Surgery for Retinal Detachment
Medically reviewed by Drugs.com. Last updated on Sep 23, 2025.
AMBULATORY CARE:
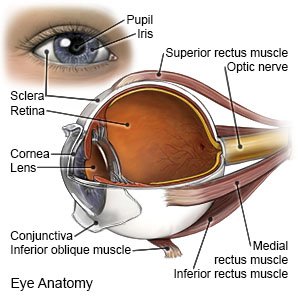
What you need to know about surgery for retinal detachment:
Surgery for retinal detachment is done to reattach your retina to the back of your eye.
 |
How to prepare for surgery:
You may not have time to prepare for surgery. If you have time to prepare, your healthcare provider will tell you how.
- You may be told not to eat or drink anything after midnight on the day of your surgery. Ask someone to drive you home and stay with you for 48 hours after surgery.
- Tell your provider about all your current medicines. He or she will tell you if you need to stop any medicine for the procedure, and when to stop. He or she will tell you which medicines to take or not take on the day of your surgery.
- Tell your provider about any allergies you have, including to anesthesia or medicines. You may be given an antibiotic to help prevent a bacterial infection.
What will happen during surgery:
- You may be given general anesthesia to keep you asleep and free from pain during surgery. You may instead be given IV sedation to make you feel calm and relaxed during surgery. If your are given IV sedation, you will also be given local anesthesia to numb the surgery area. With local anesthesia, you may still feel pressure or pushing during surgery, but you should not feel any pain.
- Your retina may be reattached to your eye with 1 or more of the following:
- A vitrectomy is surgery to remove vitreous gel from your eye and replace it with a gas or oil bubble. The bubble will allow the retina to return to the correct place. If an oil bubble is placed, you may need another surgery to remove it.
- A scleral buckle is surgery to place a flexible band around your eye. Your surgeon may also drain fluid from beneath your retina. This will help move the retina back into its correct position. You will not feel or see the band around your eye.
- A pneumatic retinopexy is surgery to inject a gas bubble into your eye. The bubble helps push the retina into the correct place. The bubble will reabsorb over time. A laser or freezing treatment will be used to permanently hold the retina at the back of the eye.
What to expect after surgery:
- Healthcare providers will monitor you until you are awake. Do not get out of bed until your healthcare provider says it is okay.
- You may need to keep your head in 1 position. This can help prevent an increase in pressure in your eye.
- You may have pain and swelling in or around your eye for several days. You may also have bloody or pink eye drainage for 48 hours.
- It may take several months for your vision to get better.
Risks of surgery:
You may bleed more than expected or get an infection. Eye structures may be damaged during surgery. You may develop a cataract or glaucoma. Surgery may not improve or return your vision.
Seek care immediately if:
- You have severe eye pain.
- You have sudden changes in your vision or loss of vision.
- Blood soaks through your bandage.
Related medications
Call your doctor or surgeon if:
- You have a fever or chills.
- Your eye is red, swollen, or draining pus.
- You have questions or concerns about your condition or care.
Medicines:
You may need any of the following:
- Antibiotics help prevent a bacterial infection. They may be given as eye drops.
- Antinausea medicine helps prevent nausea and vomiting. Nausea and vomiting can increase pressure in your eye and cause damage.
- Stool softeners help prevent constipation. Constipation causes you to strain. This can increase pressure in your eye and cause damage.
- Steroids help decrease swelling. They may be given as eye drops.
- Prescription pain medicine may be given. Ask your healthcare provider how to take this medicine safely. Some prescription pain medicines contain acetaminophen. Do not take other medicines that contain acetaminophen without talking to your healthcare provider. Too much acetaminophen may cause liver damage. Prescription pain medicine may cause constipation. Ask your healthcare provider how to prevent or treat constipation.
- NSAIDs , such as ibuprofen, help decrease swelling, pain, and fever. NSAIDs can cause stomach bleeding or kidney problems in certain people. If you take blood thinner medicine, always ask your healthcare provider if NSAIDs are safe for you. Always read the medicine label and follow directions.
- Acetaminophen decreases pain and fever. It is available without a doctor's order. Ask how much to take and how often to take it. Follow directions. Read the labels of all other medicines you are using to see if they also contain acetaminophen, or ask your doctor or pharmacist. Acetaminophen can cause liver damage if not taken correctly.
- Take your medicine as directed. Contact your healthcare provider if you think your medicine is not helping or if you have side effects. Tell your provider if you are allergic to any medicine. Keep a list of the medicines, vitamins, and herbs you take. Include the amounts, and when and why you take them. Bring the list or the pill bottles to follow-up visits. Carry your medicine list with you in case of an emergency.
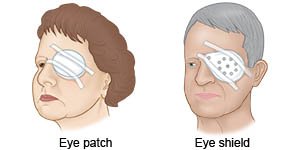
Wear your eye patch or shield as directed:
These devices help your eye rest and heal.
 |
Wound care:
Remove the bandage in 48 hours or as directed. Apply a cool compress on your eye for 15 to 20 minutes every hour or as directed. Use a washcloth or towel soaked in cool water. A cool compress will help decrease swelling and pain. Replace your eye patch or shield after you remove the compress.
Activity:
Ask your healthcare provider when you can drive and return to your normal activities. Some activities can increase pressure in your eye. High pressure can prevent healing and may cause the retina to detach again. Follow these instructions to prevent an increase in eye pressure:
- Do not cough, vomit, or strain to have a bowel movement. You may be given medicine to prevent vomiting or constipation.
- Keep your head above your waist at all times. Do not bend forward.
- Lie or rest in the position that your healthcare provider tells you to. If you had a vitrectomy, lie face down as much as possible. Keep your head turned to the side to allow easy breathing. Your healthcare provider will tell how often you can sit up or change your position. After other types of eye surgery, you may need to keep your head in 1 position, or sleep with your head raised on pillows.
- Ask your healthcare provider when you can travel to high altitudes or on an airplane.
- Do not exercise until your healthcare provider says it is okay.
Follow up with your doctor or surgeon in 1 to 2 days, or as directed:
Write down your questions so you remember to ask them during your visits.
© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
