Voriconazole (Monograph)
Brand name: Vfend
Drug class: Azoles
VA class: AM700
Chemical name: (αR,βS)-α-(2,4,-difluorophenyl)-5-fluoro-β-methyl-α-(1H-1,2,4-triazol-1-yl-methyl)-4-pyrimidineethanol
Molecular formula: C16H14F3N5O
CAS number: 137234-62-9
Introduction
Antifungal; azole (triazole); synthetic derivative of fluconazole.
Uses for Voriconazole
Aspergillosis
Treatment of invasive aspergillosis. A drug of choice.
Has been effective for primary and salvage therapy of invasive aspergillosis, including treatment of invasive aspergillosis in patients intolerant of, or whose disease was refractory to, other antifungals.
IDSA considers voriconazole the drug of choice for primary treatment of invasive aspergillosis in most patients and amphotericin B the preferred alternative. For salvage therapy in patients refractory to or intolerant of primary antifungal therapy, IDSA recommends amphotericin B, caspofungin, micafungin, posaconazole, or itraconazole. For empiric or preemptive therapy of presumed aspergillosis, IDSA recommends amphotericin B, caspofungin, itraconazole, or voriconazole.
For HIV-infected adults and adolescents with invasive aspergillosis, CDC, NIH, and IDSA recommend voriconazole as the drug of choice; IV amphotericin B, IV echinocandins (caspofungin, micafungin, anidulafungin), and oral posaconazole are alternatives. Voriconazole also considered drug of choice for treatment of invasive aspergillosis in HIV-infected children† [off-label]; IV amphotericin B and IV caspofungin are alternatives.
Candidemia and Disseminated Candida Infections
Treatment of candidemia in nonneutropenic patients. Has been effective in Candida albicans, C. tropicalis, C. parapsilosis, C. glabrata, or C. krusei infections.
Treatment of disseminated Candida infections involving the skin, abdomen, kidney, bladder wall, or wounds.
For treatment of candidemia in nonneutropenic patients or for empiric treatment of suspected invasive candidiasis in such patients, IDSA recommends fluconazole or an IV echinocandin (caspofungin, micafungin, anidulafungin) for initial therapy; IV amphotericin B or voriconazole are the preferred alternatives. These experts state that voriconazole offers little advantage over fluconazole and generally has been reserved for step-down oral therapy for treatment of C. krusei candidiasis or for treatment of fluconazole-resistant, voriconazole-susceptible C. glabrata infections. Although an echinocandin is preferred for initial treatment of C. glabrata infections, if the patient initially received fluconazole or voriconazole, continuation of the azole antifungal until treatment completion is reasonable if the patient is clinically improved and follow-up cultures are negative.
For treatment of candidemia in neutropenic† [off-label] patients, IDSA recommends an IV echinocandin (caspofungin, micafungin, anidulafungin) or IV amphotericin B for initial therapy; fluconazole is the preferred alternative in those who are less critically ill or have not recently received an azole; voriconazole can be used as an alternative when broader antifungal coverage is required. An echinocandin, amphotericin B, or voriconazole is recommended for C. krusei infections. An echinocandin is preferred for C. glabrata infections; fluconazole or amphotericin B is preferred for C. parapsilosis infections; an echinocandin, amphotericin B, or voriconazole is recommended for C. krusei infections. Although an echinocandin is preferred for initial treatment of C. glabrata infections, if the patient initially received fluconazole or voriconazole, continuation of the azole antifungal until treatment completion is reasonable if the patient is clinically improved and follow-up culture results are negative. For initial empiric treatment of suspected invasive candidiasis in neutropenic† [off-label] patients, amphotericin B, caspofungin, or IV voriconazole is recommended; alternatives are fluconazole or itraconazole.
Has been used prophylactically to reduce the incidence of candidiasis in patients at risk, including hematopoietic stem cell transplant recipients† [off-label].
Oropharyngeal Candidiasis
Treatment of oropharyngeal candidiasis† [off-label] refractory to other antifungals.
IDSA recommends topical treatment with clotrimazole lozenges or nystatin oral suspension for mild oropharyngeal candidiasis; oral fluconazole is recommended for moderate to severe disease. For refractory oropharyngeal candidiasis, including fluconazole-refractory infections, itraconazole oral solution, oral posaconazole, or oral voriconazole is recommended. An IV echinocandin (caspofungin, micafungin, anidulafungin) or IV amphotericin B also are recommended as alternatives for refractory infections.
For HIV-infected adults and adolescents with oropharyngeal candidiasis, CDC, NIH, and IDSA recommend oral fluconazole as drug of choice for treatment of initial episodes; if topical therapy used for treatment of mild to moderate episodes, drugs of choice are miconazole buccal tablets or clotrimazole lozenges. Alternatives for systemic treatment are itraconazole oral solution or oral posaconazole; alternative for topical treatment is nystatin oral suspension. For fluconazole-refractory oropharyngeal infections in HIV-infected adults and adolescents, oral posaconazole is preferred; itraconazole oral solution is an alternative.
Although routine long-term suppressive or maintenance therapy (secondary prophylaxis) to prevent relapse or recurrence not usually recommended in patients adequately treated for oropharyngeal candidiasis, patients with frequent or severe recurrences (including HIV-infected adults, adolescents, and children) may benefit from secondary prophylaxis with oral fluconazole or itraconazole oral solution; however, the potential for azole resistance should be considered. Patients with fluconazole-refractory oropharyngeal candidiasis who responded to treatment with an echinocandin should receive voriconazole or posaconazole for secondary prophylaxis until antiretroviral therapy produces immune reconstitution.
Esophageal Candidiasis
Treatment of esophageal candidiasis. Has been effective in immunocompromised patients with esophageal candidiasis caused by C. albicans, C. glabrata, or C. krusei.
Esophageal candidiasis requires treatment with a systemic antifungal (not a topical antifungal).
IDSA recommends oral fluconazole as the preferred drug of choice for treatment of esophageal candidiasis; if oral therapy is not tolerated, IV fluconazole, IV amphotericin B, or an IV echinocandin (caspofungin, micafungin, anidulafungin) is recommended. For fluconazole-refractory infections, preferred alternatives are itraconazole oral solution, oral posaconazole, or oral or IV voriconazole; other alternatives are an IV echinocandin or IV amphotericin B.
For HIV-infected adults and adolescents with esophageal candidiasis, CDC, NIH, and IDSA recommend oral or IV fluconazole as drug of choice for treatment and itraconazole oral solution as the preferred alternative. Other alternatives include an IV echinocandin (caspofungin, micafungin, anidulafungin), oral or IV voriconazole, oral posaconazole, or IV amphotericin B. For refractory esophageal candidiasis in HIV-infected adults and adolescents, including fluconazole-refractory infections, itraconazole oral solution or oral posaconazole is preferred; alternatives including IV amphotericin B, an IV echinocandin (caspofungin, micafungin, anidulafungin), or oral or IV voriconazole.
Although long-term suppressive or maintenance therapy (secondary prophylaxis) to prevent relapse or recurrence not usually recommended in patients adequately treated for esophageal candidiasis, patients with frequent or severe recurrences (including HIV-infected adults, adolescents, and children) may benefit from secondary prophylaxis with oral fluconazole or oral posaconazole; however, the potential for azole resistance should be considered. Patients with fluconazole-refractory esophageal candidiasis who responded to treatment with an echinocandin should receive voriconazole or posaconazole for secondary prophylaxis until antiretroviral therapy produces immune reconstitution.
Coccidioidomycosis
Has been used for treatment of coccidioidomycosis† caused by Coccidioides immitis or C. posadasii.
Antifungal treatment may not be necessary for mild, uncomplicated coccidioidal pneumonia since such infections may resolve spontaneously; treatment recommended for patients with more severe or rapidly progressing infections, those with chronic pulmonary or disseminated infections, and immunocompromised or debilitated individuals (e.g., HIV-infected individuals, organ transplant recipients, those receiving immunosuppressive therapy, those with diabetes or cardiopulmonary disease).
For HIV-infected adults and adolescents with clinically mild coccidioidomycosis (e.g., focal pneumonia), CDC, NIH, and IDSA recommend oral fluconazole or oral itraconazole for initial treatment; although data are limited, oral voriconazole or oral posaconazole are alternatives if there is no response to fluconazole or itraconazole.
Long-term suppressive or maintenance therapy (secondary prophylaxis) with oral fluconazole or oral itraconazole recommended to prevent relapse or recurrence of coccidioidomycosis in HIV-infected individuals who have been adequately treated for the disease; voriconazole or posaconazole are alternatives if patient did not initially respond to fluconazole or itraconazole.
Exserohilum Infections
Treatment of infections known or suspected to be caused by Exserohilum rostratum†.
Exserohilum, a common mold found in soil and on plants (especially grasses), is rarely involved in human infections. E. rostratum has caused cutaneous and subcutaneous infections or keratitis, typically from skin or eye trauma; also has rarely caused more invasive or life-threatening infections (e.g., sinuses, heart, lungs, bones), usually in immunocompromised individuals. Exserohilum infections cannot be transmitted person-to-person.
Although data limited and clinical relevance of in vitro testing remains uncertain, Exserohilum is inhibited in vitro by some triazole antifungals (e.g., voriconazole, itraconazole, posaconazole) and amphotericin B; echinocandins (e.g., caspofungin, micafungin) have variable in vitro activity and fluconazole has poor in vitro activity against the fungus.
E. rostratum was the predominant pathogen in the 2012–2013 US outbreak of fungal meningitis and other fungal infections in patients who received contaminated preservative-free methylprednisolone acetate injections prepared by a compounding pharmacy (New England Compounding Center [NECC]).
As of September 6, 2013, total of 750 cases of fungal infections (including 64 deaths) reported in 20 states and linked to 3 lots of contaminated methylprednisolone acetate injections. Majority of initial cases involved fungal meningitis (some with stroke); subsequent reports involved localized spinal or paraspinal infections (e.g., epidural abscess). More than 6 months after the outbreak, CDC continued to receive reports of patients presenting with localized spinal and paraspinal infections (e.g., epidural abscess, phlegmon, discitis, vertebral osteomyelitis, arachnoiditis, or other complications at or near the injection site). Localized infections have occurred in patients with or without a diagnosis of fungal meningitis.
Consultation with an infectious disease expert recommended to assist with diagnosis, management, and follow-up, which may be complex and prolonged. Clinical consultant network for clinicians can be reached by calling CDC at 800-232-4636.
Because of evidence of latent disease, CDC cautions clinicians to maintain high index of suspicion and remain vigilant for fungal infections in patients who received the contaminated products (especially in those who have mild or baseline symptoms) and to consider MRI evaluation for localized infections if clinically warranted.
Consult most recent CDC treatment guidance documents ([Web]) for the most current recommendations for selection of antifungal agents and appropriate dosages and duration of treatment for CNS and parameningeal infections and osteoarticular infections associated with the contaminated methylprednisolone acetate products. The following information was current when the voriconazole monograph was finalized for publication.
For treatment of CNS infections (including meningitis, stroke, and arachnoiditis) and/or parameningeal infections (epidural or paraspinal abscess, discitis or osteomyelitis, and sacroiliac infection) in adults who received contaminated methylprednisolone acetate injections, CDC recommends voriconazole. In most of these patients, use IV voriconazole initially; consider transitioning to oral voriconazole only after patient is clinically stable or improving and consider initial treatment with oral voriconazole only in those with mild disease who can be monitored closely. Strongly consider use of IV amphotericin B liposomal in addition to IV voriconazole in patients who present with severe disease and in those who do not improve or experience clinical deterioration or manifest new sites of disease activity while receiving voriconazole monotherapy. IV amphotericin B liposomal also is an alternative in patients unable to tolerate voriconazole. Although posaconazole or itraconazole has been used in some patients who could not tolerate voriconazole or amphotericin B, efficacy for treatment of these fungal infections not established; expert consultation advised when making decisions regarding alternative regimens.
For treatment of osteoarticular infections (discitis, vertebral osteomyelitis, and epidural abscess or osteoarticular infections not involving the spine) in adults who received intra-articular injections of contaminated methylprednisolone acetate injections, CDC recommends voriconazole. Use IV voriconazole initially in those with more severe osteoarticular infections, clinical instability, discitis, vertebral osteomyelitis, or epidural abscess; consider transitioning to oral voriconazole only after patient is clinically stable or improving and consider initial treatment with oral voriconazole only in patients with mild osteoarticular infections not involving the spine who can be monitored closely. Consider use of a lipid formulation of IV amphotericin B in addition to IV voriconazole in patients with severe osteoarticular infection and/or clinical instability. A lipid formulation of IV amphotericin B, posaconazole, or itraconazole are alternatives in patients who cannot tolerate voriconazole; expert consultation advised when making decisions regarding alternative regimens.
Adequate duration of antifungal treatment for these Exserohilum infections not known, but prolonged therapy (at least 3–6 months) required. (See Exserohilum Infections under Dosage and Administration.) Close follow-up monitoring after completion of treatment is essential in all patients to detect potential relapse.
Consult CDC website at [Web] and FDA website at for most recent information. CDC website includes information regarding case definitions and diagnostic testing as well as management and treatment of these infections.
Fusarium and Scedosporium infections
Treatment of serious Fusarium (including F. solani) or Scedosporium apiospermum (asexual form of Pseudallescheria boydii) infections in patients intolerant of, or whose disease is refractory to, other antifungals.
Select most appropriate antifungal based on in vitro susceptibility testing. Amphotericin B may be preferred for infections caused by F. solani or F. verticillioides; either voriconazole or amphotericin B recommended for other Fusarium infections.
For treatment of scedosporiosis, some clinicians consider voriconazole the drug of choice and posaconazole the preferred alternative.
Histoplasmosis
Has been used for treatment of histoplasmosis† caused by Histoplasma capsulatum.
For HIV-infected adults and adolescents with less severe disseminated histoplasmosis, CDC, NIH, and IDSA recommend initial treatment with oral itraconazole; although clinical data are limited, voriconazole or posaconazole may be used as alternatives for treatment of less severe histoplasmosis† in those intolerant of itraconazole who are only moderately ill.
Long-term suppressive or maintenance therapy (secondary prophylaxis) with itraconazole recommended to prevent recurrence or relapse in HIV-infected individuals who have been adequately treated for histoplasmosis. Role of voriconazole for secondary prophylaxis not evaluated to date.
Penicilliosis
Has been used for treatment of penicilliosis† caused by Penicillium marneffei.
For HIV-infected adults and adolescents with severe acute penicilliosis, CDC, NIH, and IDSA recommend treatment with IV amphotericin B liposomal initially followed by oral itraconazole. Voriconazole is an alternative, and may be used in those who do not respond to amphotericin B followed by itraconazole.
For HIV-infected adults and adolescents with mild penicilliosis†, CDC, NIH, and IDSA recommend itraconazole as drug of choice for treatment and voriconazole as an alternative.
Long-term suppressive or maintenance therapy (secondary prophylaxis) with itraconazole recommended to prevent recurrence or relapse in HIV-infected individuals who were treated for penicilliosis. An optimal voriconazole regimen for secondary prophylaxis of penicilliosis not identified to date.
Empiric Therapy in Febrile Neutropenic Patients
Has been used for empiric therapy of presumed fungal infections in febrile neutropenic patients†.
Voriconazole Dosage and Administration
Administration
Administer orally or by slow IV infusion.
IV route used for initial treatment of systemic fungal infections; oral route may replace IV when clinically indicated.
Correct electrolyte disturbances (e.g., hypokalemia, hypomagnesemia, hypocalcemia) prior to initiation of voriconazole. (See IV Infusion under Dosage and Administration and see Cardiovascular Effects under Cautions.)
Oral Administration
Administer orally at least 1 hour before or 1 hour after a meal.
Prior to withdrawal of each dose, shake reconstituted oral suspension for approximately 10 seconds. Administer using the oral dispenser supplied by the manufacturer.
If a dose is missed, take the missed dose as soon as possible; however, if it has been >6 hours since the missed dose, take the next scheduled dose at the appropriate time. Do not take a double dose.
Reconstitution
Reconstitute powder for oral suspension by adding 46 mL of water to the bottle containing 45 g to provide a suspension containing 40 mg/mL. Shake closed bottle vigorously for about 1 minute.
Do not mix oral suspension with other drugs or additional flavoring agents; do not dilute reconstituted suspension further with water or other vehicles.
IV Infusion
Do not administer voriconazole IV solutions concomitantly with short-term infusions of concentrated electrolytes, even if the 2 infusions are running in separate IV lines or cannulas. Voriconazole IV solutions may be administered at the same time as other IV solutions containing nonconcentrated electrolytes; however, the drug must be infused through a separate line.
Do not administer voriconazole IV solutions concomitantly with any blood product, even if the 2 infusions are running in separate IV lines or cannulas.
Voriconazole IV solutions may be administered at the same time as total parenteral nutrition (TPN); however, the drug must be infused through a separate line. If infused through a multiple-lumen catheter, TPN must be administered using a different port from the one used for voriconazole.
Reconstitution and Dilution
Reconstitute single-use 200-mg vial with exactly 19 mL of sterile water for injection to provide a solution containing 10 mg/mL. The vial should be shaken until all powder is dissolved.
Reconstituted solution must be further diluted in a compatible IV infusion solution prior to administration.
Calculate the volume of reconstituted solution required to administer the appropriate weight-based dose; withdraw and discard a volume of diluent from the final infusion container that equals or exceeds that volume. Withdraw appropriate dose from the required number of vials and add to the infusion container. Final concentration should be ≥0.5 mg/mL but ≤5 mg/mL. Discard any unused portion of reconstituted solution.
Rate of Administration
Administer by IV infusion over 1–2 hours at a maximum rate of 3 mg/kg per hour. Do not administer by rapid IV infusion.
Dosage
Pediatric Patients
Treatment of Aspergillosis
Oral
Children ≥12 years of age weighing <40 kg: Loading dose of 200 mg every 12 hours for 2 doses, then maintenance dosage of 100 mg every 12 hours has been recommended; if response is inadequate, may be increased to 150 mg every 12 hours.
Children ≥12 years of age weighing ≥40 kg: Loading dose of 400 mg every 12 hours for 2 doses, then maintenance dosage of 200 mg every 12 hours has been recommended; if response is inadequate, may be increased to 300 mg every 12 hours.
Duration of treatment is based on severity of underlying disease, recovery from immunosuppression, and response to the drug. IDSA recommends treatment of invasive pulmonary aspergillosis be continued for at least 6–12 weeks and continued throughout the period of immunosuppression.
HIV-infected children†: 8 mg/kg (maximum 400 mg) twice daily on day 1, followed by maintenance dosage of 7 mg/kg (maximum 200 mg) twice daily has been recommended. Continue treatment for ≥12 weeks; individualize treatment duration according to clinical response.
IV
Children ≥12 years of age: Loading dose regimen of 6 mg/kg every 12 hours for 2 doses, followed by IV maintenance regimen of 4 mg/kg every 12 hours has been recommended. Decrease IV maintenance dosage to 3 mg/kg every 12 hours if higher dosage not tolerated.
IDSA recommends that pediatric patients receive 5–7 mg/kg every 12 hours.
Switch to oral maintenance when clinically indicated. Total duration of treatment is based on severity of underlying disease, recovery from immunosuppression, and response to the drug.
HIV-infected children†: Loading dose regimen of 6–8 mg/kg twice daily on day 1, followed by IV maintenance dosage of 7 mg/kg (maximum 200 mg) twice daily has been recommended. Continue treatment for ≥12 weeks; individualize treatment duration according to clinical response.
HIV-infected adolescents: Loading dose regimen of 6 mg/kg twice daily on day 1, followed by IV maintenance dosage of 4 mg/kg twice daily. After clinical improvement, switch to an oral regimen of 200 mg twice daily. Optimal duration of therapy not established; continue antifungal therapy at least until CD4+ T-cells increase to 200/mm3 as a result of potent antiretroviral therapy and there is evidence of clinical response.
Candida Infections
Treatment of Candidemia and Disseminated Candida Infections
OralChildren ≥12 years of age weighing <40 kg: Loading dose of 200 mg every 12 hours for 2 doses, then maintenance dosage of 100 mg every 12 hours has been recommended; if response is inadequate, may be increased to 150 mg every 12 hours.
Children ≥12 years of age weighing ≥40 kg: Loading dose of 400 mg every 12 hours for 2 doses, then maintenance dosage of 200 mg every 12 hours has been recommended; if response is inadequate, may be increased to 300 mg every 12 hours.
Manufacturer recommends that treatment be continued for at least 14 days after symptoms resolve or the last positive culture, whichever is longer. IDSA and others recommend that antifungal treatment for candidemia (without persistent fungemia or metastatic complications) be continued for 14 days after first negative blood culture and resolutions of signs and symptoms of candidemia.
IVChildren ≥12 years of age: Loading dose regimen of 6 mg/kg every 12 hours for 2 doses, followed by IV maintenance regimen of 4 mg/kg every 12 hours has been recommended. Decrease IV maintenance dosage to 3 mg/kg every 12 hours if higher dosage not tolerated.
Manufacturer recommends that treatment be continued for at least 14 days after symptoms resolve or the last positive culture, whichever is longer. IDSA and others recommend that antifungal treatment for candidemia (without persistent fungemia or metastatic complications) be continued for 14 days after first negative blood culture and resolution of signs and symptoms of candidemia.
Treatment of Oropharyngeal Candidiasis†
OralChildren 2 through 11 years of age†: 200 mg twice daily (without loading dose) has been recommended.
Treatment of Esophageal Candidiasis
OralChildren ≥12 years of age weighing <40 kg: 100 mg every 12 hours has been recommended.
Children ≥12 years of age weighing ≥40 kg: 200 mg every 12 hours has been recommended.
HIV-infected adolescents: 200 mg twice daily.
Manufacturer recommends that treatment be continued for at least 14 days and for at least 7 days after symptoms resolve. IDSA and others recommend a treatment duration of 14–21 days.
IVHIV-infected adolescents: 200 mg twice daily.
Manufacturer recommends that treatment be continued for at least 14 days and for at least 7 days after symptoms resolve. IDSA and others recommend a treatment duration of 14–21 days.
Coccidioidomycosis†
Treatment of Clinically Mild Coccidioidomycosis†
OralHIV-infected adolescents: 200 mg twice daily recommended by CDC, NIH, and IDSA.
Prevention of Recurrence (Secondary Prophylaxis) of Coccidioidomycosis†
OralHIV-infected adolescents who have completed initial treatment: 200 mg twice daily recommended by CDC, NIH, and IDSA.
In HIV-infected patients who were treated for focal coccidioidal pneumonia and are receiving effective antiretroviral therapy, can consider discontinuing secondary prophylaxis against coccidioidomycosis after 12 months if CD4+ T-cells ≥250/mm3, provided patient is monitored for recurrence (e.g., serial chest radiographs, coccidioidal serology).
HIV-infected patients who were treated for diffuse pulmonary, disseminated, or meningeal coccidioidomycosis usually require life-long secondary prophylaxis.
Fusarium and Scedosporium Infections
Treatment of Fusarium and Scedosporium Infections
OralChildren ≥12 years of age weighing <40 kg: Loading dose of 200 mg every 12 hours for 2 doses, then maintenance dosage of 100 mg every 12 hours has been recommended; if response is inadequate, may be increased to 150 mg every 12 hours.
Children ≥12 years of age weighing ≥40 kg: Loading dose of 400 mg every 12 hours for 2 doses, then maintenance dosage of 200 mg every 12 hours has been recommended; if response is inadequate, may be increased to 300 mg every 12 hours.
Duration of treatment is based on severity of underlying disease, recovery from immunosuppression, and response to the drug.
IVChildren ≥12 years of age: Loading dose regimen of 6 mg/kg every 12 hours for 2 doses, followed by IV maintenance regimen of 4 mg/kg every 12 hours has been recommended. Decrease IV maintenance dosage to 3 mg/kg every 12 hours if higher dosage not tolerated.
Duration of treatment is based on severity of underlying disease, recovery from immunosuppression, and response to the drug.
Histoplasmosis†
Treatment of Less Severe Disseminated Histoplasmosis†
OralHIV-infected adolescents who are only moderately ill: 400 mg twice daily for 2 doses, then 200 mg twice daily recommended by CDC, NIH, and IDSA.
Penicilliosis†
Treatment of Severe Penicilliosis†
IV, then OralHIV-infected adolescents: 6 mg/kg IV every 12 hours for 2 doses followed by 4 mg/kg every 12 hours for at least 3 days, then 200 mg orally twice daily for maximum of 12 weeks recommended by CDC, NIH, and IDSA.
Treatment of Mild Penicilliosis†
OralHIV-infected adolescents: 400 mg twice daily for 2 doses, then 200 mg twice daily for maximum of 12 weeks recommended by CDC, NIH, and IDSA.
Adults
Oral dosage of 200 mg every 12 hours results in AUC similar to that achieved with IV dosage of 3 mg/kg every 12 hours; oral dosage of 300 mg every 12 hours results in AUC similar to that reported with IV dosage of 4 mg/kg every 12 hours.
Treatment of Aspergillosis
Oral
Adults weighing <40 kg: After initial IV regimen, maintenance dosage of 100 mg every 12 hours; if response is inadequate, increase to 150 mg every 12 hours. If not tolerated, decrease dosage by increments of 50 mg to a minimum of 100 mg every 12 hours.
Adults weighing ≥40 kg: After initial IV regimen, maintenance dosage of 200 mg every 12 hours; if response is inadequate, increase to 300 mg every 12 hours. If not tolerated, decrease dosage by increments of 50 mg to a minimum of 200 mg every 12 hours.
Duration of treatment is based on severity of underlying disease, recovery from immunosuppression, and response to the drug. In a clinical study, median duration of initial IV therapy was 10 days (range 2–90 days) and median duration of maintenance oral therapy was 76 days (range 2–232 days). IDSA recommends treatment of invasive pulmonary aspergillosis be continued for at least 6–12 weeks and continued throughout the period of immunosuppression.
IV
Loading dose regimen of 6 mg/kg every 12 hours for 2 doses, followed by IV maintenance regimen of 4 mg/kg every 12 hours. Decrease IV maintenance dosage to 3 mg/kg every 12 hours if higher dosage not tolerated. Continue IV regimen for at least 7 days until clinically stable before switching to oral voriconazole.
HIV-infected adults and adolescents: Loading dose regimen of 6 mg/kg every 12 hours on day 1, followed by IV maintenance regimen of 4 mg/kg every 12 hours. After clinical improvement, switch to oral regimen of 200 mg every 12 hours. Optimal duration of therapy not established; continue antifungal therapy at least until CD4+ T-cells increase to 200/mm3 as a result of potent antiretroviral therapy and there is evidence of clinical response.
Candida Infections
Treatment of Candidemia and Disseminated infections
OralAdults weighing <40 kg: After initial IV regimen, maintenance dosage of 100 mg every 12 hours; if response is inadequate, increase to 150 mg every 12 hours. If not tolerated, decrease dosage by increments of 50 mg to a minimum of 100 mg every 12 hours.
Adults weighing ≥40 kg: After initial IV regimen, maintenance dosage of 200 mg every 12 hours; if response is inadequate, increase to 300 mg every 12 hours. If not tolerated, decrease dosage by increments of 50 mg to a minimum of 200 mg every 12 hours.
Manufacturer recommends that treatment be continued for at least 14 days after symptoms resolve or the last positive culture, whichever is longer. IDSA and others recommend that antifungal treatment for candidemia (without persistent fungemia or metastatic complications) be continued for 14 days after first negative blood culture and resolution of signs and symptoms of candidemia.
IVLoading dose regimen of 6 mg/kg every 12 hours for 2 doses, followed by IV maintenance regimen of 3–4 mg/kg every 12 hours. Decrease IV maintenance dosage to 3 mg/kg every 12 hours if higher dosage not tolerated.
In clinical studies, patients with candidemia received 3 mg/kg every 12 hours and those with deep tissue infections received 4 mg/kg every 12 hours as salvage therapy.
Switch to oral maintenance when clinically indicated.
Manufacturer recommends that treatment be continued for at least 14 days after symptoms resolve or the last positive culture, whichever is longer. IDSA and others recommend antifungal treatment for candidemia (without persistent fungemia or metastatic complications) be continued for 14 days after first negative blood culture and resolution of signs and symptoms of candidemia.
Treatment of Oropharyngeal Candidiasis†
Oral200 mg twice daily.
IDSA and others recommend a treatment duration of 7–14 days.
Treatment of Esophageal Candidiasis
OralAdults weighing <40 kg: 100 mg every 12 hours.
Adults weighing ≥40 kg: 200 mg every 12 hours.
HIV-infected adults: 200 mg twice daily.
Manufacturer recommends that treatment be continued for at least 14 days and for at least 7 days after symptoms resolve. IDSA and others recommend a treatment duration of 14–21 days.
IVHIV-infected adults: 200 mg twice daily.
Manufacturer recommends that treatment be continued for at least 14 days and for at least 7 days after symptoms resolve. IDSA and others recommend a treatment duration of 14–21 days.
Coccidioidomycosis†
Treatment of Clinically Mild Coccidioidomycosis†
OralHIV-infected adults: 200 mg twice daily recommended by CDC, NIH, and IDSA.
Prevention of Recurrence (Secondary Prophylaxis) of Coccidioidomycosis†
OralHIV-infected adults who have completed initial treatment: 200 mg twice daily recommended by CDC, NIH, and IDSA.
In HIV-infected patients who were treated for focal coccidioidal pneumonia and are receiving effective antiretroviral therapy, can consider discontinuing secondary prophylaxis against coccidioidomycosis after 12 months if CD4+ T-cells ≥250/mm3, provided patient is monitored for recurrence (e.g., serial chest radiographs, coccidioidal serology).
HIV-infected patients who were treated for diffuse pulmonary, disseminated, or meningeal coccidioidomycosis usually require life-long secondary prophylaxis.
Exserohilum Infections†
Treatment of Known or Suspected Exserohilum Infections†
IV or OralCNS and/or parameningeal infections: CDC recommends 6 mg/kg every 12 hours. Give IV initially in most patients; consider switching to oral route only after patient is clinically stable or improving. Consider initial oral treatment only in those with mild disease who can be monitored closely.
Osteoarticular infections: CDC recommends 6 mg/kg every 12 hours. For osteoarticular infections not involving the spine, consider 6 mg/kg every 12 hours for 2 doses, followed by 4 mg/kg every 12 hours. Give IV initially in most patients; consider switching to oral route only after patient is clinically stable or improving.
In all patients, measure serum voriconazole concentrations on treatment day 5 and adjust dosage if needed, aiming for trough concentrations of 2–5 mcg/mL. Monitor serum concentrations once weekly during initial 4–6 weeks of treatment and when dosage changes are made, maintaining trough voriconazole concentrations of 2–5 mcg/mL. Avoid concentrations >5 mcg/mL because of risk of neurotoxicity and other adverse effects.
Adequate duration of antifungal treatment unknown; prolonged treatment required based on disease severity and clinical response.
In those with severe CNS disease with complications (arachnoiditis, stroke), persistent CSF abnormalities, or underlying immunosuppression, treatment duration of 6–12 months probably necessary. In those with parameningeal infection, consider minimum duration of 3–6 months (≥6 months for more severe disease such as discitis or osteomyelitis, underlying immunosuppression, or complications not amenable to surgical treatment).
In those with osteoarticular infections, consider minimum duration of 3 months (>3 months probably necessary for severe disease, bone infections, or underlying immunosuppression).
After treatment completion, close follow-up monitoring essential in all patients to detect potential relapse.
Consult infectious disease expert and most recent CDC guidelines for information regarding management. Consult CDC website at [Web] for most recent recommendations regarding drugs of choice, dosage, and duration of treatment.
Fusarium and Scedosporium Infections
Treatment of Fusarium and Scedosporium Infections
OralAdults weighing <40 kg: After initial IV regimen, maintenance dosage of 100 mg every 12 hours; if response is inadequate, increase to 150 mg every 12 hours. If not tolerated, decrease dosage by increments of 50 mg to a minimum of 100 mg every 12 hours.
Adults weighing ≥40 kg: After initial IV regimen, maintenance dosage of 200 mg every 12 hours; if response is inadequate, increase to 300 mg every 12 hours. If not tolerated, decrease dosage by increments of 50 mg to a minimum of 200 mg every 12 hours.
Duration of treatment is based on severity of underlying disease, recovery from immunosuppression, and response to the drug.
IVLoading dose regimen of 6 mg/kg every 12 hours for 2 doses, followed by IV maintenance regimen of 4 mg/kg every 12 hours. Decrease IV maintenance dosage to 3 mg/kg every 12 hours if higher dosage not tolerated.
Switch to oral maintenance when clinically indicated.
Duration of treatment is based on severity of underlying disease, recovery from immunosuppression, and response to the drug.
Histoplasmosis†
Treatment of Less Severe Disseminated Histoplasmosis†
OralHIV-infected adults who are only moderately ill: 400 mg twice daily for 2 doses, then 200 mg twice daily recommended by CDC, NIH, and IDSA.
Penicilliosis†
Treatment of Severe Penicilliosis†
IV, then OralHIV-infected adults: 6 mg/kg IV every 12 hours for 2 doses followed by 4 mg/kg IV every 12 hours for at least 3 days, then 200 mg orally twice daily for maximum of 12 weeks recommended by CDC, NIH, and IDSA.
Treatment of Mild Penicilliosis†
OralHIV-infected adults: 400 mg twice daily for 2 doses, then 200 mg twice daily for maximum of 12 weeks recommended by CDC, NIH, and IDSA.
Special Populations
Hepatic Impairment
Mild to moderate hepatic cirrhosis (Child-Pugh class A or B): Use usual loading dose regimen, but decrease maintenance dosages by 50%.
Severe hepatic impairment: Use only if benefits outweigh risks. Not studied in patients with severe cirrhosis (Child-Pugh class C) or chronic HBV or HCV infection. (See Hepatic Impairment under Cautions.)
Renal Impairment
Dosage adjustment of oral voriconazole not needed.
Moderate to severe renal impairment (Clcr <50 mL/minute): Use IV voriconazole only if possible benefits outweigh risks. (See Renal Impairment under Cautions.) Monitor serum creatinine closely; if increases occur, consider switching to oral voriconazole.
Geriatric Patients
Dosage adjustments not necessary based on age.
Concomitant Therapy with Efavirenz or Phenytoin
If used with efavirenz or phenytoin, voriconazole dosage adjustment recommended. (See Specific Drugs under Interactions.)
Cautions for Voriconazole
Contraindications
-
Known hypersensitivity to voriconazole or any ingredient in the formulation.
-
Concomitant use with astemizole or terfenadine (drugs no longer commercially available in US), carbamazepine, cisapride (currently commercially available in the US only under a limited-access protocol), ergot alkaloids (e.g., ergotamine, dihydroergotamine), pimozide, quinidine, rifabutin, rifampin, sirolimus, St. John's wort (Hypericum perforatum), or long-acting barbiturates (e.g., phenobarbital, mephobarbital). (See Specific Drugs under Interactions.)
-
Concomitant use with full-dose ritonavir (≥400 mg twice daily) is contraindicated; avoid concomitant use with low-dose ritonavir (100 mg every 12 hours) unless benefits outweigh risks. (See Specific Drugs under Interactions.)
Warnings/Precautions
Sensitivity Reactions
Hypersensitivity Reactions
Anaphylactoid reactions (e.g., flushing, fever, sweating, tachycardia, chest tightness, dyspnea, faintness, nausea, pruritus, rash) reported rarely immediately after initiation of voriconazole IV infusion. Consider stopping the infusion if these reactions occur.
Serious cutaneous reactions (e.g., Stevens-Johnson syndrome, erythema multiforme, toxic epidermal necrolysis) and photosensitivity reactions reported rarely. (See Dermatologic Effects under Cautions.)
Data regarding cross-sensitivity with other azole antifungals not available. Use with caution in patients hypersensitive to other azoles.
Hepatic Effects
Hepatitis, cholestasis, and fulminant hepatic failure reported rarely. Hepatic effects (including hepatitis and jaundice) have occurred in patients with no identifiable risk factors. Hepatic effects usually are reversible when voriconazole discontinued, but fatalities have occurred.
Perform liver function tests prior to and during voriconazole therapy.
If abnormal liver function tests occur during therapy, monitor for development of more severe hepatic injury using appropriate laboratory evaluations (particularly liver function tests and bilirubin). Consider discontinuing voriconazole if clinical signs and symptoms consistent with liver disease develop that may be attributable to the drug.
Ocular Effects
Visual disturbances (e.g., abnormal vision, blurred vision, color vision change, photophobia) reported; may be related to high dosage and high plasma voriconazole concentrations.
Postmarketing reports of prolonged visual disturbances, including optic neuritis and papilledema.
Effect on visual function unknown if duration of therapy is >28 days. Monitor visual function (visual acuity, visual field, and color perception) if duration is >28 days.
Fetal/Neonatal Morbidity and Mortality
May cause fetal harm; teratogenicity demonstrated in animals. (See Pregnancy under Cautions.)
Pregnancy should be avoided. Women of childbearing potential should use effective contraception during voriconazole treatment. (See Specific Drugs under Interactions.)
If used during pregnancy or if patient becomes pregnant while receiving voriconazole, advise patient of the potential hazard to the fetus.
Fructose or Galactose Intolerance
Voriconazole tablets contain lactose and should not be used in those with galactose intolerance, Lapp lactase deficiency, or glucose-galactose malabsorption.
Voriconazole oral suspension contains sucrose and should not be used in those with fructose intolerance, sucrase-isomaltase deficiency, or glucose-galactose malabsorption.
Cardiovascular Effects
Prolonged QT interval reported with voriconazole and other azoles. Arrhythmias (e.g., torsades de pointes), cardiac arrest, and sudden death reported rarely.
Most reported cases involved seriously ill patients with multiple confounding risk factors that may have contributed (e.g., history of cardiotoxic chemotherapy, cardiomyopathy, hypokalemia, concomitant drugs).
Use with caution in patients with potentially proarrhythmic conditions.
Rigorous attempts should be made to correct potassium, magnesium, and calcium before starting voriconazole.
Laboratory Monitoring
Evaluate liver function (e.g., liver function tests, bilirubin) prior to and during voriconazole therapy.
Evaluate serum electrolytes (i.e., potassium, magnesium, calcium) and correct any abnormalities prior to initiating therapy.
Monitor renal function (e.g., Serum creatinine) during voriconazole therapy.
Monitor patients who have risk factors for acute pancreatitis (e.g., recent chemotherapy, hematopoietic stem cell transplantation [HSCT]) for the development of pancreatitis.
Dermatologic Effects
Serious exfoliative cutaneous reactions (e.g., Stevens-Johnson syndrome, erythema multiforme, toxic epidermal necrolysis) reported rarely. If an exfoliative cutaneous reaction occurs, discontinue voriconazole.
Photosensitivity skin reactions reported. Avoid intense or prolonged exposure to direct sunlight during voriconazole therapy.
Squamous cell carcinoma of the skin and melanoma have been reported during long-term voriconazole therapy in patients with photosensitivity reactions. If skin lesion consistent with squamous cell carcinoma or melanoma develops, discontinue voriconazole.
Renal Effects
Acute renal failure reported in severely ill patients with other factors predisposing to impaired renal function (e.g., underlying conditions, concomitant nephrotoxic drugs).
Skeletal Effects
Fluorosis and periostitis reported during long-term therapy. If skeletal pain and radiologic findings compatible with fluorosis or periostitis occur, discontinue voriconazole.
Specific Populations
Pregnancy
Category D. (See Fetal/Neonatal Morbidity and Mortality under Cautions.)
Do not use during pregnancy except when benefits for the mother clearly outweigh potential risks for the fetus.
In animal studies, teratogenic effects (cleft palate, hydronephrosis/hydroureter) and embryotoxic effects reported.
Lactation
Not known whether distributed into milk. Discontinue nursing or the drug.
Pediatric Use
Safety and efficacy not established in children <12 years of age.
Has been recommended for treatment of fungal infections in children. Some clinicians consider voriconazole the drug of choice for treatment of invasive aspergillosis in HIV-infected children†, but state that data are insufficient to recommend use of the drug for treatment of candidemia or esophageal candidiasis in these children.
Has been used in children 9 months to 15 years of age† in clinical studies.
Adverse effects in pediatric patients similar to those reported in adults.
Cases of pancreatitis in pediatric patients documented in postmarketing reports; monitor for the development of pancreatitis in children with risk factors for acute pancreatitis (e.g., recent chemotherapy, HSCT).
Geriatric Use
Plasma voriconazole concentrations increased in geriatric patients, but overall safety profile is similar to that in younger adults.
Hepatic Impairment
Monitor carefully for adverse effects, including adverse hepatic effects. (See Hepatic Effects under Cautions.)
Not evaluated in patients with severe hepatic cirrhosis (Child-Pugh class C) or with HBV or HCV infection.
Not recommended in patients with severe hepatic impairment unless potential benefits outweigh risks.
Renal Impairment
IV voriconazole contains sulfobutyl ether β-cyclodextrin sodium (SBECD) which may accumulate in patients with moderate-to-severe renal impairment (Clcr <50 mL/minute).
IV voriconazole should not be used in patients with Clcr <50 mL/minute, unless potential benefits outweigh risks. If IV voriconazole is used in these patients, monitor serum creatinine concentrations closely; if increases occur, consider switching to oral voriconazole.
Common Adverse Effects
Visual disturbances (abnormal vision, blurred vision, color vision change, photophobia), GI effects (nausea, vomiting, diarrhea, abdominal pain), fever, rash, chills, headache, abnormalities in liver function test results, tachycardia, hallucinations.
Drug Interactions
Metabolized by CYP2C9, 2C19, and 3A4.
Inhibits CYP2C9, 2C19, and 3A4; the major metabolite (voriconazole N-oxide) also inhibits these enzymes. Voriconazole appears to be a less potent inhibitor of CYP3A4 than some other azoles (e.g., itraconazole, ketoconazole).
Drugs Affecting or Metabolized by Hepatic Microsomal Enzymes
Potential pharmacokinetic interactions with drugs that are inhibitors, inducers, or substrates of CYP2C9, 2C19, or 3A4 with possible alteration in metabolism of voriconazole and/or other drug.
Specific Drugs
|
Drug |
Interaction |
Comments |
|---|---|---|
|
Alfentanil |
Increased mean AUC and elimination half-life of alfentanil when administered with voriconazole and naloxone Increased incidence of delayed and persistent alfentanil-induced nausea and vomiting when administered with voriconazole |
If voriconazole used concomitantly with alfentanil or other opiate agonist metabolized by CYP3A4 (e.g., sufentanil), reduced dosage of the opiate agonist may be necessary Extended close monitoring for opiate-related adverse events (e.g., respiratory depression) may be necessary |
|
Anticoagulants, oral (warfarin) |
Potentiates warfarin’s effect on PT |
Monitor PT or other appropriate tests closely if used with warfarin; reduce anticoagulant dosage if necessary |
|
Antidiabetic agents, sulfonylureas (glipizide, glyburide, tolbutamide) |
Possible increased concentrations of glipizide, glyburide, tolbutamide and risk of hypoglycemia |
Monitor blood glucose and observe patient for signs and symptoms of hypoglycemia; adjust dosage of antidiabetic agent as necessary |
|
Antihistamines (astemizole, terfenadine) |
Possible pharmacokinetic interaction and potential for serious or life-threatening reactions (e.g., cardiac arrhythmias) with astemizole or terfenadine (drugs no longer commercially available in the US) |
Concomitant use contraindicated |
|
Antimycobacterials, rifamycins (rifabutin, rifampin) |
Rifabutin: Decreased voriconazole concentrations and AUC and increased rifabutin concentrations and AUC Rifampin: Decreased voriconazole concentrations and AUC |
Concomitant use with rifabutin or rifampin contraindicated |
|
Antiretrovirals, HIV entry inhibitors |
Maraviroc: Possible increased maraviroc concentrations |
Maraviroc: Consider reducing maraviroc dosage to 150 mg twice daily |
|
Antiretrovirals, HIV integrase inhibitors |
Fixed combination of elvitegravir, cobicistat, emtricitabine, and tenofovir: Possible increased concentrations of voriconazole, elvitegravir, and/or cobicistat Raltegravir: Pharmacokinetic interaction unlikely |
Elvitegravir/cobicistat/emtricitabine/tenofovir: Avoid concomitant use unless potential benefits outweigh risks; if used concomitantly, consider monitoring voriconazole concentrations to guide dosage adjustments Raltegravir: Dosage adjustments not needed |
|
Antiretrovirals, HIV protease inhibitors (PIs) |
Possible pharmacokinetic interactions (altered PI and/or voriconazole concentrations) if voriconazole used in patients receiving PIs (e.g., atazanavir, darunavir, fosamprenavir, indinavir, lopinavir, nelfinavir, ritonavir, saquinavir, tipranavir), especially if ritonavir-boosted PI regimen used Indinavir: No clinically important effects on pharmacokinetics of voriconazole or indinavir; Indinavir (with low-dose ritonavir): Possible decreased voriconazole concentrations Ritonavir, full-dose (400 mg twice daily): Decreased voriconazole concentrations and AUC; no clinically important effect on ritonavir pharmacokinetics Ritonavir, low-dose (100 mg twice daily): Slightly decreased voriconazole concentrations and AUC, slightly decreased ritonavir concentrations and AUC |
Avoid concomitant use with ritonavir-boosted atazanavir, ritonavir-boosted darunavir, ritonavir-boosted fosamprenavir, ritonavir-boosted indinavir, lopinavir/ritonavir, ritonavir-boosted nelfinavir, ritonavir-boosted saquinavir, or ritonavir-boosted tipranavir unless benefits outweigh risks; if used concomitantly, consider monitoring voriconazole concentrations and adjust voriconazole dosage as needed Atazanavir: Monitor for voriconazole and atazanavir toxicity Fosamprenavir: Monitor for voriconazole and fosamprenavir toxicity Indinavir: Dosage adjustments not needed Nelfinavir: Monitor for voriconazole and nelfinavir toxicity Ritonavir, full-dose (400 mg twice daily): Concomitant use contraindicated Ritonavir, low-dose (100 mg twice daily): Concomitant use not recommended unless benefits outweigh risks; consider monitoring voriconazole concentrations Saquinavir: Monitor for voriconazole and saquinavir toxicity |
|
Antiretrovirals, nonnucleoside reverse transcriptase inhibitors (NNRTIs) |
Delavirdine: Increased voriconazole concentrations Efavirenz: Decreased voriconazole AUC, increased peak plasma voriconazole concentrations, and increased peak plasma efavirenz concentrations and AUC when voriconazole (400 mg every 12 hours) used concomitantly with efavirenz (300 mg daily) Etravirine: Possible increased voriconazole and etravirine concentrations Nevirapine: Possible decreased voriconazole concentrations, increased nevirapine concentrations Rilpivirine: Possible increased rilpivirine concentrations; effect on voriconazole concentrations unknown |
Delavirdine: Monitor for voriconazole toxicity and clinical response Efavirenz: Increase voriconazole maintenance dosage to 400 mg every 12 hours and decrease efavirenz dosage to 300 mg daily; when voriconazole is discontinued, initial dosage of efavirenz may be resumed Etravirine: Use concomitantly with caution; dosage adjustment not needed for either drug; some experts state consider monitoring voriconazole concentrations Nevirapine: Monitor for nevirapine toxicity and monitor clinical response to voriconazole and/or voriconazole plasma concentrations Rilpivirine: Dosage adjustments not needed; monitor for breakthrough fungal infections |
|
Barbiturates, long-acting (phenobarbital, mephobarbital) |
Possible decreased voriconazole concentrations with long-acting barbiturates and risk of prolonged sedative effects |
Concomitant use contraindicated |
|
Benzodiazepines (alprazolam, midazolam, triazolam) |
Possible increased benzodiazepine concentrations and AUC |
Monitor closely for manifestations of benzodiazepine toxicity; adjustment of benzodiazepine dosage may be needed |
|
Boceprevir |
Possible increased voriconazole concentrations |
|
|
Calcium-channel blocking agents |
Possible increased concentrations of calcium-channel blockers metabolized by CYP3A4 (e.g., felodipine) |
Monitor for toxicity; dosage adjustment of the calcium-channel blocker may be necessary |
|
Carbamazepine |
Possible decreased voriconazole concentrations |
Concomitant use contraindicated |
|
Cisapride (currently commercially available in US only under a limited access protocol) |
Possible pharmacokinetic interaction and potential for serious or life-threatening reactions (e.g., cardiac arrhythmias) |
Concomitant use contraindicated |
|
Clopidogrel |
Possible decreased plasma concentrations of the active metabolite of clopidogrel and reduced antiplatelet effects of clopidogrel |
Avoid concomitant use of clopidogrel and CYP2C19 inhibitors since clopidogrel is metabolized to its active metabolite by CYP2C19; in vitro studies indicate voriconazole inhibits CYP2C19 |
|
Corticosteroids (prednisolone) |
Increased concentration and AUC of prednisolone |
Dosage adjustments not needed |
|
Digoxin |
No clinically important effect on pharmacokinetics on digoxin |
Dosage adjustments not needed |
|
Ergot alkaloids (dihydroergotamine, ergonovine, ergotamine, methylergonovine) |
Possible increased ergot alkaloid plasma concentrations; potential for serious or life-threatening reactions (e.g., acute ergot toxicity) |
Concomitant use contraindicated |
|
Estrogens/Progestins |
Oral contraceptive containing ethinyl estradiol and norethindrone: Increased peak plasma concentrations and AUC of ethinyl estradiol and norethindrone, increased peak plasma concentrations and AUC of voriconazole |
Monitor for adverse effects of the oral contraceptives and voriconazole |
|
Fentanyl |
Decreased mean plasma clearance and increased AUC of IV fentanyl |
If voriconazole is used concomitantly with IV, oral, or transdermal fentanyl, extended and frequent monitoring for respiratory depression and other fentanyl-associated adverse effects is recommended, reduce fentanyl dosage if warranted |
|
Fluconazole |
Substantially increased voriconazole concentrations and AUC |
Avoid concomitant use; if voriconazole initiated ≤24 hours after last fluconazole dose, monitor for voriconazole adverse effects |
|
Histamine H2-receptor antagonists (cimetidine, ranitidine) |
Cimetidine: Possible increased voriconazole concentrations and AUC; not considered clinically important Ranitidine: No pharmacokinetic interaction |
Dosage adjustments not needed |
|
HMG-CoA reductase inhibitors |
Possible increased plasma concentrations of HMG-CoA reductase inhibitors metabolized by CYP3A4 (e.g., lovastatin) |
Monitor for manifestations of toxicity and adjust dosage of HMG-CoA reductase inhibitor as necessary |
|
Immunosuppressive agents (cyclosporine, sirolimus, tacrolimus) |
Cyclosporine: Increased cyclosporine concentrations and AUC Sirolimus: Increased sirolimus concentrations and AUC Tacrolimus: Increased tacrolimus concentrations |
Cyclosporine: Decrease cyclosporine dosage by 50% if initiating voriconazole; when voriconazole discontinued, monitor concentrations of the immunosuppressive agent and adjust dosage as necessary Sirolimus: Concomitant use contraindicated Tacrolimus: Decrease tacrolimus dosage by 33% if initiating voriconazole; when voriconazole discontinued, monitor concentrations of the immunosuppressive agent and adjust dosage as necessary |
|
Macrolides (azithromycin, erythromycin) |
No clinically important effects on pharmacokinetics of voriconazole when given with azithromycin or erythromycin |
Dosage adjustments not needed |
|
Methadone |
Increased peak plasma concentrations of R-methadone; risk of toxicity (QT prolongation) |
Monitor frequently for methadone toxicity; adjust methadone dosage if needed |
|
Mycophenolate |
No clinically important effect on pharmacokinetics of mycophenolate or its major metabolite |
Dosage adjustments not needed |
|
NSAIAs |
Diclofenac: Increased peak plasma diclofenac concentrations and AUC; clinical relevance unknown Ibuprofen: Increased ibuprofen AUC Celecoxib, naproxen, lornoxicam, meloxicam: Possible increased plasma concentrations of the NSAIA |
Diclofenac, ibuprofen: Reduced NSAIA dosage may be necessary; monitor closely for NSAIA-related adverse effects and toxicity Celecoxib, naproxen, lornoxicam, meloxicam: Monitor closely for NSAIA-related adverse effects and toxicity; reduce NSAIA dosage if warranted |
|
Oxycodone |
Increased peak plasma concentration, AUC, and elimination half-life of oxycodone; increased oxycodone-associated adverse visual effects (heterophoria, miosis) |
If used concomitantly, extended and frequent monitoring for oxycodone-associated adverse effects is recommended; reduced oxycodone dosage may be necessary to avoid opiate-related adverse effects |
|
Phenytoin |
Decreased voriconazole concentrations and AUC with voriconazole 200 mg every 12 hours; concomitant use of voriconazole 400 mg every 12 hours with phenytoin results in plasma voriconazole concentrations similar to those attained with voriconazole 200 mg every 12 hours given without phenytoin Increased plasma concentrations of phenytoin with voriconazole 400 mg every 12 hours |
If used concomitantly, increase voriconazole IV maintenance dosage to 5 mg/kg every 12 hours; increase voriconazole oral maintenance dosage to 400 mg every 12 hours in those weighing ≥40 kg or 200 mg every 12 hour in those weighing <40 kg Closely monitor phenytoin concentrations and observe patient for potential phenytoin adverse effects |
|
Pimozide |
Possible pharmacokinetic interaction and potential for serious or life-threatening reactions (e.g., cardiac arrhythmias) |
Concomitant use contraindicated |
|
Proton-pump inhibitors (omeprazole) |
Omeprazole: Increased omeprazole concentrations and AUC; slightly increased voriconazole concentrations and AUC; GI absorption of voriconazole not affected Possible pharmacokinetic interactions with other proton-pump inhibitors metabolized by CYP2C19 |
Omeprazole: In those receiving omeprazole dosages ≥40 mg daily, decrease omeprazole dosage by 50% if voriconazole is initiated; voriconazole dosage adjustment not necessary |
|
Quinidine |
Possible pharmacokinetic interaction and potential for serious or life-threatening reactions (e.g., cardiac arrhythmias) |
Concomitant use contraindicated |
|
St. John's wort (Hypericum perforatum) |
Decreased voriconazole AUC following multiple doses of St. John's wort; no clinically important effects on voriconazole AUC following single dose of St. John's wort |
Concomitant use contraindicated |
|
Telaprevir |
Possible altered voriconazole concentrations; possible increased telaprevir concentrations |
Use only if benefits justify risks; if used concomitantly, use caution and clinical monitoring |
|
Venlafaxine |
Increased venlafaxine AUC |
If used concomitantly, monitor for venlafaxine-associated toxicity |
|
Vinca alkaloids |
Possible increased concentrations of vinca alkaloids |
Monitor for manifestations of vinca alkaloid toxicity (neurotoxicity) and adjust dosage as necessary |
|
Zolpidem |
Increased peak plasma concentration and AUC of zolpidem and prolonged zolpidem half-life |
If used concomitantly, monitor for zolpidem-associated toxicity and adjust dosage as necessary |
Voriconazole Pharmacokinetics
Absorption
Bioavailability
Oral bioavailability estimated to be 96%. Following oral administration, peak plasma concentrations achieved within 1–2 hours.
In adults, the 200-mg tablet and 40-mg/mL oral suspension are bioequivalent when administered with a loading dose regimen (400 mg every 12 hours) followed by maintenance dosage (200 mg every 12 hours).
Food
When multiple doses are administered with a high-fat meal, mean peak plasma concentrations and extent of absorption are reduced by 34 and 24%, respectively.
Plasma Concentrations
Nonlinear pharmacokinetics because of saturation of its metabolism.
When recommended IV or oral loading dose regimens are administered in adults, peak plasma concentrations close to steady state are achieved within the first 24 hours of dosing. Without the loading dose regimen, steady-state concentrations are achieved within 5–7 days in adults.
Special Populations
Peak plasma concentrations and AUCs after oral or IV administration are higher in geriatric patients ≥65 years of age compared with younger adults.
In a population pharmacokinetic analysis of voriconazole concentrations in children 2 to <12 years of age who received various dosage regimens, AUCs achieved with IV dosage of 7 mg/kg twice daily or oral dosage of 200 mg twice daily (oral suspension) were comparable to AUCs observed in adults receiving usual voriconazole dosages. Data from this study also indicated that loading doses do not appear to reduce the length of time required to reach steady-state in children 2 to <12 years of age and appear to offer little benefit in this age group. Based on a comparison of pharmacokinetic data from pediatric patients (2 to <12 years of age) with data from adults, the manufacturer states that the predicted steady-state plasma voriconazole concentrations were similar in pediatric patients or adults (median concentration 1.19 or 1.16 mcg/mL, respectively) at a maintenance IV dosage of 4 mg/kg every 12 hours in children or 3 mg/kg every 12 hours in adults.
Distribution
Extent
Probably extensively distributed into tissues.
Not known whether distributed into milk.
Plasma Protein Binding
Approximately 58%.
Elimination
Metabolism
In vitro studies indicate voriconazole is metabolized by CYP2C9, 2C19, and 3A4. The major metabolite is the N-oxide, which has minimal antifungal activity.
Elimination Route
After initial load dosage regimen, 80–83% of an oral or IV dose is eliminated in urine; <2% of a dose excreted unchanged in urine.
Small amounts of voriconazole removed by hemodialysis.
Half-life
As a result of non-linear pharmacokinetics, terminal half-life is dose dependent and therefore not useful in predicting accumulation or elimination of the drug.
Special Populations
In patients with mild or moderate hepatic impairment (Child-Pugh class A or B), AUC is increased but peak plasma concentrations not affected. Pharmacokinetic data not available for patients with severe hepatic impairment (Child-Pugh class C).
Peak plasma concentrations and AUC following oral or IV administration not substantially affected by renal impairment. However, in patients with moderate renal impairment (Clcr 30–50 mL/minute) receiving IV voriconazole, accumulation of the IV vehicle, sulfobutyl ether beta-cyclodextrin sodium (SBECD) can occur.
There is some evidence that voriconazole systemic metabolism and first-pass metabolism are greater in children than in adults.
Stability
Storage
Oral
Tablets
15–30°C.
For Suspension
2–8°C for up to 18 months.
Following reconstitution, store at 15–30°C in tight container; do not refrigerate or freeze. Discard 14 days after reconstitution.
Parenteral
Powder for IV Infusion
15–30°C.
Following reconstitution with sterile water for injection, IV solutions should be used immediately since they contain no preservative; if not used immediately, reconstituted solutions may be stored for ≤24 hours at 2–8°C.
Compatibility
Parenteral
Solution Compatibility1 HID
aVoriconazole undergoes slight decomposition at room temperature in 24 hours due to mild alkaline nature of sodium bicarbonate.
|
Compatible |
|---|
|
Dextrose 5% in water |
|
Dextrose 5% and potassium chloride 20 mEq |
|
Dextrose 5% in Ringer’s injection, lactated |
|
Dextrose 5% in 0.45 or 0.9% sodium chloride |
|
Ringer’s injection, lactated |
|
Sodium chloride 0.45 or 0.9% |
|
Incompatible |
|
Sodium bicarbonate 4.2%a |
Drug Compatibility
|
Compatible |
|---|
|
Anidulafungin |
|
Caspofungin acetate |
|
Ceftaroline fosamil |
|
Doripenem |
|
Vasopressin |
|
Incompatible |
|
Tigecycline |
Actions and Spectrum
-
Triazole antifungal agent; synthetic derivative of fluconazole.
-
Alters cellular membranes, resulting in increased permeability, secondary metabolic effects, and growth inhibition.
-
Inhibits cytochrome P-450-dependent sterol 14-α-demethylase in susceptible fungi; results in accumulation of C-14-methylated sterols (e.g., lanosterol) and decreased concentrations of ergosterol.
-
Spectrum of antifungal activity includes Aspergillus, Candida, Fusarium, and Scedosporium.
-
Candida: Active in vitro against Candida albicans, C. dubliniensis, C. fumata, C. glabrata, C. guilliermondii, C. kefyr, C. krusei, C. lipolytica, C. lusitaniae, C. metapsilosis, C. orthopsilosis, C. parapsilosis, C. pelliculosa, C. rugosa, and C. tropicalis.
-
Aspergillus: Active in vitro against Aspergillus fumigatus, A. flavus, A. fumigatus, A. niger, and A. terreus.
-
Other fungi: Active in vitro against Exserohilum rostratum. Variable activity in vitro against Fusarium (including F. solani) and Scedosporium apiospermum. Active in vitro against Cryptococcus neoformans and C. gattii.
-
Fungi with reduced susceptibility to other azoles (e.g., fluconazole, itraconazole) may also have reduced susceptibility to voriconazole.
Advice to Patients
-
Importance of taking oral voriconazole at least 1 hour before or 1 hour after meals.
-
Advise patients that tablets contain lactose and should not be used in patients with galactose intolerance, Lapp lactase deficiency, or glucose-galactose malabsorption and that the oral suspension contains sucrose and is not recommended for those with fructose intolerance, sucrase-isomaltase deficiency, or glucose-galactose malabsorption.
-
Possibility of visual changes, including blurred vision and photophobia. Avoid driving, operating machinery, or performing hazardous tasks if visual changes occur; importance of not driving at night while taking voriconazole.
-
Possibility of photosensitivity reactions; importance of avoiding exposure to strong, direct sunlight during voriconazole therapy.
-
Importance of informing clinicians if any of the following symptoms develop during voriconazole therapy: Changes in heart rate or rhythm, chest tightness, itching, yellowing of skin or eyes, extreme fatigue or flu-like symptoms, nausea or vomiting, visual changes, loss of appetite, changes in thinking, difficulty breathing, or seizures.
-
Importance of informing clinicians and discontinuing voriconazole if serious skin reactions (e.g., rash, hives, mouth sores, blisters, peeling skin) occur.
-
Importance of informing clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs, and any concomitant illnesses.
-
Importance of women informing clinicians if they are or plan to become pregnant or plan to breast-feed. Importance of contraceptive measures during voriconazole therapy.
-
Importance of advising patients of other important precautionary information. (See Cautions.)
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
For suspension |
200 mg/5 mL* |
Vfend |
Pfizer |
|
Voriconazole for Suspension |
||||
|
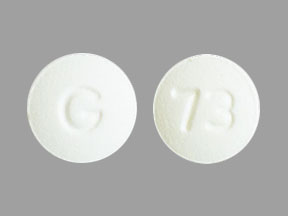
Tablets, film-coated |
50 mg* |
Vfend |
Pfizer |
|
|
Voriconazole Tablets |
||||
|
200 mg* |
Vfend |
Pfizer |
||
|
Voriconazole Tablets |
||||
|
Parenteral |
For injection, for IV infusion only |
200 mg* |
Vfend |
Pfizer |
|
Voriconazole for Injection |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions October 21, 2013. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
† Off-label: Use is not currently included in the labeling approved by the US Food and Drug Administration.
Reload page with references included
Related/similar drugs
More about voriconazole
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (7)
- Drug images
- Side effects
- Dosage information
- During pregnancy
- Drug class: azole antifungals
- Breastfeeding
- En español