Sickle Cell Disease in Children
Medically reviewed by Drugs.com. Last updated on Aug 4, 2025.
What is sickle cell disease (SCD)?
SCD causes your child's red blood cell (RBC)s to be sickle-(crescent) shaped. The sickle shape is caused by abnormal hemoglobin within the RBC. Hemoglobin carries oxygen to all tissues in your child's body. Sickle-shaped RBCs can get stuck inside blood vessels. This can stop or slow blood flow, and prevent oxygen from getting to tissues. When this happens, it is called a sickle cell crisis. SCD also causes RBCs break apart and die faster than healthy RBCs. This causes low red blood cell levels (anemia).
What causes SCD?
Your child is born with SCD. SCD is passed from parents to a child. Your child is given two abnormal genes for hemoglobin, one from each parent.
What are the signs and symptoms of SCD?
The following symptoms may come and go, or happen during a sickle cell crisis:
- Pain anywhere in the body
- Swollen hands and fingers
- Feeling very tired
- Dizziness or weakness
- Poor feeding in babies or young children
- Yellow skin or eyes
- Pale skin
- Shortness of breath
How is SCD diagnosed and managed?
A blood test can check the shape and number of your child's RBCs. Your child may need continued screening for conditions that can develop because of SCD. Your child may need any of the following:
- Medicines may be given to decrease pain or decrease sickling of your child's RBCs. Your child may also need medicine to prevent a bacterial infection.
- A blood transfusion increases the number of healthy RBCs in your child's blood. Your child may need a blood transfusion more than once.
- Surgery may be done to remove your child's spleen or gallbladder. Surgery may be needed if RBCs often get stuck in your child's spleen or he or she has gallstones.
- A stem cell transplant , also called a bone marrow transplant, helps your child's body make new, healthy blood cells.
What can I do to care for my child and manage my child's pain?
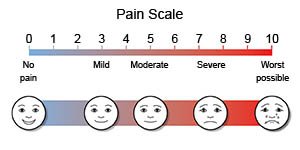
- Monitor your child for signs of pain. Watch for redness or swelling in your child's hands or feet. If he or she is too young to talk, watch his or her face and look for other signs of pain. If your child is old enough to talk, ask him or her where he or she feels the pain and how bad it is. Have your child use a pain scale to show you how much pain he or she feels.
- Apply heat to areas of pain. Heat can help decrease your child's pain. Use a heating pad or place your child in a warm bath. Do this for 20 to 30 minutes every 2 hours for as many days as directed.
- Gently massage painful areas. This can help decrease pain and may help your child relax.
- Help your child balance rest and exercise. Have your child rest during a sickle cell crisis. Over time, he or she can increase activity. Activity may help decrease pain. Ask your child's healthcare provider which activities are safe for your child. He or she may need to avoid activities that increase risk for injury, such as football. Your child should take breaks during activity and drink plenty of water.
- Feel your child's spleen if he or she has pain, yellow skin or eyes, or a swollen abdomen. Your child's healthcare provider will show you how to feel your child's spleen. The spleen will get bigger if RBCs are stuck there. This is called splenic sequestration crisis. Seek care immediately if your child's spleen feels larger than normal.
- Talk to caregivers, teachers, and others in your child's school. Tell them that your child has SCD. Teach them the signs and symptoms of a crisis and acute chest syndrome. Teach them what to do if they see any signs or symptoms of these problems.
What can I do to prevent a sickle cell crisis in my child?
A sickle cell crisis may be caused by illness, changes in temperature, stress, dehydration, or being at high altitudes. Do the following to help prevent a sickle cell crisis in your child:
- Give your child liquids as directed. Dehydration can increase your child's risk for a sickle cell crisis. Ask how much liquid he or she should drink each day and which liquids are best for him or her.
- Do not let your child get too hot or too cold. Dress your child in light clothing in the summer and warm clothing in the winter. Help him or her avoid quick changes in temperature. Do not let your child go from a warm place to a cold place quickly. Have your child get in a pool slowly instead of jumping in.
- Ask about vaccinations your child needs. Vaccinations can help prevent a viral infection that may lead to a sickle cell crisis. Take your child to get a flu shot every year as directed. He or she may also need a pneumonia vaccine every 5 years.
- Wash your hands and your child's hand frequently. Frequent handwashing can help prevent illness and your child's risk for a crisis. Have your child wash his or her hands before he or she eats and after he or she uses the bathroom. Wash your hands before you prepare your child's food.

- Talk to your child about harmful behaviors. Tell your child not to smoke and to stay away from others who smoke. Tell him or her not to drink alcohol. Smoking cigarettes or drinking alcohol increases your child's risk for a sickle cell crisis.
- Help your child manage stress. Your child's healthcare provider may recommend relaxation techniques and deep breathing exercises to help decrease your child's stress. The provider may recommend that your child talk to someone about his or her stress or anxiety, such as a school counselor.
- Do not let your child travel in an unpressurized plane or travel to high altitudes. These environments are low in oxygen and may cause a sickle cell crisis.
Related medications
Treatment options
The following list of medications are related to or used in the treatment of this condition.
What are the risks of SCD?
SCD increases your child's risk for the following:
- Infection
- Breathing problems
- Damage to organs such as the heart, liver, kidney, bone marrow, or spleen
- Stroke, heart attack, or blood clots in the lungs or limbs
- Eye problems
- Joint problems
- Open sores on your legs
- Depression
- Delayed growth or late puberty
Call your local emergency number (911 in the US) if:
- Your child says that he or she cannot see out of one or both eyes.
- Your child is confused, has problems speaking, or has weakness or numbness in his or her arm, leg, or face.
- Your child has a seizure.
- Your child loses consciousness or cannot be woken.
When should I seek immediate care?
- Your child feels lightheaded, short of breath, and has chest pain.
- Your child coughs up blood.
- Your child's heart is beating faster than usual.
- Your child has a fever of 100.4°F (38°C) or higher.
- Your child has abdominal pain, is bloated, or is vomiting a lot.
- Your child's spleen feels larger than normal.
- Your child has a severe headache.
- Your child's arm or leg is painful, red, and larger than usual.
- Your child's pain does not decrease after you give him or her pain medicine.
- Your male child's penis is painful or stays erect for more than 4 hours.
- Your child tells you that he or she wants to hurt himself or herself.
When should I call my child's doctor?
- Your child's eyes or skin is yellow.
- Your child has a cold or the flu.
- You see blood in your child's urine.
- Your child is urinating less than usual or not at all.
- Your child is less active or more sleepy than usual.
- Your child has an open sore on his or her skin that will not heal.
- Your child is constipated or has diarrhea.
- Your child has changes in his or her vision.
- Your child has new or worse swelling over his or her joints.
- Your child is anxious or depressed.
- You have questions or concerns about your child's condition or care.
Care Agreement
You have the right to help plan your child's care. Learn about your child's health condition and how it may be treated. Discuss treatment options with your child's healthcare providers to decide what care you want for your child. The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
Learn more about Sickle Cell Disease
Treatment options
Care guides
Symptoms and treatments
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
