Roux-En-Y Gastric Bypass
Medically reviewed by Drugs.com. Last updated on Aug 4, 2025.
AMBULATORY CARE:
What you need to know about roux-en-Y gastric bypass surgery:
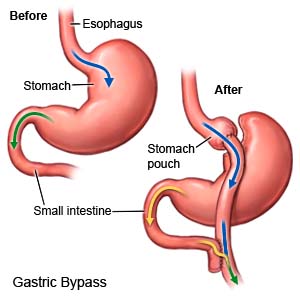
Roux-en-Y gastric bypass is a type of weight loss surgery. Staples are used to make a small stomach pouch that is separate from the rest of your stomach. The new stomach pouch is connected to the middle part of the small intestine. Food will bypass (go around) the rest of the stomach and move directly into the small intestine. The surgery makes your stomach permanently smaller so that you feel full sooner and cannot eat as much during meals. Your body will not absorb as many calories from food because part of your stomach and intestines are bypassed.
 |
What to understand before you have a roux-en-Y gastric bypass:
- You will work closely with a dietitian before and after surgery. Your dietitian will talk to you about nutrition and what you should eat and drink before and after surgery. You may need to follow a very low-calorie diet for several weeks before surgery. This will help you lose some weight before surgery. Weight loss will help your liver handle anesthesia better. It will also help you create healthy nutrition and activity habits.
- Your surgeon will talk to you about self-care and follow-up activities you will need after surgery. You will need to take vitamins and come in often to have your progress checked.
- If you have diabetes, your diabetes medicine needs may change after surgery. This depends on the medicine you take and if you have type 1 or type 2 diabetes. Do not change your diabetes medicine unless directed. Your providers will help you set schedules for checking your blood sugar levels and taking your medicine.
- Your medicine needs may change if you are taking medicine for hypothyroidism. Your healthcare providers will monitor your TSH levels and make medicine changes if needed. Do not change your thyroid medicine unless directed.
- Your surgeon will talk to you about family planning if you are a woman of childbearing age. It is important that you do not get pregnant for 12 to 18 months after surgery. Then your pregnancy will need to be monitored for your safety and your baby's safety. Your provider will tell you how much weight is safe for you to gain during pregnancy. He or she will help you create healthy meal plans so you get the right nutrition without gaining too much weight. If you want to prevent pregnancy, healthcare providers will help you choose the right kind of birth control. You may not be able to use birth control pills because you will not be able to absorb them fully after surgery.
How to prepare for surgery:
- Your surgeon will talk to you about how to prepare for surgery. He or she may tell you not to eat or drink anything after midnight on the day of your surgery. Arrange to have someone drive you home and stay with you to make sure you are okay.
- Tell your surgeon about all medicines you currently take. He or she will tell you if you need to stop any medicine for surgery, and when to stop. He or she will tell you which medicines to take or not take on the day of your surgery.
- Tell your surgeon about all your allergies, including anesthesia or antibiotics. You may be given an antibiotic to help prevent a bacterial infection.
- You may need a fasting blood test to check your lipid (fat) levels, or other blood tests. Your heart may be checked to make sure it is healthy enough for surgery. You may also need tests to check your digestive system.
- If you have diabetes, healthcare providers will help you schedule meals and medicines before surgery. Your A1c level may also be checked.
- If you currently use tobacco products, you will need to quit before you have surgery. It is best to quit at least 1 year before surgery. You must quit at least 6 weeks before surgery. Talk to your surgeon or other healthcare providers if you need help quitting.
What will happen during surgery:
- You may be given general anesthesia to keep you asleep and free from pain during surgery. You may instead be given spinal anesthesia to numb the surgery area. With spinal anesthesia, you may still feel pressure or pushing during surgery, but you should not feel pain.
- Your surgeon will make small incisions in your abdomen. He or she will use staples to make a small stomach pouch that is closed off from the rest of your stomach. The new stomach pouch is then connected to the middle part of the small intestine. The incisions will be closed with stitches or medical tape.
What will happen after surgery:
- Medicines may be given to prevent or treat pain, nausea, or a bacterial infection.
- A nasogastric (NG) tube may be put into your nose and down into your stomach during surgery. The NG tube helps prevent vomiting and may help get your intestines working. The NG tube is usually removed 1 day after surgery.
- A test called a contrast swallow may be done the first day after surgery. This test checks for leaks in your stomach. You will be able to have clear liquids when your stomach starts working after surgery and tests show no leaks. You may be given ice chips at first. Then you will get clear liquids such as water, broth, or juice.
- You will be helped to walk around after surgery to help prevent blood clots.
- As you begin to eat differently, you may begin to lose weight. It may take several months to reach a healthy weight.
Risks of roux-en-Y gastric bypass surgery:
You may bleed more than expected or get an infection. Your spleen or other organs may be injured during surgery. You may have abdominal pain, heartburn, or a stomach ulcer. You may develop a life-threatening blood clot. The staples inside your stomach could break down. The new connections to your stomach and intestines could form scars, narrow areas, or leaks. Stomach juices may leak into your abdomen and you may need emergency surgery. You may develop gallstones or an incisional hernia (a weak area near your incision). You may need a larger incision than expected during laparoscopic surgery. After surgery, you may not lose any weight. You may lose weight and then gain it back.
Related medications
Call your local emergency number (911 in the US) for any of the following:
- You feel lightheaded or short of breath, or you have chest pain.
- You cough up blood.
Seek care immediately if:
- Your arm or leg feels warm, tender, and painful. It may look swollen and red.
- Blood soaks through your bandages.
- Your stitches or incisions come apart.
- You cannot stop vomiting.
- You have a fever higher than 100°F (37.8°C).
Call your doctor or surgeon if:
- You have pain or pressure in your abdomen or back, hiccups, and you feel restless.
- You have redness, swelling, or pus coming from your incisions.
- You have nausea and are vomiting.
- You feel your heart beating faster than usual.
- You have questions or concerns about your condition or care.
Medicines:
You may need any of the following:
- A multivitamin may be recommended by your healthcare provider or dietitian. This will help replace vitamins and minerals you may lose from eating less food.
- Medicine may be given to lower the amount of stomach acid, or to relieve heartburn.
- Nausea medicine may be needed to help decrease nausea and prevent vomiting.
- Acetaminophen decreases pain and fever. It is available without a doctor's order. Ask how much to take and how often to take it. Follow directions. Read the labels of all other medicines you are using to see if they also contain acetaminophen, or ask your doctor or pharmacist. Acetaminophen can cause liver damage if not taken correctly.
- Prescription pain medicine may be given. Ask your healthcare provider how to take this medicine safely. Some prescription pain medicines contain acetaminophen. Do not take other medicines that contain acetaminophen without talking to your healthcare provider. Too much acetaminophen may cause liver damage. Prescription pain medicine may cause constipation. Ask your healthcare provider how to prevent or treat constipation.
- Blood thinners help prevent blood clots. Clots can cause strokes, heart attacks, and death. Many types of blood thinners are available. Your healthcare provider will give you specific instructions for the type you are given. The following are general safety guidelines to follow while you are taking a blood thinner:
- Watch for bleeding and bruising. Watch for bleeding from your gums or nose. Watch for blood in your urine and bowel movements. Use a soft washcloth on your skin, and a soft toothbrush to brush your teeth. This can keep your skin and gums from bleeding. If you shave, use an electric shaver. Do not play contact sports.
- Tell your dentist and other healthcare providers that you take a blood thinner. Wear a bracelet or necklace that says you take this medicine.
- Do not start or stop any other medicines or supplements unless your healthcare provider tells you to. Many medicines and supplements cannot be used with blood thinners.
- Take your blood thinner exactly as prescribed by your healthcare provider. Do not skip a dose or take less than prescribed. Tell your provider right away if you forget to take your blood thinner, or if you take too much.
- Take your medicine as directed. Contact your healthcare provider if you think your medicine is not helping or if you have side effects. Tell your provider if you are allergic to any medicine. Keep a list of the medicines, vitamins, and herbs you take. Include the amounts, and when and why you take them. Bring the list or the pill bottles to follow-up visits. Carry your medicine list with you in case of an emergency.
Self-care:
- Care for your surgery area as directed. When you allowed to bathe, carefully wash the area with soap and water. Dry the area and put on new, clean bandages as directed. Change your bandages when they get wet or dirty.
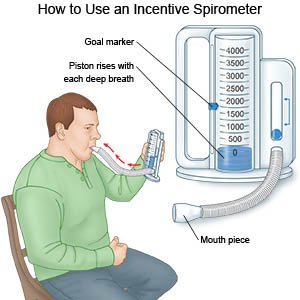
- Do deep breathing and coughing as directed. Take deep breaths and cough 10 times each hour or as directed. This will help prevent pneumonia. You may need to hold a pillow on your abdomen for support and comfort. Take a deep breath and hold it for as long as you can. Let the air out and then cough strongly. Deep breaths help open your airway. You may be given an incentive spirometer to help you take deep breaths. Put the plastic piece in your mouth and take a slow, deep breath. Then let the air out and cough.
- Take short walks often throughout the day. Walks help prevent blood clots. Do not do any strenuous activity or lift more than 10 pounds. Ask your healthcare provider about the best exercise plan for you at your follow-up visit. Ask when you can return to work or school.
- Go to therapy. Therapy may include working with a counselor to understand your reasons for overeating. You may want to join a support group to talk with others who have had roux-en-Y gastric bypass surgery.
Follow your nutrition plan:
Ask your dietitian or nutritionist any questions you have about your nutrition plan. The plan will include which foods to eat and how much of each to eat during a meal.
- Prevent dumping syndrome. Dumping syndrome happens when high-sugar or high-fat foods and drinks go into your intestine too quickly after a meal. Dumping syndrome may also occur if you drink liquids during a meal. Dumping syndrome may cause you to sweat, or feel faint, weak, and dizzy. You may have stomach cramps, an upset stomach, and diarrhea.
- Eat slowly. Chew your food well before you swallow. Large bits of food may cause choking or may block your stomach. If you eat too much or do not chew well enough before you swallow, you may vomit.
- Eat 3 small meals each day. Do not eat snacks between meals unless your healthcare provider says it is okay. Stop eating when you feel full, even if you have not eaten all of your meal. If you often eat too much and do not follow instructions, you may stretch out your stomach pouch.
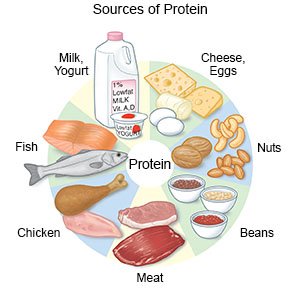
- Eat nutritious foods. Eat plenty of protein. Foods that contain protein include chicken, fish, eggs, and dairy products. You may need protein drinks for the first week after surgery. Avoid candy, cookies, ice cream, and fried foods.
- Drink liquids between meals. Wait at least 1 or 2 hours after a meal before you drink liquids. Do not drink liquids with meals. Drink water, diet drinks, or other drinks that have few or no calories. Do not drink carbonated liquids, such as soft drinks.
Follow up with your doctor or surgeon as directed:
You will need to come in to have your surgery area checked. You will also need to come in over time to have your vitamin levels checked and to monitor your progress. Write down your questions so you remember to ask them during your visits.
© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.
Learn more about Roux-En-Y Gastric Bypass
Treatment options
Care guides
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
