In healthy subject studies, 200 mg orally every 12 hours provided an exposure similar to 3 mg/kg IV every 12 hours and 300 mg orally every 12 hours provided an exposure similar to 4 mg/kg IV every 12 hours.
- Candidemia in nonneutropenic patients and other deep tissue Candida infections: Patients should be treated for at least 14 days after symptoms resolve or after last positive culture, whichever is longer.
- Candidemia in nonneutropenic patients and other deep tissue Candida infections: In clinical trials, patients with candidemia were treated using 3 mg/kg IV every 12 hours as primary therapy, while patients with other deep tissue Candida infections were treated using 4 mg/kg IV every 12 hours as salvage therapy; appropriate dose should be based on the nature and severity of the infection.
- Invasive aspergillosis and serious fungal infections due to Fusarium species and Scedosporium apiospermum: Therapy must start with the specified IV loading dose on Day 1 followed by the recommended maintenance dose; IV therapy should continue for at least 7 days. Once the patient has clinically improved and can tolerate oral medication, the oral tablet or oral suspension formulation may be used.
- Invasive aspergillosis: In a clinical trial, the median duration of IV therapy was 10 days (range: 2 to 85 days) and oral therapy was 76 days (range: 2 to 232 days).
Uses:
- For the treatment of candidemia in nonneutropenic patients and the following Candida infections: disseminated infections in skin and infections in abdomen, kidney, bladder wall, and wounds
- For the treatment of invasive aspergillosis
- For the treatment of serious fungal infections due to S apiospermum (asexual form of Pseudallescheria boydii) and Fusarium species (including Fusarium solani) in patients intolerant of (or refractory to) other therapy
Infectious Diseases Society of America (IDSA) Recommendations: 6 mg/kg IV every 12 hours for 1 day, followed by 4 mg/kg IV every 12 hours
- Oral therapy can be used at: 200 to 300 mg orally every 12 hours (or 3 to 4 mg/kg orally every 12 hours)
Comments:
- In general, recommended as primary therapy for invasive syndromes of Aspergillus
- Current guidelines should be consulted for additional information.
Usual Adult Dose for Pseudoallescheriosis
Loading Dose: 6 mg/kg IV every 12 hours for the first 24 hours
Maintenance Dose (after first 24 hours):
IV:
- Candidemia in nonneutropenic patients and other deep tissue Candida infections: 3 to 4 mg/kg IV every 12 hours
- Invasive aspergillosis: 4 mg/kg IV every 12 hours
- Scedosporiosis and fusariosis: 4 mg/kg IV every 12 hours
Oral:
- Less than 40 kg: 100 mg orally every 12 hours
- At least 40 kg: 200 mg orally every 12 hours
Comments:
- The IV formulation should be administered by IV infusion over 1 to 3 hours only, at a maximum rate of 3 mg/kg/hour.
- In healthy subject studies, 200 mg orally every 12 hours provided an exposure similar to 3 mg/kg IV every 12 hours and 300 mg orally every 12 hours provided an exposure similar to 4 mg/kg IV every 12 hours.
- Candidemia in nonneutropenic patients and other deep tissue Candida infections: Patients should be treated for at least 14 days after symptoms resolve or after last positive culture, whichever is longer.
- Candidemia in nonneutropenic patients and other deep tissue Candida infections: In clinical trials, patients with candidemia were treated using 3 mg/kg IV every 12 hours as primary therapy, while patients with other deep tissue Candida infections were treated using 4 mg/kg IV every 12 hours as salvage therapy; appropriate dose should be based on the nature and severity of the infection.
- Invasive aspergillosis and serious fungal infections due to Fusarium species and Scedosporium apiospermum: Therapy must start with the specified IV loading dose on Day 1 followed by the recommended maintenance dose; IV therapy should continue for at least 7 days. Once the patient has clinically improved and can tolerate oral medication, the oral tablet or oral suspension formulation may be used.
- Invasive aspergillosis: In a clinical trial, the median duration of IV therapy was 10 days (range: 2 to 85 days) and oral therapy was 76 days (range: 2 to 232 days).
Uses:
- For the treatment of candidemia in nonneutropenic patients and the following Candida infections: disseminated infections in skin and infections in abdomen, kidney, bladder wall, and wounds
- For the treatment of invasive aspergillosis
- For the treatment of serious fungal infections due to S apiospermum (asexual form of Pseudallescheria boydii) and Fusarium species (including Fusarium solani) in patients intolerant of (or refractory to) other therapy
Infectious Diseases Society of America (IDSA) Recommendations: 6 mg/kg IV every 12 hours for 1 day, followed by 4 mg/kg IV every 12 hours
- Oral therapy can be used at: 200 to 300 mg orally every 12 hours (or 3 to 4 mg/kg orally every 12 hours)
Comments:
- In general, recommended as primary therapy for invasive syndromes of Aspergillus
- Current guidelines should be consulted for additional information.
Usual Adult Dose for Systemic Fungal Infection
Loading Dose: 6 mg/kg IV every 12 hours for the first 24 hours
Maintenance Dose (after first 24 hours):
IV:
- Candidemia in nonneutropenic patients and other deep tissue Candida infections: 3 to 4 mg/kg IV every 12 hours
- Invasive aspergillosis: 4 mg/kg IV every 12 hours
- Scedosporiosis and fusariosis: 4 mg/kg IV every 12 hours
Oral:
- Less than 40 kg: 100 mg orally every 12 hours
- At least 40 kg: 200 mg orally every 12 hours
Comments:
- The IV formulation should be administered by IV infusion over 1 to 3 hours only, at a maximum rate of 3 mg/kg/hour.
- In healthy subject studies, 200 mg orally every 12 hours provided an exposure similar to 3 mg/kg IV every 12 hours and 300 mg orally every 12 hours provided an exposure similar to 4 mg/kg IV every 12 hours.
- Candidemia in nonneutropenic patients and other deep tissue Candida infections: Patients should be treated for at least 14 days after symptoms resolve or after last positive culture, whichever is longer.
- Candidemia in nonneutropenic patients and other deep tissue Candida infections: In clinical trials, patients with candidemia were treated using 3 mg/kg IV every 12 hours as primary therapy, while patients with other deep tissue Candida infections were treated using 4 mg/kg IV every 12 hours as salvage therapy; appropriate dose should be based on the nature and severity of the infection.
- Invasive aspergillosis and serious fungal infections due to Fusarium species and Scedosporium apiospermum: Therapy must start with the specified IV loading dose on Day 1 followed by the recommended maintenance dose; IV therapy should continue for at least 7 days. Once the patient has clinically improved and can tolerate oral medication, the oral tablet or oral suspension formulation may be used.
- Invasive aspergillosis: In a clinical trial, the median duration of IV therapy was 10 days (range: 2 to 85 days) and oral therapy was 76 days (range: 2 to 232 days).
Uses:
- For the treatment of candidemia in nonneutropenic patients and the following Candida infections: disseminated infections in skin and infections in abdomen, kidney, bladder wall, and wounds
- For the treatment of invasive aspergillosis
- For the treatment of serious fungal infections due to S apiospermum (asexual form of Pseudallescheria boydii) and Fusarium species (including Fusarium solani) in patients intolerant of (or refractory to) other therapy
Infectious Diseases Society of America (IDSA) Recommendations: 6 mg/kg IV every 12 hours for 1 day, followed by 4 mg/kg IV every 12 hours
- Oral therapy can be used at: 200 to 300 mg orally every 12 hours (or 3 to 4 mg/kg orally every 12 hours)
Comments:
- In general, recommended as primary therapy for invasive syndromes of Aspergillus
- Current guidelines should be consulted for additional information.
Usual Adult Dose for Cutaneous Fungal Infection
Loading Dose: 6 mg/kg IV every 12 hours for the first 24 hours
Maintenance Dose (after first 24 hours):
IV:
- Candidemia in nonneutropenic patients and other deep tissue Candida infections: 3 to 4 mg/kg IV every 12 hours
- Invasive aspergillosis: 4 mg/kg IV every 12 hours
- Scedosporiosis and fusariosis: 4 mg/kg IV every 12 hours
Oral:
- Less than 40 kg: 100 mg orally every 12 hours
- At least 40 kg: 200 mg orally every 12 hours
Comments:
- The IV formulation should be administered by IV infusion over 1 to 3 hours only, at a maximum rate of 3 mg/kg/hour.
- In healthy subject studies, 200 mg orally every 12 hours provided an exposure similar to 3 mg/kg IV every 12 hours and 300 mg orally every 12 hours provided an exposure similar to 4 mg/kg IV every 12 hours.
- Candidemia in nonneutropenic patients and other deep tissue Candida infections: Patients should be treated for at least 14 days after symptoms resolve or after last positive culture, whichever is longer.
- Candidemia in nonneutropenic patients and other deep tissue Candida infections: In clinical trials, patients with candidemia were treated using 3 mg/kg IV every 12 hours as primary therapy, while patients with other deep tissue Candida infections were treated using 4 mg/kg IV every 12 hours as salvage therapy; appropriate dose should be based on the nature and severity of the infection.
- Invasive aspergillosis and serious fungal infections due to Fusarium species and Scedosporium apiospermum: Therapy must start with the specified IV loading dose on Day 1 followed by the recommended maintenance dose; IV therapy should continue for at least 7 days. Once the patient has clinically improved and can tolerate oral medication, the oral tablet or oral suspension formulation may be used.
- Invasive aspergillosis: In a clinical trial, the median duration of IV therapy was 10 days (range: 2 to 85 days) and oral therapy was 76 days (range: 2 to 232 days).
Uses:
- For the treatment of candidemia in nonneutropenic patients and the following Candida infections: disseminated infections in skin and infections in abdomen, kidney, bladder wall, and wounds
- For the treatment of invasive aspergillosis
- For the treatment of serious fungal infections due to S apiospermum (asexual form of Pseudallescheria boydii) and Fusarium species (including Fusarium solani) in patients intolerant of (or refractory to) other therapy
Infectious Diseases Society of America (IDSA) Recommendations: 6 mg/kg IV every 12 hours for 1 day, followed by 4 mg/kg IV every 12 hours
- Oral therapy can be used at: 200 to 300 mg orally every 12 hours (or 3 to 4 mg/kg orally every 12 hours)
Comments:
- In general, recommended as primary therapy for invasive syndromes of Aspergillus
- Current guidelines should be consulted for additional information.
Usual Adult Dose for Fungal Infection - Disseminated
Loading Dose: 6 mg/kg IV every 12 hours for the first 24 hours
Maintenance Dose (after first 24 hours):
IV:
- Candidemia in nonneutropenic patients and other deep tissue Candida infections: 3 to 4 mg/kg IV every 12 hours
- Invasive aspergillosis: 4 mg/kg IV every 12 hours
- Scedosporiosis and fusariosis: 4 mg/kg IV every 12 hours
Oral:
- Less than 40 kg: 100 mg orally every 12 hours
- At least 40 kg: 200 mg orally every 12 hours
Comments:
- The IV formulation should be administered by IV infusion over 1 to 3 hours only, at a maximum rate of 3 mg/kg/hour.
- In healthy subject studies, 200 mg orally every 12 hours provided an exposure similar to 3 mg/kg IV every 12 hours and 300 mg orally every 12 hours provided an exposure similar to 4 mg/kg IV every 12 hours.
- Candidemia in nonneutropenic patients and other deep tissue Candida infections: Patients should be treated for at least 14 days after symptoms resolve or after last positive culture, whichever is longer.
- Candidemia in nonneutropenic patients and other deep tissue Candida infections: In clinical trials, patients with candidemia were treated using 3 mg/kg IV every 12 hours as primary therapy, while patients with other deep tissue Candida infections were treated using 4 mg/kg IV every 12 hours as salvage therapy; appropriate dose should be based on the nature and severity of the infection.
- Invasive aspergillosis and serious fungal infections due to Fusarium species and Scedosporium apiospermum: Therapy must start with the specified IV loading dose on Day 1 followed by the recommended maintenance dose; IV therapy should continue for at least 7 days. Once the patient has clinically improved and can tolerate oral medication, the oral tablet or oral suspension formulation may be used.
- Invasive aspergillosis: In a clinical trial, the median duration of IV therapy was 10 days (range: 2 to 85 days) and oral therapy was 76 days (range: 2 to 232 days).
Uses:
- For the treatment of candidemia in nonneutropenic patients and the following Candida infections: disseminated infections in skin and infections in abdomen, kidney, bladder wall, and wounds
- For the treatment of invasive aspergillosis
- For the treatment of serious fungal infections due to S apiospermum (asexual form of Pseudallescheria boydii) and Fusarium species (including Fusarium solani) in patients intolerant of (or refractory to) other therapy
Infectious Diseases Society of America (IDSA) Recommendations: 6 mg/kg IV every 12 hours for 1 day, followed by 4 mg/kg IV every 12 hours
- Oral therapy can be used at: 200 to 300 mg orally every 12 hours (or 3 to 4 mg/kg orally every 12 hours)
Comments:
- In general, recommended as primary therapy for invasive syndromes of Aspergillus
- Current guidelines should be consulted for additional information.
Usual Adult Dose for Fungal Meningitis
Loading Dose: 6 mg/kg IV every 12 hours for the first 24 hours
Maintenance Dose (after first 24 hours):
IV:
- Candidemia in nonneutropenic patients and other deep tissue Candida infections: 3 to 4 mg/kg IV every 12 hours
- Invasive aspergillosis: 4 mg/kg IV every 12 hours
- Scedosporiosis and fusariosis: 4 mg/kg IV every 12 hours
Oral:
- Less than 40 kg: 100 mg orally every 12 hours
- At least 40 kg: 200 mg orally every 12 hours
Comments:
- The IV formulation should be administered by IV infusion over 1 to 3 hours only, at a maximum rate of 3 mg/kg/hour.
- In healthy subject studies, 200 mg orally every 12 hours provided an exposure similar to 3 mg/kg IV every 12 hours and 300 mg orally every 12 hours provided an exposure similar to 4 mg/kg IV every 12 hours.
- Candidemia in nonneutropenic patients and other deep tissue Candida infections: Patients should be treated for at least 14 days after symptoms resolve or after last positive culture, whichever is longer.
- Candidemia in nonneutropenic patients and other deep tissue Candida infections: In clinical trials, patients with candidemia were treated using 3 mg/kg IV every 12 hours as primary therapy, while patients with other deep tissue Candida infections were treated using 4 mg/kg IV every 12 hours as salvage therapy; appropriate dose should be based on the nature and severity of the infection.
- Invasive aspergillosis and serious fungal infections due to Fusarium species and Scedosporium apiospermum: Therapy must start with the specified IV loading dose on Day 1 followed by the recommended maintenance dose; IV therapy should continue for at least 7 days. Once the patient has clinically improved and can tolerate oral medication, the oral tablet or oral suspension formulation may be used.
- Invasive aspergillosis: In a clinical trial, the median duration of IV therapy was 10 days (range: 2 to 85 days) and oral therapy was 76 days (range: 2 to 232 days).
Uses:
- For the treatment of candidemia in nonneutropenic patients and the following Candida infections: disseminated infections in skin and infections in abdomen, kidney, bladder wall, and wounds
- For the treatment of invasive aspergillosis
- For the treatment of serious fungal infections due to S apiospermum (asexual form of Pseudallescheria boydii) and Fusarium species (including Fusarium solani) in patients intolerant of (or refractory to) other therapy
Infectious Diseases Society of America (IDSA) Recommendations: 6 mg/kg IV every 12 hours for 1 day, followed by 4 mg/kg IV every 12 hours
- Oral therapy can be used at: 200 to 300 mg orally every 12 hours (or 3 to 4 mg/kg orally every 12 hours)
Comments:
- In general, recommended as primary therapy for invasive syndromes of Aspergillus
- Current guidelines should be consulted for additional information.
Usual Adult Dose for Fusariosis
Loading Dose: 6 mg/kg IV every 12 hours for the first 24 hours
Maintenance Dose (after first 24 hours):
IV:
- Candidemia in nonneutropenic patients and other deep tissue Candida infections: 3 to 4 mg/kg IV every 12 hours
- Invasive aspergillosis: 4 mg/kg IV every 12 hours
- Scedosporiosis and fusariosis: 4 mg/kg IV every 12 hours
Oral:
- Less than 40 kg: 100 mg orally every 12 hours
- At least 40 kg: 200 mg orally every 12 hours
Comments:
- The IV formulation should be administered by IV infusion over 1 to 3 hours only, at a maximum rate of 3 mg/kg/hour.
- In healthy subject studies, 200 mg orally every 12 hours provided an exposure similar to 3 mg/kg IV every 12 hours and 300 mg orally every 12 hours provided an exposure similar to 4 mg/kg IV every 12 hours.
- Candidemia in nonneutropenic patients and other deep tissue Candida infections: Patients should be treated for at least 14 days after symptoms resolve or after last positive culture, whichever is longer.
- Candidemia in nonneutropenic patients and other deep tissue Candida infections: In clinical trials, patients with candidemia were treated using 3 mg/kg IV every 12 hours as primary therapy, while patients with other deep tissue Candida infections were treated using 4 mg/kg IV every 12 hours as salvage therapy; appropriate dose should be based on the nature and severity of the infection.
- Invasive aspergillosis and serious fungal infections due to Fusarium species and Scedosporium apiospermum: Therapy must start with the specified IV loading dose on Day 1 followed by the recommended maintenance dose; IV therapy should continue for at least 7 days. Once the patient has clinically improved and can tolerate oral medication, the oral tablet or oral suspension formulation may be used.
- Invasive aspergillosis: In a clinical trial, the median duration of IV therapy was 10 days (range: 2 to 85 days) and oral therapy was 76 days (range: 2 to 232 days).
Uses:
- For the treatment of candidemia in nonneutropenic patients and the following Candida infections: disseminated infections in skin and infections in abdomen, kidney, bladder wall, and wounds
- For the treatment of invasive aspergillosis
- For the treatment of serious fungal infections due to S apiospermum (asexual form of Pseudallescheria boydii) and Fusarium species (including Fusarium solani) in patients intolerant of (or refractory to) other therapy
Infectious Diseases Society of America (IDSA) Recommendations: 6 mg/kg IV every 12 hours for 1 day, followed by 4 mg/kg IV every 12 hours
- Oral therapy can be used at: 200 to 300 mg orally every 12 hours (or 3 to 4 mg/kg orally every 12 hours)
Comments:
- In general, recommended as primary therapy for invasive syndromes of Aspergillus
- Current guidelines should be consulted for additional information.
Usual Adult Dose for Esophageal Candidiasis
Less than 40 kg: 100 mg orally every 12 hours
At least 40 kg: 200 mg orally every 12 hours
Duration of therapy: At least 14 days and at least 7 days after symptoms resolve
Use: For the treatment of esophageal candidiasis
Usual Adult Dose for Blastomycosis
IDSA Recommendations: 200 to 400 mg orally twice a day
Duration of therapy: At least 12 months and until CSF abnormalities resolve
Comments:
- An oral azole is recommended for step-down therapy of CNS disease after an initial regimen of liposomal amphotericin B.
- Longer therapy may be needed for immunosuppressed patients.
- Current guidelines should be consulted for additional information.
Usual Pediatric Dose for Aspergillosis - Invasive
PEDIATRIC PATIENTS 2 TO LESS THAN 12 YEARS AND PEDIATRIC PATIENTS 12 TO 14 YEARS WEIGHING LESS THAN 50 kg:
Loading Dose: 9 mg/kg IV every 12 hours for the first 24 hours
Maintenance Dose:
- IV: 8 mg/kg IV every 12 hours after the first 24 hours
- Oral: 9 mg/kg orally every 12 hours
- Maximum dose: 350 mg orally every 12 hours
PEDIATRIC PATIENTS 12 TO 14 YEARS WEIGHING AT LEAST 50 kg AND PEDIATRIC PATIENTS 15 YEARS OR OLDER:
Loading Dose: 6 mg/kg IV every 12 hours for the first 24 hours
Maintenance Dose (after first 24 hours):
IV:
- Candidemia in nonneutropenic patients and other deep tissue Candida infections: 3 to 4 mg/kg IV every 12 hours
- Invasive aspergillosis: 4 mg/kg IV every 12 hours
- Scedosporiosis and fusariosis: 4 mg/kg IV every 12 hours
Oral:
- Less than 40 kg: 100 mg orally every 12 hours
- At least 40 kg: 200 mg orally every 12 hours
COMMENTS:
- The IV formulation should be administered by IV infusion over 1 to 3 hours only, at a maximum rate of 3 mg/kg/hour.
Pediatric Patients 2 to Less Than 12 Years and Pediatric Patients 12 to 14 Years Weighing Less Than 50 kg:
- Therapy should start with an IV regimen; oral regimen should be considered only after significant clinical improvement. It should be noted that an 8 mg/kg IV dose provides drug exposure about 2-fold higher than a 9 mg/kg oral dose.
- The oral dose recommendation for children is based on studies using the oral suspension formulation; bioequivalence between the oral suspension and tablets has not been studied in pediatrics.
- Oral bioavailability may be limited in patients 2 to 12 years with malabsorption and very low body weight for age; the IV formulation is recommended for such patients.
- Primary or salvage invasive candidiasis and candidemia: Study treatment consisted of the IV formulation with an option to switch to oral therapy after at least 5 days of IV therapy (based on subjects meeting switch criteria). This drug was administered for at least 14 days after the last positive culture; up to 42 days of therapy was permitted.
- Invasive aspergillosis: In phase 3 clinical trials, patients received IV therapy for at least 6 weeks and up to 12 weeks; patients received IV therapy for at least the first 7 days of treatment and then could be switched to the oral tablet or oral suspension formulation.
Pediatric Patients 12 to 14 Years Weighing at Least 50 kg and Pediatric Patients 15 Years or Older:
- In healthy subject studies, 200 mg orally every 12 hours provided an exposure similar to 3 mg/kg IV every 12 hours and 300 mg orally every 12 hours provided an exposure similar to 4 mg/kg IV every 12 hours.
- Candidemia in nonneutropenic patients and other deep tissue Candida infections: Patients should be treated for at least 14 days after symptoms resolve or after last positive culture, whichever is longer.
- Candidemia in nonneutropenic patients and other deep tissue Candida infections: In clinical trials, patients with candidemia were treated using 3 mg/kg IV every 12 hours as primary therapy, while patients with other deep tissue Candida infections were treated using 4 mg/kg IV every 12 hours as salvage therapy; appropriate dose should be based on the nature and severity of the infection.
- Invasive aspergillosis and serious fungal infections due to Fusarium species and S apiospermum Therapy must start with the specified IV loading dose on Day 1 followed by the recommended maintenance dose; IV therapy should continue for at least 7 days. Once the patient has clinically improved and can tolerate oral medication, the oral tablet or oral suspension formulation may be used.
- Invasive aspergillosis: In a clinical trial, the median duration of IV therapy was 10 days (range: 2 to 85 days) and oral therapy was 76 days (range: 2 to 232 days).
Uses:
- For the treatment of candidemia in nonneutropenic patients and the following Candida infections: disseminated infections in skin and infections in abdomen, kidney, bladder wall, and wounds
- For the treatment of invasive aspergillosis
- For the treatment of serious fungal infections due to S apiospermum (asexual form of P boydii) and Fusarium species (including F solani) in patients intolerant of (or refractory to) other therapy
Usual Pediatric Dose for Candidemia
PEDIATRIC PATIENTS 2 TO LESS THAN 12 YEARS AND PEDIATRIC PATIENTS 12 TO 14 YEARS WEIGHING LESS THAN 50 kg:
Loading Dose: 9 mg/kg IV every 12 hours for the first 24 hours
Maintenance Dose:
- IV: 8 mg/kg IV every 12 hours after the first 24 hours
- Oral: 9 mg/kg orally every 12 hours
- Maximum dose: 350 mg orally every 12 hours
PEDIATRIC PATIENTS 12 TO 14 YEARS WEIGHING AT LEAST 50 kg AND PEDIATRIC PATIENTS 15 YEARS OR OLDER:
Loading Dose: 6 mg/kg IV every 12 hours for the first 24 hours
Maintenance Dose (after first 24 hours):
IV:
- Candidemia in nonneutropenic patients and other deep tissue Candida infections: 3 to 4 mg/kg IV every 12 hours
- Invasive aspergillosis: 4 mg/kg IV every 12 hours
- Scedosporiosis and fusariosis: 4 mg/kg IV every 12 hours
Oral:
- Less than 40 kg: 100 mg orally every 12 hours
- At least 40 kg: 200 mg orally every 12 hours
COMMENTS:
- The IV formulation should be administered by IV infusion over 1 to 3 hours only, at a maximum rate of 3 mg/kg/hour.
Pediatric Patients 2 to Less Than 12 Years and Pediatric Patients 12 to 14 Years Weighing Less Than 50 kg:
- Therapy should start with an IV regimen; oral regimen should be considered only after significant clinical improvement. It should be noted that an 8 mg/kg IV dose provides drug exposure about 2-fold higher than a 9 mg/kg oral dose.
- The oral dose recommendation for children is based on studies using the oral suspension formulation; bioequivalence between the oral suspension and tablets has not been studied in pediatrics.
- Oral bioavailability may be limited in patients 2 to 12 years with malabsorption and very low body weight for age; the IV formulation is recommended for such patients.
- Primary or salvage invasive candidiasis and candidemia: Study treatment consisted of the IV formulation with an option to switch to oral therapy after at least 5 days of IV therapy (based on subjects meeting switch criteria). This drug was administered for at least 14 days after the last positive culture; up to 42 days of therapy was permitted.
- Invasive aspergillosis: In phase 3 clinical trials, patients received IV therapy for at least 6 weeks and up to 12 weeks; patients received IV therapy for at least the first 7 days of treatment and then could be switched to the oral tablet or oral suspension formulation.
Pediatric Patients 12 to 14 Years Weighing at Least 50 kg and Pediatric Patients 15 Years or Older:
- In healthy subject studies, 200 mg orally every 12 hours provided an exposure similar to 3 mg/kg IV every 12 hours and 300 mg orally every 12 hours provided an exposure similar to 4 mg/kg IV every 12 hours.
- Candidemia in nonneutropenic patients and other deep tissue Candida infections: Patients should be treated for at least 14 days after symptoms resolve or after last positive culture, whichever is longer.
- Candidemia in nonneutropenic patients and other deep tissue Candida infections: In clinical trials, patients with candidemia were treated using 3 mg/kg IV every 12 hours as primary therapy, while patients with other deep tissue Candida infections were treated using 4 mg/kg IV every 12 hours as salvage therapy; appropriate dose should be based on the nature and severity of the infection.
- Invasive aspergillosis and serious fungal infections due to Fusarium species and S apiospermum Therapy must start with the specified IV loading dose on Day 1 followed by the recommended maintenance dose; IV therapy should continue for at least 7 days. Once the patient has clinically improved and can tolerate oral medication, the oral tablet or oral suspension formulation may be used.
- Invasive aspergillosis: In a clinical trial, the median duration of IV therapy was 10 days (range: 2 to 85 days) and oral therapy was 76 days (range: 2 to 232 days).
Uses:
- For the treatment of candidemia in nonneutropenic patients and the following Candida infections: disseminated infections in skin and infections in abdomen, kidney, bladder wall, and wounds
- For the treatment of invasive aspergillosis
- For the treatment of serious fungal infections due to S apiospermum (asexual form of P boydii) and Fusarium species (including F solani) in patients intolerant of (or refractory to) other therapy
Usual Pediatric Dose for Fungal Pneumonia
PEDIATRIC PATIENTS 2 TO LESS THAN 12 YEARS AND PEDIATRIC PATIENTS 12 TO 14 YEARS WEIGHING LESS THAN 50 kg:
Loading Dose: 9 mg/kg IV every 12 hours for the first 24 hours
Maintenance Dose:
- IV: 8 mg/kg IV every 12 hours after the first 24 hours
- Oral: 9 mg/kg orally every 12 hours
- Maximum dose: 350 mg orally every 12 hours
PEDIATRIC PATIENTS 12 TO 14 YEARS WEIGHING AT LEAST 50 kg AND PEDIATRIC PATIENTS 15 YEARS OR OLDER:
Loading Dose: 6 mg/kg IV every 12 hours for the first 24 hours
Maintenance Dose (after first 24 hours):
IV:
- Candidemia in nonneutropenic patients and other deep tissue Candida infections: 3 to 4 mg/kg IV every 12 hours
- Invasive aspergillosis: 4 mg/kg IV every 12 hours
- Scedosporiosis and fusariosis: 4 mg/kg IV every 12 hours
Oral:
- Less than 40 kg: 100 mg orally every 12 hours
- At least 40 kg: 200 mg orally every 12 hours
COMMENTS:
- The IV formulation should be administered by IV infusion over 1 to 3 hours only, at a maximum rate of 3 mg/kg/hour.
Pediatric Patients 2 to Less Than 12 Years and Pediatric Patients 12 to 14 Years Weighing Less Than 50 kg:
- Therapy should start with an IV regimen; oral regimen should be considered only after significant clinical improvement. It should be noted that an 8 mg/kg IV dose provides drug exposure about 2-fold higher than a 9 mg/kg oral dose.
- The oral dose recommendation for children is based on studies using the oral suspension formulation; bioequivalence between the oral suspension and tablets has not been studied in pediatrics.
- Oral bioavailability may be limited in patients 2 to 12 years with malabsorption and very low body weight for age; the IV formulation is recommended for such patients.
- Primary or salvage invasive candidiasis and candidemia: Study treatment consisted of the IV formulation with an option to switch to oral therapy after at least 5 days of IV therapy (based on subjects meeting switch criteria). This drug was administered for at least 14 days after the last positive culture; up to 42 days of therapy was permitted.
- Invasive aspergillosis: In phase 3 clinical trials, patients received IV therapy for at least 6 weeks and up to 12 weeks; patients received IV therapy for at least the first 7 days of treatment and then could be switched to the oral tablet or oral suspension formulation.
Pediatric Patients 12 to 14 Years Weighing at Least 50 kg and Pediatric Patients 15 Years or Older:
- In healthy subject studies, 200 mg orally every 12 hours provided an exposure similar to 3 mg/kg IV every 12 hours and 300 mg orally every 12 hours provided an exposure similar to 4 mg/kg IV every 12 hours.
- Candidemia in nonneutropenic patients and other deep tissue Candida infections: Patients should be treated for at least 14 days after symptoms resolve or after last positive culture, whichever is longer.
- Candidemia in nonneutropenic patients and other deep tissue Candida infections: In clinical trials, patients with candidemia were treated using 3 mg/kg IV every 12 hours as primary therapy, while patients with other deep tissue Candida infections were treated using 4 mg/kg IV every 12 hours as salvage therapy; appropriate dose should be based on the nature and severity of the infection.
- Invasive aspergillosis and serious fungal infections due to Fusarium species and S apiospermum Therapy must start with the specified IV loading dose on Day 1 followed by the recommended maintenance dose; IV therapy should continue for at least 7 days. Once the patient has clinically improved and can tolerate oral medication, the oral tablet or oral suspension formulation may be used.
- Invasive aspergillosis: In a clinical trial, the median duration of IV therapy was 10 days (range: 2 to 85 days) and oral therapy was 76 days (range: 2 to 232 days).
Uses:
- For the treatment of candidemia in nonneutropenic patients and the following Candida infections: disseminated infections in skin and infections in abdomen, kidney, bladder wall, and wounds
- For the treatment of invasive aspergillosis
- For the treatment of serious fungal infections due to S apiospermum (asexual form of P boydii) and Fusarium species (including F solani) in patients intolerant of (or refractory to) other therapy
Usual Pediatric Dose for Pseudoallescheriosis
PEDIATRIC PATIENTS 2 TO LESS THAN 12 YEARS AND PEDIATRIC PATIENTS 12 TO 14 YEARS WEIGHING LESS THAN 50 kg:
Loading Dose: 9 mg/kg IV every 12 hours for the first 24 hours
Maintenance Dose:
- IV: 8 mg/kg IV every 12 hours after the first 24 hours
- Oral: 9 mg/kg orally every 12 hours
- Maximum dose: 350 mg orally every 12 hours
PEDIATRIC PATIENTS 12 TO 14 YEARS WEIGHING AT LEAST 50 kg AND PEDIATRIC PATIENTS 15 YEARS OR OLDER:
Loading Dose: 6 mg/kg IV every 12 hours for the first 24 hours
Maintenance Dose (after first 24 hours):
IV:
- Candidemia in nonneutropenic patients and other deep tissue Candida infections: 3 to 4 mg/kg IV every 12 hours
- Invasive aspergillosis: 4 mg/kg IV every 12 hours
- Scedosporiosis and fusariosis: 4 mg/kg IV every 12 hours
Oral:
- Less than 40 kg: 100 mg orally every 12 hours
- At least 40 kg: 200 mg orally every 12 hours
COMMENTS:
- The IV formulation should be administered by IV infusion over 1 to 3 hours only, at a maximum rate of 3 mg/kg/hour.
Pediatric Patients 2 to Less Than 12 Years and Pediatric Patients 12 to 14 Years Weighing Less Than 50 kg:
- Therapy should start with an IV regimen; oral regimen should be considered only after significant clinical improvement. It should be noted that an 8 mg/kg IV dose provides drug exposure about 2-fold higher than a 9 mg/kg oral dose.
- The oral dose recommendation for children is based on studies using the oral suspension formulation; bioequivalence between the oral suspension and tablets has not been studied in pediatrics.
- Oral bioavailability may be limited in patients 2 to 12 years with malabsorption and very low body weight for age; the IV formulation is recommended for such patients.
- Primary or salvage invasive candidiasis and candidemia: Study treatment consisted of the IV formulation with an option to switch to oral therapy after at least 5 days of IV therapy (based on subjects meeting switch criteria). This drug was administered for at least 14 days after the last positive culture; up to 42 days of therapy was permitted.
- Invasive aspergillosis: In phase 3 clinical trials, patients received IV therapy for at least 6 weeks and up to 12 weeks; patients received IV therapy for at least the first 7 days of treatment and then could be switched to the oral tablet or oral suspension formulation.
Pediatric Patients 12 to 14 Years Weighing at Least 50 kg and Pediatric Patients 15 Years or Older:
- In healthy subject studies, 200 mg orally every 12 hours provided an exposure similar to 3 mg/kg IV every 12 hours and 300 mg orally every 12 hours provided an exposure similar to 4 mg/kg IV every 12 hours.
- Candidemia in nonneutropenic patients and other deep tissue Candida infections: Patients should be treated for at least 14 days after symptoms resolve or after last positive culture, whichever is longer.
- Candidemia in nonneutropenic patients and other deep tissue Candida infections: In clinical trials, patients with candidemia were treated using 3 mg/kg IV every 12 hours as primary therapy, while patients with other deep tissue Candida infections were treated using 4 mg/kg IV every 12 hours as salvage therapy; appropriate dose should be based on the nature and severity of the infection.
- Invasive aspergillosis and serious fungal infections due to Fusarium species and S apiospermum Therapy must start with the specified IV loading dose on Day 1 followed by the recommended maintenance dose; IV therapy should continue for at least 7 days. Once the patient has clinically improved and can tolerate oral medication, the oral tablet or oral suspension formulation may be used.
- Invasive aspergillosis: In a clinical trial, the median duration of IV therapy was 10 days (range: 2 to 85 days) and oral therapy was 76 days (range: 2 to 232 days).
Uses:
- For the treatment of candidemia in nonneutropenic patients and the following Candida infections: disseminated infections in skin and infections in abdomen, kidney, bladder wall, and wounds
- For the treatment of invasive aspergillosis
- For the treatment of serious fungal infections due to S apiospermum (asexual form of P boydii) and Fusarium species (including F solani) in patients intolerant of (or refractory to) other therapy
Usual Pediatric Dose for Systemic Fungal Infection
PEDIATRIC PATIENTS 2 TO LESS THAN 12 YEARS AND PEDIATRIC PATIENTS 12 TO 14 YEARS WEIGHING LESS THAN 50 kg:
Loading Dose: 9 mg/kg IV every 12 hours for the first 24 hours
Maintenance Dose:
- IV: 8 mg/kg IV every 12 hours after the first 24 hours
- Oral: 9 mg/kg orally every 12 hours
- Maximum dose: 350 mg orally every 12 hours
PEDIATRIC PATIENTS 12 TO 14 YEARS WEIGHING AT LEAST 50 kg AND PEDIATRIC PATIENTS 15 YEARS OR OLDER:
Loading Dose: 6 mg/kg IV every 12 hours for the first 24 hours
Maintenance Dose (after first 24 hours):
IV:
- Candidemia in nonneutropenic patients and other deep tissue Candida infections: 3 to 4 mg/kg IV every 12 hours
- Invasive aspergillosis: 4 mg/kg IV every 12 hours
- Scedosporiosis and fusariosis: 4 mg/kg IV every 12 hours
Oral:
- Less than 40 kg: 100 mg orally every 12 hours
- At least 40 kg: 200 mg orally every 12 hours
COMMENTS:
- The IV formulation should be administered by IV infusion over 1 to 3 hours only, at a maximum rate of 3 mg/kg/hour.
Pediatric Patients 2 to Less Than 12 Years and Pediatric Patients 12 to 14 Years Weighing Less Than 50 kg:
- Therapy should start with an IV regimen; oral regimen should be considered only after significant clinical improvement. It should be noted that an 8 mg/kg IV dose provides drug exposure about 2-fold higher than a 9 mg/kg oral dose.
- The oral dose recommendation for children is based on studies using the oral suspension formulation; bioequivalence between the oral suspension and tablets has not been studied in pediatrics.
- Oral bioavailability may be limited in patients 2 to 12 years with malabsorption and very low body weight for age; the IV formulation is recommended for such patients.
- Primary or salvage invasive candidiasis and candidemia: Study treatment consisted of the IV formulation with an option to switch to oral therapy after at least 5 days of IV therapy (based on subjects meeting switch criteria). This drug was administered for at least 14 days after the last positive culture; up to 42 days of therapy was permitted.
- Invasive aspergillosis: In phase 3 clinical trials, patients received IV therapy for at least 6 weeks and up to 12 weeks; patients received IV therapy for at least the first 7 days of treatment and then could be switched to the oral tablet or oral suspension formulation.
Pediatric Patients 12 to 14 Years Weighing at Least 50 kg and Pediatric Patients 15 Years or Older:
- In healthy subject studies, 200 mg orally every 12 hours provided an exposure similar to 3 mg/kg IV every 12 hours and 300 mg orally every 12 hours provided an exposure similar to 4 mg/kg IV every 12 hours.
- Candidemia in nonneutropenic patients and other deep tissue Candida infections: Patients should be treated for at least 14 days after symptoms resolve or after last positive culture, whichever is longer.
- Candidemia in nonneutropenic patients and other deep tissue Candida infections: In clinical trials, patients with candidemia were treated using 3 mg/kg IV every 12 hours as primary therapy, while patients with other deep tissue Candida infections were treated using 4 mg/kg IV every 12 hours as salvage therapy; appropriate dose should be based on the nature and severity of the infection.
- Invasive aspergillosis and serious fungal infections due to Fusarium species and S apiospermum Therapy must start with the specified IV loading dose on Day 1 followed by the recommended maintenance dose; IV therapy should continue for at least 7 days. Once the patient has clinically improved and can tolerate oral medication, the oral tablet or oral suspension formulation may be used.
- Invasive aspergillosis: In a clinical trial, the median duration of IV therapy was 10 days (range: 2 to 85 days) and oral therapy was 76 days (range: 2 to 232 days).
Uses:
- For the treatment of candidemia in nonneutropenic patients and the following Candida infections: disseminated infections in skin and infections in abdomen, kidney, bladder wall, and wounds
- For the treatment of invasive aspergillosis
- For the treatment of serious fungal infections due to S apiospermum (asexual form of P boydii) and Fusarium species (including F solani) in patients intolerant of (or refractory to) other therapy
Usual Pediatric Dose for Cutaneous Fungal Infection
PEDIATRIC PATIENTS 2 TO LESS THAN 12 YEARS AND PEDIATRIC PATIENTS 12 TO 14 YEARS WEIGHING LESS THAN 50 kg:
Loading Dose: 9 mg/kg IV every 12 hours for the first 24 hours
Maintenance Dose:
- IV: 8 mg/kg IV every 12 hours after the first 24 hours
- Oral: 9 mg/kg orally every 12 hours
- Maximum dose: 350 mg orally every 12 hours
PEDIATRIC PATIENTS 12 TO 14 YEARS WEIGHING AT LEAST 50 kg AND PEDIATRIC PATIENTS 15 YEARS OR OLDER:
Loading Dose: 6 mg/kg IV every 12 hours for the first 24 hours
Maintenance Dose (after first 24 hours):
IV:
- Candidemia in nonneutropenic patients and other deep tissue Candida infections: 3 to 4 mg/kg IV every 12 hours
- Invasive aspergillosis: 4 mg/kg IV every 12 hours
- Scedosporiosis and fusariosis: 4 mg/kg IV every 12 hours
Oral:
- Less than 40 kg: 100 mg orally every 12 hours
- At least 40 kg: 200 mg orally every 12 hours
COMMENTS:
- The IV formulation should be administered by IV infusion over 1 to 3 hours only, at a maximum rate of 3 mg/kg/hour.
Pediatric Patients 2 to Less Than 12 Years and Pediatric Patients 12 to 14 Years Weighing Less Than 50 kg:
- Therapy should start with an IV regimen; oral regimen should be considered only after significant clinical improvement. It should be noted that an 8 mg/kg IV dose provides drug exposure about 2-fold higher than a 9 mg/kg oral dose.
- The oral dose recommendation for children is based on studies using the oral suspension formulation; bioequivalence between the oral suspension and tablets has not been studied in pediatrics.
- Oral bioavailability may be limited in patients 2 to 12 years with malabsorption and very low body weight for age; the IV formulation is recommended for such patients.
- Primary or salvage invasive candidiasis and candidemia: Study treatment consisted of the IV formulation with an option to switch to oral therapy after at least 5 days of IV therapy (based on subjects meeting switch criteria). This drug was administered for at least 14 days after the last positive culture; up to 42 days of therapy was permitted.
- Invasive aspergillosis: In phase 3 clinical trials, patients received IV therapy for at least 6 weeks and up to 12 weeks; patients received IV therapy for at least the first 7 days of treatment and then could be switched to the oral tablet or oral suspension formulation.
Pediatric Patients 12 to 14 Years Weighing at Least 50 kg and Pediatric Patients 15 Years or Older:
- In healthy subject studies, 200 mg orally every 12 hours provided an exposure similar to 3 mg/kg IV every 12 hours and 300 mg orally every 12 hours provided an exposure similar to 4 mg/kg IV every 12 hours.
- Candidemia in nonneutropenic patients and other deep tissue Candida infections: Patients should be treated for at least 14 days after symptoms resolve or after last positive culture, whichever is longer.
- Candidemia in nonneutropenic patients and other deep tissue Candida infections: In clinical trials, patients with candidemia were treated using 3 mg/kg IV every 12 hours as primary therapy, while patients with other deep tissue Candida infections were treated using 4 mg/kg IV every 12 hours as salvage therapy; appropriate dose should be based on the nature and severity of the infection.
- Invasive aspergillosis and serious fungal infections due to Fusarium species and S apiospermum Therapy must start with the specified IV loading dose on Day 1 followed by the recommended maintenance dose; IV therapy should continue for at least 7 days. Once the patient has clinically improved and can tolerate oral medication, the oral tablet or oral suspension formulation may be used.
- Invasive aspergillosis: In a clinical trial, the median duration of IV therapy was 10 days (range: 2 to 85 days) and oral therapy was 76 days (range: 2 to 232 days).
Uses:
- For the treatment of candidemia in nonneutropenic patients and the following Candida infections: disseminated infections in skin and infections in abdomen, kidney, bladder wall, and wounds
- For the treatment of invasive aspergillosis
- For the treatment of serious fungal infections due to S apiospermum (asexual form of P boydii) and Fusarium species (including F solani) in patients intolerant of (or refractory to) other therapy
Usual Pediatric Dose for Fungal Infection - Disseminated
PEDIATRIC PATIENTS 2 TO LESS THAN 12 YEARS AND PEDIATRIC PATIENTS 12 TO 14 YEARS WEIGHING LESS THAN 50 kg:
Loading Dose: 9 mg/kg IV every 12 hours for the first 24 hours
Maintenance Dose:
- IV: 8 mg/kg IV every 12 hours after the first 24 hours
- Oral: 9 mg/kg orally every 12 hours
- Maximum dose: 350 mg orally every 12 hours
PEDIATRIC PATIENTS 12 TO 14 YEARS WEIGHING AT LEAST 50 kg AND PEDIATRIC PATIENTS 15 YEARS OR OLDER:
Loading Dose: 6 mg/kg IV every 12 hours for the first 24 hours
Maintenance Dose (after first 24 hours):
IV:
- Candidemia in nonneutropenic patients and other deep tissue Candida infections: 3 to 4 mg/kg IV every 12 hours
- Invasive aspergillosis: 4 mg/kg IV every 12 hours
- Scedosporiosis and fusariosis: 4 mg/kg IV every 12 hours
Oral:
- Less than 40 kg: 100 mg orally every 12 hours
- At least 40 kg: 200 mg orally every 12 hours
COMMENTS:
- The IV formulation should be administered by IV infusion over 1 to 3 hours only, at a maximum rate of 3 mg/kg/hour.
Pediatric Patients 2 to Less Than 12 Years and Pediatric Patients 12 to 14 Years Weighing Less Than 50 kg:
- Therapy should start with an IV regimen; oral regimen should be considered only after significant clinical improvement. It should be noted that an 8 mg/kg IV dose provides drug exposure about 2-fold higher than a 9 mg/kg oral dose.
- The oral dose recommendation for children is based on studies using the oral suspension formulation; bioequivalence between the oral suspension and tablets has not been studied in pediatrics.
- Oral bioavailability may be limited in patients 2 to 12 years with malabsorption and very low body weight for age; the IV formulation is recommended for such patients.
- Primary or salvage invasive candidiasis and candidemia: Study treatment consisted of the IV formulation with an option to switch to oral therapy after at least 5 days of IV therapy (based on subjects meeting switch criteria). This drug was administered for at least 14 days after the last positive culture; up to 42 days of therapy was permitted.
- Invasive aspergillosis: In phase 3 clinical trials, patients received IV therapy for at least 6 weeks and up to 12 weeks; patients received IV therapy for at least the first 7 days of treatment and then could be switched to the oral tablet or oral suspension formulation.
Pediatric Patients 12 to 14 Years Weighing at Least 50 kg and Pediatric Patients 15 Years or Older:
- In healthy subject studies, 200 mg orally every 12 hours provided an exposure similar to 3 mg/kg IV every 12 hours and 300 mg orally every 12 hours provided an exposure similar to 4 mg/kg IV every 12 hours.
- Candidemia in nonneutropenic patients and other deep tissue Candida infections: Patients should be treated for at least 14 days after symptoms resolve or after last positive culture, whichever is longer.
- Candidemia in nonneutropenic patients and other deep tissue Candida infections: In clinical trials, patients with candidemia were treated using 3 mg/kg IV every 12 hours as primary therapy, while patients with other deep tissue Candida infections were treated using 4 mg/kg IV every 12 hours as salvage therapy; appropriate dose should be based on the nature and severity of the infection.
- Invasive aspergillosis and serious fungal infections due to Fusarium species and S apiospermum Therapy must start with the specified IV loading dose on Day 1 followed by the recommended maintenance dose; IV therapy should continue for at least 7 days. Once the patient has clinically improved and can tolerate oral medication, the oral tablet or oral suspension formulation may be used.
- Invasive aspergillosis: In a clinical trial, the median duration of IV therapy was 10 days (range: 2 to 85 days) and oral therapy was 76 days (range: 2 to 232 days).
Uses:
- For the treatment of candidemia in nonneutropenic patients and the following Candida infections: disseminated infections in skin and infections in abdomen, kidney, bladder wall, and wounds
- For the treatment of invasive aspergillosis
- For the treatment of serious fungal infections due to S apiospermum (asexual form of P boydii) and Fusarium species (including F solani) in patients intolerant of (or refractory to) other therapy
Usual Pediatric Dose for Fungal Meningitis
PEDIATRIC PATIENTS 2 TO LESS THAN 12 YEARS AND PEDIATRIC PATIENTS 12 TO 14 YEARS WEIGHING LESS THAN 50 kg:
Loading Dose: 9 mg/kg IV every 12 hours for the first 24 hours
Maintenance Dose:
- IV: 8 mg/kg IV every 12 hours after the first 24 hours
- Oral: 9 mg/kg orally every 12 hours
- Maximum dose: 350 mg orally every 12 hours
PEDIATRIC PATIENTS 12 TO 14 YEARS WEIGHING AT LEAST 50 kg AND PEDIATRIC PATIENTS 15 YEARS OR OLDER:
Loading Dose: 6 mg/kg IV every 12 hours for the first 24 hours
Maintenance Dose (after first 24 hours):
IV:
- Candidemia in nonneutropenic patients and other deep tissue Candida infections: 3 to 4 mg/kg IV every 12 hours
- Invasive aspergillosis: 4 mg/kg IV every 12 hours
- Scedosporiosis and fusariosis: 4 mg/kg IV every 12 hours
Oral:
- Less than 40 kg: 100 mg orally every 12 hours
- At least 40 kg: 200 mg orally every 12 hours
COMMENTS:
- The IV formulation should be administered by IV infusion over 1 to 3 hours only, at a maximum rate of 3 mg/kg/hour.
Pediatric Patients 2 to Less Than 12 Years and Pediatric Patients 12 to 14 Years Weighing Less Than 50 kg:
- Therapy should start with an IV regimen; oral regimen should be considered only after significant clinical improvement. It should be noted that an 8 mg/kg IV dose provides drug exposure about 2-fold higher than a 9 mg/kg oral dose.
- The oral dose recommendation for children is based on studies using the oral suspension formulation; bioequivalence between the oral suspension and tablets has not been studied in pediatrics.
- Oral bioavailability may be limited in patients 2 to 12 years with malabsorption and very low body weight for age; the IV formulation is recommended for such patients.
- Primary or salvage invasive candidiasis and candidemia: Study treatment consisted of the IV formulation with an option to switch to oral therapy after at least 5 days of IV therapy (based on subjects meeting switch criteria). This drug was administered for at least 14 days after the last positive culture; up to 42 days of therapy was permitted.
- Invasive aspergillosis: In phase 3 clinical trials, patients received IV therapy for at least 6 weeks and up to 12 weeks; patients received IV therapy for at least the first 7 days of treatment and then could be switched to the oral tablet or oral suspension formulation.
Pediatric Patients 12 to 14 Years Weighing at Least 50 kg and Pediatric Patients 15 Years or Older:
- In healthy subject studies, 200 mg orally every 12 hours provided an exposure similar to 3 mg/kg IV every 12 hours and 300 mg orally every 12 hours provided an exposure similar to 4 mg/kg IV every 12 hours.
- Candidemia in nonneutropenic patients and other deep tissue Candida infections: Patients should be treated for at least 14 days after symptoms resolve or after last positive culture, whichever is longer.
- Candidemia in nonneutropenic patients and other deep tissue Candida infections: In clinical trials, patients with candidemia were treated using 3 mg/kg IV every 12 hours as primary therapy, while patients with other deep tissue Candida infections were treated using 4 mg/kg IV every 12 hours as salvage therapy; appropriate dose should be based on the nature and severity of the infection.
- Invasive aspergillosis and serious fungal infections due to Fusarium species and S apiospermum Therapy must start with the specified IV loading dose on Day 1 followed by the recommended maintenance dose; IV therapy should continue for at least 7 days. Once the patient has clinically improved and can tolerate oral medication, the oral tablet or oral suspension formulation may be used.
- Invasive aspergillosis: In a clinical trial, the median duration of IV therapy was 10 days (range: 2 to 85 days) and oral therapy was 76 days (range: 2 to 232 days).
Uses:
- For the treatment of candidemia in nonneutropenic patients and the following Candida infections: disseminated infections in skin and infections in abdomen, kidney, bladder wall, and wounds
- For the treatment of invasive aspergillosis
- For the treatment of serious fungal infections due to S apiospermum (asexual form of P boydii) and Fusarium species (including F solani) in patients intolerant of (or refractory to) other therapy
Usual Pediatric Dose for Fusariosis
PEDIATRIC PATIENTS 2 TO LESS THAN 12 YEARS AND PEDIATRIC PATIENTS 12 TO 14 YEARS WEIGHING LESS THAN 50 kg:
Loading Dose: 9 mg/kg IV every 12 hours for the first 24 hours
Maintenance Dose:
- IV: 8 mg/kg IV every 12 hours after the first 24 hours
- Oral: 9 mg/kg orally every 12 hours
- Maximum dose: 350 mg orally every 12 hours
PEDIATRIC PATIENTS 12 TO 14 YEARS WEIGHING AT LEAST 50 kg AND PEDIATRIC PATIENTS 15 YEARS OR OLDER:
Loading Dose: 6 mg/kg IV every 12 hours for the first 24 hours
Maintenance Dose (after first 24 hours):
IV:
- Candidemia in nonneutropenic patients and other deep tissue Candida infections: 3 to 4 mg/kg IV every 12 hours
- Invasive aspergillosis: 4 mg/kg IV every 12 hours
- Scedosporiosis and fusariosis: 4 mg/kg IV every 12 hours
Oral:
- Less than 40 kg: 100 mg orally every 12 hours
- At least 40 kg: 200 mg orally every 12 hours
COMMENTS:
- The IV formulation should be administered by IV infusion over 1 to 3 hours only, at a maximum rate of 3 mg/kg/hour.
Pediatric Patients 2 to Less Than 12 Years and Pediatric Patients 12 to 14 Years Weighing Less Than 50 kg:
- Therapy should start with an IV regimen; oral regimen should be considered only after significant clinical improvement. It should be noted that an 8 mg/kg IV dose provides drug exposure about 2-fold higher than a 9 mg/kg oral dose.
- The oral dose recommendation for children is based on studies using the oral suspension formulation; bioequivalence between the oral suspension and tablets has not been studied in pediatrics.
- Oral bioavailability may be limited in patients 2 to 12 years with malabsorption and very low body weight for age; the IV formulation is recommended for such patients.
- Primary or salvage invasive candidiasis and candidemia: Study treatment consisted of the IV formulation with an option to switch to oral therapy after at least 5 days of IV therapy (based on subjects meeting switch criteria). This drug was administered for at least 14 days after the last positive culture; up to 42 days of therapy was permitted.
- Invasive aspergillosis: In phase 3 clinical trials, patients received IV therapy for at least 6 weeks and up to 12 weeks; patients received IV therapy for at least the first 7 days of treatment and then could be switched to the oral tablet or oral suspension formulation.
Pediatric Patients 12 to 14 Years Weighing at Least 50 kg and Pediatric Patients 15 Years or Older:
- In healthy subject studies, 200 mg orally every 12 hours provided an exposure similar to 3 mg/kg IV every 12 hours and 300 mg orally every 12 hours provided an exposure similar to 4 mg/kg IV every 12 hours.
- Candidemia in nonneutropenic patients and other deep tissue Candida infections: Patients should be treated for at least 14 days after symptoms resolve or after last positive culture, whichever is longer.
- Candidemia in nonneutropenic patients and other deep tissue Candida infections: In clinical trials, patients with candidemia were treated using 3 mg/kg IV every 12 hours as primary therapy, while patients with other deep tissue Candida infections were treated using 4 mg/kg IV every 12 hours as salvage therapy; appropriate dose should be based on the nature and severity of the infection.
- Invasive aspergillosis and serious fungal infections due to Fusarium species and S apiospermum Therapy must start with the specified IV loading dose on Day 1 followed by the recommended maintenance dose; IV therapy should continue for at least 7 days. Once the patient has clinically improved and can tolerate oral medication, the oral tablet or oral suspension formulation may be used.
- Invasive aspergillosis: In a clinical trial, the median duration of IV therapy was 10 days (range: 2 to 85 days) and oral therapy was 76 days (range: 2 to 232 days).
Uses:
- For the treatment of candidemia in nonneutropenic patients and the following Candida infections: disseminated infections in skin and infections in abdomen, kidney, bladder wall, and wounds
- For the treatment of invasive aspergillosis
- For the treatment of serious fungal infections due to S apiospermum (asexual form of P boydii) and Fusarium species (including F solani) in patients intolerant of (or refractory to) other therapy
Usual Pediatric Dose for Esophageal Candidiasis
Pediatric Patients 2 to Less Than 12 Years and Pediatric Patients 12 to 14 Years Weighing Less Than 50 kg:
- IV: 4 mg/kg IV every 12 hours
- Oral: 9 mg/kg orally every 12 hours
- Maximum dose: 350 mg orally every 12 hours
Pediatric Patients 12 to 14 Years Weighing at Least 50 kg and Pediatric Patients 15 Years or Older:
- Less than 40 kg: 100 mg orally every 12 hours
- At least 40 kg: 200 mg orally every 12 hours
COMMENTS:
- The IV formulation should be administered by IV infusion over 1 to 3 hours only, at a maximum rate of 3 mg/kg/hour.
Pediatric Patients 2 to Less Than 12 Years and Pediatric Patients 12 to 14 Years Weighing Less Than 50 kg:
- Therapy should start with an IV regimen; oral regimen should be considered only after significant clinical improvement. It should be noted that an 8 mg/kg IV dose provides drug exposure about 2-fold higher than a 9 mg/kg oral dose.
- The oral dose recommendation for children is based on studies using the oral suspension formulation; bioequivalence between the oral suspension and tablets has not been studied in pediatrics.
- Oral bioavailability may be limited in patients 2 to 12 years with malabsorption and very low body weight for age; the IV formulation is recommended for such patients.
- Primary or salvage esophageal candidiasis: Study treatment consisted of the IV formulation with an option to switch to oral therapy after at least 5 days of IV therapy (based on subjects meeting switch criteria). Patients were treated for at least 7 days after clinical signs/symptoms resolved; up to 42 days of therapy was permitted.
Use: For the treatment of esophageal candidiasis
Renal Dose Adjustments
Adult Patients:
IV:
- Moderate or severe renal dysfunction (CrCl less than 50 mL/min): Oral formulation should be used unless benefit/risk assessment justifies use of IV formulation.
Oral:
- Mild to severe renal dysfunction: No adjustment recommended
Pediatric Patients:
- Renal dysfunction: Data not available
Comments:
- Accumulation of the IV vehicle (sulfobutyl ether beta-cyclodextrin sodium [SBECD]), occurs in adult patients with moderate or severe renal dysfunction.
- Serum creatinine levels should be closely monitored in adult patients with moderate or severe renal dysfunction; if increases occur, switching to oral therapy should be considered.
Liver Dose Adjustments
Adult Patients:
Mild to moderate liver dysfunction (Child-Pugh A and B): The maintenance dose should be reduced.
Severe liver dysfunction: Data not available
Baseline liver function tests (ALT, AST) up to 5 times the upper limit of normal (5 x ULN): No adjustment recommended
Mild to moderate liver cirrhosis (Child-Pugh A and B):
- Loading dose: No adjustment recommended
- Maintenance dose: Dose should be reduced by one-half.
Pediatric Patients:
- Liver dysfunction: Data not available
Comments:
- For adults, duration of therapy should be based on the severity of the patient's underlying disease, recovery from immunosuppression, and clinical response.
- Continued monitoring of liver function tests for further elevations is recommended for adult patients with baseline liver function tests up to 5 x ULN.
- This drug should only be used in adult patients with severe liver dysfunction if the benefit outweighs the risk.
- Adult patients with liver dysfunction must be carefully monitored for drug toxicity.
Dose Adjustments
ADULT PATIENTS:
If patient is unable to tolerate 4 mg/kg IV every 12 hours, the IV maintenance dose should be reduced to 3 mg/kg IV every 12 hours.
If patient response is inadequate, the oral maintenance dose may be increased to:
- Less than 40 kg: 150 mg orally every 12 hours
- At least 40 kg: 300 mg orally every 12 hours
If patient is unable to tolerate the higher dose, the oral maintenance dose should be reduced by 50 mg steps to a minimum of:
- Less than 40 kg: 100 mg orally every 12 hours
- At least 40 kg: 200 mg orally every 12 hours
PEDIATRIC PATIENTS:
Pediatric Patients 2 to Less Than 12 Years and Pediatric Patients 12 to 14 Years Weighing Less Than 50 kg:
- If patient response is inadequate and patient can tolerate the initial IV maintenance dose, the maintenance dose may be increased by 1 mg/kg steps.
- If patient response is inadequate and patient can tolerate the oral maintenance dose, the dose may be increased by 1 mg/kg steps or 50 mg steps up to a maximum of 350 mg orally every 12 hours.
- If patient is unable to tolerate the initial IV maintenance dose, the dose should be reduced by 1 mg/kg steps.
- If patient is unable to tolerate the oral maintenance dose, the dose should be reduced by 1 mg/kg or 50 mg steps.
Pediatric Patients 12 to 14 Years Weighing at Least 50 kg and Pediatric Patients 15 Years or Older: The optimal method for titrating dosage recommended for adults should be used.
COADMINISTRATION WITH PHENYTOIN OR EFAVIRENZ:
- The maintenance dose should be increased when coadministered with phenytoin or efavirenz; the optimal method for titrating dosage should be used.
- The manufacturer product information should be consulted for further guidance.
Precautions
CONTRAINDICATIONS:
- Known hypersensitivity to the active component or any of the ingredients
- Coadministration with pimozide, quinidine, ivabradine, sirolimus, rifampin, carbamazepine, long-acting barbiturates, St. John's wort, high-dose ritonavir (400 mg every 12 hours), rifabutin, ergot alkaloids (ergotamine, dihydroergotamine), naloxegol, tolvaptan, lurasidone
- Coadministration of standard doses of this drug with efavirenz 400 mg every 24 hours or higher
- Coadministration with venetoclax at initiation and during the dose-titration phase in patients with chronic lymphocytic leukemia or small lymphocytic lymphoma
Safety and efficacy have not been established in patients younger than 2 years; this drug is not recommended for use in these patients.
Consult WARNINGS section for additional precautions.
Dialysis
Adult Patients:
- Hemodialysis: No adjustment recommended
Comments:
- This drug and the IV vehicle (SBECD) are dialyzable.
- A 4-hour hemodialysis session does not remove a sufficient amount of this drug to require dose adjustment.
Other Comments
Administration advice:
- IV: Administer diluted IV solution by IV infusion over 1 to 3 hours only, at a maximum rate of 3 mg/kg/hour; do not administer as IV bolus injection.
- IV: Do not infuse concomitantly with any blood product or short-term infusion of concentrated electrolytes, even if the 2 infusions are running in separate IV lines (or cannulas); correct electrolyte disturbances (e.g., hypokalemia, hypomagnesemia, hypocalcemia) before starting and during therapy.
- IV: May infuse concurrently with other IV solutions containing non-concentrated electrolytes; must infuse through a separate line
- IV: May infuse concurrently with total parenteral nutrition; must infuse through a separate line or a different port (if infused through a multiple-lumen catheter)
- Oral: Administer the tablets or oral suspension at least 1 hour before or after a meal.
- Oral: Shake the oral suspension about 10 seconds before each use; only administer using the oral dispenser provided with the product.
- Duration of therapy depends on the severity of the patient's underlying disease, recovery from immunosuppression, and clinical response.
Storage requirements:
- Powder for solution for injection: Store at 15C to 30C (59F to 86F).
- After reconstitution: If not used at once, storage should not exceed 24 hours at 2C to 8C (36F to 46F).
- Powder for oral suspension: Store in refrigerator at 2C to 8C (36F to 46F).
- After reconstitution: Store at 15C to 30C (59F to 86F); do not refrigerate or freeze. Keep container tightly closed. Discard 14 days after reconstitution.
- Tablets: Store at 15C to 30C (59F to 86F).
Reconstitution/preparation techniques:
- The manufacturer product information should be consulted.
- IV: Reconstitute and dilute before administration as an infusion.
- Oral suspension: Do not mix with any other medication or additional flavoring agent (before or after reconstitution); do not further dilute with water or other vehicles.
IV compatibility:
- Compatible diluents: 0.9% Sodium Chloride USP; Lactated Ringers USP; 5% Dextrose and Lactated Ringers USP; 5% Dextrose and 0.45% Sodium Chloride USP; 5% Dextrose USP; 5% Dextrose and 20 mEq Potassium Chloride USP; 0.45% Sodium Chloride USP; 5% Dextrose and 0.9% Sodium Chloride USP
- Incompatibilities: 4.2% Sodium Bicarbonate Infusion
- Compatibility with diluents other than those listed above is unknown.
General:
- Specimens for fungal culture and other relevant laboratory studies (including histopathology) should be obtained before therapy to isolate and identify causative organisms; therapy may be started before results are known, but once available, antifungal therapy should be adjusted accordingly.
- The recommended oral maintenance dose of 200 mg achieves an exposure to this drug similar to 3 mg/kg IV; a 300 mg oral dose achieves an exposure similar to 4 mg/kg IV.
- Invasive aspergillosis: In clinical trials, most isolates recovered were Aspergillus fumigatus; there was a small number of cases of culture-proven disease due to Aspergillus species other than A fumigatus.
- The tablet formulations contain lactose; patients with galactose intolerance, total lactase deficiency, or glucose-galactose malabsorption should not take products containing lactose.
Monitoring:
- Gastrointestinal: For pancreatitis in at-risk patients
- General: For drug toxicity in patients with liver dysfunction
- Hepatic: Hepatic function in adult and pediatric patients; serum transaminase levels and bilirubin (at start of therapy and at least weekly for the first month; may reduce to monthly if no clinically significant changes); hepatic function, especially liver function tests and bilirubin; liver function tests in adults with baseline liver function tests up to 5 x ULN
- Metabolic: Electrolyte disturbances (before starting and during therapy)
- Ocular: Visual function including visual acuity, visual field, and color perception (if therapy extends beyond 28 days)
- Renal: Renal function, especially serum creatinine; for abnormal renal function; serum creatinine levels in adult patients with moderate or severe renal dysfunction and in pediatric patients
Patient advice:
- Read the US FDA-approved patient labeling (Patient Information).
- Contact your health care provider immediately if new/worsening skin rash develops.
- Avoid exposure to direct sunlight and use measures such as protective clothing and sunscreen with high sun protection factor (SPF).
- Seek immediate medical care if signs/symptoms of Cushing's syndrome or adrenal insufficiency develop.
- Patients of childbearing potential: Use effective contraception during therapy.
- Do not drive at night while using this drug.
- Until you know how this drug affects you, avoid potentially hazardous tasks (such as driving or operating machinery).
More about voriconazole
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (7)
- Drug images
- Side effects
- During pregnancy
- Drug class: azole antifungals
- Breastfeeding
- En español
Patient resources
- Voriconazole oral/injection drug information
- Voriconazole (Intravenous) (Advanced Reading)
- Voriconazole (Oral) (Advanced Reading)
- Voriconazole Tablets
- Voriconazole Injection
- Voriconazole Suspension
Other brands
Professional resources
- Voriconazole monograph
- Voriconazole (FDA)
- Voriconazole Injection (FDA)
- Voriconazole Suspension (FDA)
Other brands
Related treatment guides
See also:
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.