Rifamate Disease Interactions
There are 11 disease interactions with Rifamate (isoniazid / rifampin).
- Colitis
- Hepatotoxicity
- Peripheral neuropathy
- Hematopoietic disturbances
- Hepatotoxicity
- Liver disease
- Porphyria
- Hemodialysis
- Human immunodeficiency virus
- Renal dysfunction
- Enzyme induction
Antibiotics (applies to Rifamate) colitis
Major Potential Hazard, Moderate plausibility. Applicable conditions: Colitis/Enteritis (Noninfectious)
Clostridioides difficile-associated diarrhea (CDAD), formerly pseudomembranous colitis, has been reported with almost all antibacterial drugs and may range from mild diarrhea to fatal colitis. The most common culprits include clindamycin and lincomycin. Antibacterial therapy alters the normal flora of the colon, leading to overgrowth of C difficile, whose toxins A and B contribute to CDAD development. Morbidity and mortality are increased with hypertoxin-producing strains of C difficile; these infections can be resistant to antimicrobial therapy and may require colectomy. CDAD must be considered in all patients who present with diarrhea after antibacterial use. Since CDAD has been reported to occur more than 2 months after antibacterial use, careful medical history is necessary. Therapy with broad-spectrum antibacterials and other agents with significant antibacterial activity should be administered cautiously in patients with history of gastrointestinal disease, particularly colitis; pseudomembranous colitis (generally characterized by severe, persistent diarrhea and severe abdominal cramps, and sometimes associated with the passage of blood and mucus), if it occurs, may be more severe in these patients and may be associated with flares in underlying disease activity. Antibacterial drugs not directed against C difficile may need to be stopped if CDAD is suspected or confirmed. Appropriate fluid and electrolyte management, protein supplementation, antibacterial treatment of C difficile, and surgical evaluation should be started as clinically indicated.
INH (applies to Rifamate) hepatotoxicity
Major Potential Hazard, Moderate plausibility. Applicable conditions: Liver Disease, Alcoholism
The use of isoniazid is contraindicated in patients with a history of hepatic injury due to this drug and acute liver disease of any etiology. Caution is advised when using the drug in patients with chronic liver disease or a history of alcoholism. This drug has been associated with severe and sometimes fatal hepatitis, which may occur even after many months of therapy. In a US Public Health Service Surveillance Study of 13,838 persons taking isoniazid, there were 8 deaths among 174 cases of hepatitis. Epidemiologic studies indicate an increased incidence with increasing age, alcohol use, and female gender. As a precautionary measure, routine monitoring of serum transaminases (SGOT, SGPT) and bilirubin may be considered, although a transient and harmless increase in serum transaminase reportedly occurs in 10% to 20% of patients, usually in the first 3 months of therapy. Patients should be advised to promptly discontinue isoniazid therapy and seek medical attention if they experience signs or symptoms suggestive of liver damage such as fever, rash, anorexia, nausea, vomiting, fatigue, right upper quadrant pain, dark urine, and jaundice. Reinstitution of the drug should occur only after symptoms and laboratory abnormalities resolve, with low and gradually increasing dosages.
INH (applies to Rifamate) peripheral neuropathy
Major Potential Hazard, Moderate plausibility. Applicable conditions: Malnourished, Diabetes Mellitus, Alcoholism
Isoniazid commonly causes dose-related peripheral neuropathy, which results from the depletion of pyridoxine in the presence of the drug. The neuropathy is usually preceded by paraesthesia's of the feet and hands. Therapy with isoniazid should be administered cautiously in patients with pre-existing peripheral neuropathy or risk factors for developing the condition, such as malnutrition, diabetes and alcoholism. Careful monitoring is recommended on these patients. Pyridoxine (vitamin B6) at a dosage of 10 to 50 mg/day may prevent or attenuate isoniazid-related peripheral neuropathy and is recommended for these patients.
Rifampin (applies to Rifamate) hematopoietic disturbances
Major Potential Hazard, Low plausibility. Applicable conditions: Bone Marrow Depression/Low Blood Counts
Rifampin may infrequently cause hematopoietic abnormalities such as thrombocytopenia, leukopenia, decreased hemoglobin, and acute hemolytic anemia. Hemolysis has been described as part of an immune-mediated reaction which generally occurs after gaps in therapy. Thrombocytopenia is observed most frequently in patients receiving high-dose intermittent therapy or after a lapse in therapy, but very rarely during daily administration. It is reversible if rifampin is discontinued as soon as purpura appears. Patients with preexisting bone marrow depression or blood dyscrasias should be monitored closely during rifampin therapy for further decreases in blood counts. Although rifampin-related hematologic effects are often transient, cerebral hemorrhage and fatalities have been reported with the continued administration of rifampin after the appearance of purpura.
Rifampin (applies to Rifamate) hepatotoxicity
Major Potential Hazard, High plausibility. Applicable conditions: Liver Disease, Alcoholism
The use of rifampin has been associated with hepatocellular injury and liver dysfunction. Hepatitis and jaundice resulting in death have occurred, mostly in patients with underlying liver disease and during coadministration with other hepatotoxic agents including other antituberculous drugs such as isoniazid and pyrazinamide. Therapy with rifampin should be administered cautiously and under strict medical supervision in patients with liver disease or a history of alcoholism. Serum transaminases (ALT, AST) and bilirubin should be measured at baseline and every 2 to 4 weeks during therapy, but keeping in mind that elevated levels may occur transiently in 10% to 15% of patients, usually during the early days of treatment. Patients should be instructed to discontinue the drug promptly and seek medical attention if signs and symptoms of hepatic injury develop, including fever, rash, anorexia, nausea, vomiting, fatigue, right upper quadrant pain, dark urine, and jaundice.
Rifampin (applies to Rifamate) liver disease
Major Potential Hazard, High plausibility.
Rifampin is primarily metabolized by the liver. Patients with liver disease may be at greater risk for adverse effects from rifampin due to decreased drug clearance. In addition, the accumulation of rifampin may result in hyperbilirubinemia because rifampin competes with bilirubin for uptake by hepatocytes. Dosage adjustments are recommended in patients with liver disease. Withdrawal of rifampin therapy may be required if serum bilirubin is persistently high.
Rifampin (applies to Rifamate) porphyria
Major Potential Hazard, Moderate plausibility.
Rifampin may induce the activity of delta amino levulinic acid synthetase, an enzyme involved in the biosynthesis of porphyrins. The use of rifampin has been associated with isolated cases of porphyria exacerbation. Therapy with rifampin should be administered cautiously in patients with a history of porphyria.
INH (applies to Rifamate) hemodialysis
Moderate Potential Hazard, High plausibility.
Isoniazid is substantially removed by hemodialysis and should be administered after dialysis.
INH (applies to Rifamate) human immunodeficiency virus
Moderate Potential Hazard, Moderate plausibility. Applicable conditions: HIV Infection
Caution and close monitoring is advised when using isoniazid in patients with HIV seropositive patients. Patients with pulmonary tuberculosis and HIV infection may have problems with malabsorption. Screening of antimycobacterial drug levels, especially in patients with advanced HIV disease, may be necessary to prevent the emergence of multi-drug resistant tuberculosis.
INH (applies to Rifamate) renal dysfunction
Moderate Potential Hazard, Moderate plausibility.
Isoniazid may cause cerebellar syndrome in patients with chronic kidney disease. Patients with end-stage renal disease have been reported to have an increased risk of developing tuberculosis. Careful monitoring is recommended if this drug is used in patients with severe renal dysfunction. Dosage adjustments in renal impairment are generally not necessary except in slow acetylators with a creatinine clearance below 10 mL/min. Approximately 50% of Blacks and Caucasians are slow acetylators, and most Eskimos and Asians are rapid acetylators.
Rifampin (applies to Rifamate) enzyme induction
Moderate Potential Hazard, Moderate plausibility. Applicable conditions: Hyperthyroidism, Hyperadrenocorticism, Hypoparathyroidism, Hypothyroidism, Panhypopituitarism, Hyperparathyroidism, Adrenal Insufficiency
Rifampin has enzyme-inducing effects that can enhance the metabolism of many endogenous substrates, including adrenal hormones, thyroid hormones, and vitamin D, the latter of which may affect serum calcium, phosphate and parathyroid hormone levels. Patients with preexisting imbalances of these hormones should be monitored more closely during long-term therapy with rifampin. In patients whose hormonal condition is stabilized on treatment, adjustments may be necessary in their treatment regimen to compensate for these effects.
Switch to professional interaction data
Rifamate drug interactions
There are 949 drug interactions with Rifamate (isoniazid / rifampin).
Rifamate alcohol/food interactions
There are 2 alcohol/food interactions with Rifamate (isoniazid / rifampin).
More about Rifamate (isoniazid / rifampin)
- Rifamate consumer information
- Check interactions
- Compare alternatives
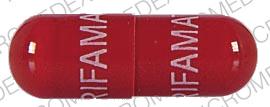
- Drug images
- Side effects
- Dosage information
- During pregnancy
- Drug class: antituberculosis combinations
Related treatment guides
Drug Interaction Classification
| Highly clinically significant. Avoid combinations; the risk of the interaction outweighs the benefit. | |
| Moderately clinically significant. Usually avoid combinations; use it only under special circumstances. | |
| Minimally clinically significant. Minimize risk; assess risk and consider an alternative drug, take steps to circumvent the interaction risk and/or institute a monitoring plan. | |
| No interaction information available. |
See also:
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.