Norfloxacin Disease Interactions
There are 9 disease interactions with norfloxacin.
- Colitis
- CNS disorders
- Myasthenia gravis
- Peripheral neuropathy
- QT interval prolongation
- Tendonitis
- Crystalluria
- Diabetes
- Renal dysfunction
Antibiotics (applies to norfloxacin) colitis
Major Potential Hazard, Moderate plausibility. Applicable conditions: Colitis/Enteritis (Noninfectious)
Clostridioides difficile-associated diarrhea (CDAD), formerly pseudomembranous colitis, has been reported with almost all antibacterial drugs and may range from mild diarrhea to fatal colitis. The most common culprits include clindamycin and lincomycin. Antibacterial therapy alters the normal flora of the colon, leading to overgrowth of C difficile, whose toxins A and B contribute to CDAD development. Morbidity and mortality are increased with hypertoxin-producing strains of C difficile; these infections can be resistant to antimicrobial therapy and may require colectomy. CDAD must be considered in all patients who present with diarrhea after antibacterial use. Since CDAD has been reported to occur more than 2 months after antibacterial use, careful medical history is necessary. Therapy with broad-spectrum antibacterials and other agents with significant antibacterial activity should be administered cautiously in patients with history of gastrointestinal disease, particularly colitis; pseudomembranous colitis (generally characterized by severe, persistent diarrhea and severe abdominal cramps, and sometimes associated with the passage of blood and mucus), if it occurs, may be more severe in these patients and may be associated with flares in underlying disease activity. Antibacterial drugs not directed against C difficile may need to be stopped if CDAD is suspected or confirmed. Appropriate fluid and electrolyte management, protein supplementation, antibacterial treatment of C difficile, and surgical evaluation should be started as clinically indicated.
Quinolones (applies to norfloxacin) CNS disorders
Major Potential Hazard, Moderate plausibility.
Quinolones may cause CNS stimulation manifested as tremors, agitation, restlessness, anxiety, confusion, hallucinations, paranoia, insomnia, toxic psychosis, and/or seizures. Benign intracranial hypertension has also been reported. Therapy with quinolones should be administered cautiously in patients with or predisposed to seizures or other CNS abnormalities. In addition, these patients should be advised to avoid the consumption of caffeine-containing products during therapy with some quinolones, most notably ciprofloxacin, enoxacin, and cinoxacin, since these agents can substantially reduce the clearance of caffeine and other methylxanthines, potentially resulting in severe CNS reactions.
Quinolones (applies to norfloxacin) myasthenia gravis
Major Potential Hazard, Moderate plausibility.
Fluoroquinolones have neuromuscular blocking activity and may exacerbate muscle weakness in persons with myasthenia gravis. Postmarketing serious adverse events, including deaths and requirement for ventilatory support, have been associated with fluoroquinolones use in persons with myasthenia gravis. Fluoroquinolones should be avoided in patients with history of myasthenia gravis.
Quinolones (applies to norfloxacin) peripheral neuropathy
Major Potential Hazard, Moderate plausibility.
The use of quinolones has been associated with an increased risk of peripheral neuropathy. Monitor closely and discontinue their use in patients experiencing symptoms of peripheral neuropathy. It is recommended to avoid these agents in patients who have previously experienced peripheral neuropathy.
Quinolones (applies to norfloxacin) QT interval prolongation
Major Potential Hazard, Low plausibility. Applicable conditions: Abnormal Electrocardiogram, Magnesium Imbalance, Ischemic Heart Disease, Hypokalemia, Electrolyte Abnormalities, Arrhythmias, Congestive Heart Failure
Quinolones have been reported to prolong the QT interval of the electrocardiogram in some patients. QT prolongation may potentiate the risk of ventricular arrhythmias including ventricular tachycardia, ventricular fibrillation, and torsade de pointes. The risk appears to be greatest with grepafloxacin and sparfloxacin (both are no longer marketed in the U.S.), although cardiovascular morbidity and mortality attributable to QT prolongation have also been reported rarely with others like gatifloxacin, levofloxacin, ciprofloxacin, and ofloxacin. Reported cases have primarily occurred in patients with advanced age, cardiac disease, electrolyte disturbances, and/or underlying medical problems for which they were receiving concomitant medications known to prolong the QT interval. Therapy with quinolones should be avoided in patients with known QT prolongation and/or uncorrected electrolyte disorders (hypokalemia or hypomagnesemia) and in patients treated concomitantly with class IA or III antiarrhythmic agents. Cautious use with ECG monitoring is advised in patients with other proarrhythmic conditions such as clinically significant bradycardia, congestive heart failure, acute myocardial ischemia, and atrial fibrillation. As QT prolongation may be a concentration-dependent effect, it is important that the recommended dosages or infusion rates of these drugs not be exceeded, particularly in patients with renal and/or hepatic impairment.
Quinolones (applies to norfloxacin) tendonitis
Major Potential Hazard, Moderate plausibility. Applicable conditions: Rheumatoid Arthritis, Renal Dysfunction, Organ Transplant
Tendonitis and ruptures of the shoulder, hand, and Achilles tendons have been reported in patients receiving quinolones, both during and after treatment. Avoid the use of these agents in patients who have a history of tendon disorders or have experienced tendinitis or tendon rupture. Therapy with quinolones should be administered cautiously in patients with patients with kidney, heart, and lung transplant, since it may delay the recognition or confound the diagnosis of a quinolone-induced musculoskeletal effect. Factors that may independently increase the risk of tendon rupture include strenuous physical activity, renal failure, and previous tendon disorders such as rheumatoid arthritis. It is recommended to discontinue these agents if, at any time during therapy, pain, inflammation or rupture of a tendon develops and institute appropriate treatment.
Quinolones (applies to norfloxacin) crystalluria
Moderate Potential Hazard, Moderate plausibility. Applicable conditions: Dehydration, Diarrhea, Vomiting
Crystalluria has been reported rarely during quinolone therapy. Although it is not expected to occur under normal circumstances with usual recommended dosages, patients who are dehydrated (e.g., due to severe diarrhea or vomiting) may be at increased risk and should be encouraged to consume additional amounts of liquid or given intravenous fluid to ensure an adequate urinary output. Alkalinity of the urine should be avoided, since it may also increase the risk of crystalluria. Renal function tests should be performed periodically during prolonged therapy (> 2 weeks).
Quinolones (applies to norfloxacin) diabetes
Moderate Potential Hazard, Moderate plausibility. Applicable conditions: Diabetes Mellitus
The use of certain quinolones has been associated with disturbances in blood glucose homeostasis possibly stemming from effects on pancreatic beta cell ATP-sensitive potassium channels that regulate insulin secretion. Hypoglycemia and, less frequently, hyperglycemia have been reported, although the latter may also occur due to infection alone. Hypoglycemia has usually occurred in patients with diabetes receiving concomitant oral hypoglycemic agents and/or insulin. Administration of ciprofloxacin, levofloxacin, norfloxacin, and especially gatifloxacin in patients treated with sulfonylureas or other oral hypoglycemic agents has resulted in severe, refractory hypoglycemia and hypoglycemic coma. Elderly patients and patients with reduced renal function are particularly susceptible. Blood glucose should be monitored more closely whenever quinolones are prescribed to patients with diabetes. Gatifloxacin has been known to cause hypoglycemic episodes generally within the first 3 days of therapy and sometimes even after the first dose, while hyperglycemia usually occurs 4 to 10 days after initiation of therapy. Patients should be counseled to recognize symptoms of hypoglycemia such as headache, dizziness, drowsiness, nausea, tremor, weakness, hunger, excessive perspiration, and palpitations. If hypo- or hyperglycemia occur during quinolone therapy, patients should initiate appropriate remedial therapy immediately, discontinue the antibiotic, and contact their physician.
Quinolones (applies to norfloxacin) renal dysfunction
Moderate Potential Hazard, High plausibility.
Quinolones (except trovafloxacin, moxifloxacin, and nalidixic acid) and their metabolites are eliminated by the kidney. Patients with renal impairment may be at greater risk for adverse effects from quinolones, including nephrotoxicity, due to decreased drug clearance. Dosage adjustments may be necessary and modifications should be based on the degree of renal impairment and severity of infection in accordance with the individual product package labeling. Renal function tests should be performed periodically during therapy.
Switch to professional interaction data
Norfloxacin drug interactions
There are 528 drug interactions with norfloxacin.
Norfloxacin alcohol/food interactions
There are 3 alcohol/food interactions with norfloxacin.
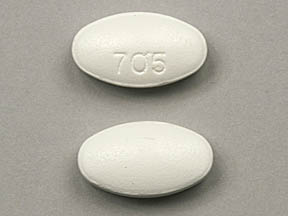
More about norfloxacin
- Check interactions
- Compare alternatives
- Reviews (5)
- Side effects
- Dosage information
- During pregnancy
- Drug class: quinolones and fluoroquinolones
- Breastfeeding
Related treatment guides
Drug Interaction Classification
| Highly clinically significant. Avoid combinations; the risk of the interaction outweighs the benefit. | |
| Moderately clinically significant. Usually avoid combinations; use it only under special circumstances. | |
| Minimally clinically significant. Minimize risk; assess risk and consider an alternative drug, take steps to circumvent the interaction risk and/or institute a monitoring plan. | |
| No interaction information available. |
See also:
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.