Robot Assisted Laparoscopic Sleeve Gastrectomy
Medically reviewed by Drugs.com. Last updated on Aug 4, 2025.
AMBULATORY CARE:
What you need to know about robot assisted laparoscopic sleeve gastrectomy (RALSG):
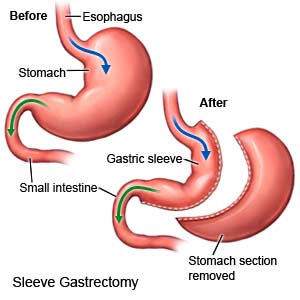
RALSG is surgery to remove most of your stomach through small incisions in your abdomen. The remaining stomach forms a tube or sleeve. You will feel full faster and have a decreased desire for food. RALSG is done with a machine that is controlled by your surgeon. The machine has mechanical arms that use small tools to help perform the surgery.
What you need to know before you have RALSG:
- You will work closely with a dietitian before and after surgery. Your dietitian will talk to you about nutrition and what you should eat and drink before and after surgery. You may need to follow a very low-calorie, low-carbohydrate, or liquid diet for 2 weeks before surgery. This will help you lose weight and make the surgery safer for your liver.
- Your surgeon will talk to you about self-care and follow-up activities you will need after surgery. You will need to take vitamins and come in to have your progress checked.
- If you have diabetes, your diabetes medicine needs may change after surgery. This depends on the medicine you take and if you have type 1 or type 2 diabetes. Do not change your diabetes medicine unless directed. Your providers will help you set schedules for checking your blood sugar levels and taking your medicine.
- Your medicine needs may change if you are taking medicine for hypothyroidism (low thyroid hormone level). Your healthcare providers will monitor your TSH levels and make medicine changes if needed. Do not change your thyroid medicine unless directed.
- Your surgeon will talk to you about family planning. If you are female, it is important that you do not get pregnant for 12 to 18 months after surgery. Then your pregnancy will need to be monitored for your safety and your baby's safety. Your provider will tell you how much weight is safe for you to gain during pregnancy. Your provider will help you create healthy meal plans so you get the right nutrition. If you want to prevent pregnancy, healthcare providers will help you choose the right kind of birth control. You may not be able to use birth control pills because you may not be able to absorb them fully after surgery.
How to prepare for surgery:
- Your surgeon will tell you how to prepare. You may be told not to eat or drink anything after midnight on the day of your surgery. Arrange to have someone drive you home when you are discharged.
- Tell your surgeon about all medicines you currently take. Your surgeon will tell you if you need to stop any medicine for the surgery, and when to stop. Your surgeon will tell you which medicines to take or not take on the day of surgery.
- Tell your surgeon about any allergies you have, including to anesthesia or medicines. You may be given an antibiotic to help prevent a bacterial infection. You may also be given blood thinner medicine to help prevent blood clots.
- Your surgeon will tell you if you need any tests before your surgery, and when to have them. You may need to have an upper endoscopy before surgery. This is a procedure to look inside your esophagus and stomach. This will check for any problems and help your surgeon plan your surgery.
What will happen during surgery:
- You will be given general anesthesia to keep you asleep and free from pain during surgery. Your surgeon will make several small incisions in your abdomen. Your abdomen will be filled with carbon dioxide to lift the muscles away from your organs. This helps your surgeon see your stomach and nearby organs better.
- Surgical tools are attached to the arms of the robot. Your surgeon will guide the arms to place a laparoscope and other tools inside your abdomen. A laparoscope is a long, thin tube with a light and camera on the end. Your surgeon will then use the arms to remove most of your stomach. The remaining stomach will be stapled to create a small tube or sleeve.
- Your surgeon will then remove the tools from your abdomen. Your incisions will be closed with stitches or medical glue and covered with bandages.
 |
What to expect after RALSG:
- You will be taken to a recovery room until you wake up. Healthcare providers will monitor you for any problems. You will then be taken to your hospital room. You may need to stay in the hospital for 1 to 2 days. You will be helped to walk around after surgery to help prevent blood clots.
- A nasogastric (NG) tube may be put into your nose and down into your stomach during surgery. The NG tube helps prevent vomiting and may help your intestines start to work. The NG tube is usually removed soon after surgery.
- Your surgeon will tell you when you can eat and drink. You may be given ice chips at first. Then you will get clear liquids such as water, broth, or juice. You will be told when you can start to eat soft foods.
Risks of RALSG:
You may bleed more than expected or develop an infection. Organs near the surgery area may be damaged. During surgery, you may need 1 large incision instead of several small incisions. A leak may develop along the staple line where it is holding your sleeve closed. This leak can cause a severe infection. You may have nausea, vomiting, or heartburn. You may not lose as much weight as you expect. You may develop a life-threatening blood clot.
Related medications
Call your local emergency number (911 in the US) if:
- You have trouble breathing, chest pain, or you cough up blood.
Seek care immediately if:
- Your arm or leg feels warm, tender, and painful. It may look swollen and red.
- You have severe stomach pain, and your abdomen feels firm or bloated.
- You cannot stop vomiting.
- Blood soaks through your bandage or your incision sites come apart.
- You have a fever higher than 101°F (38.3°C).
- Your bowel movements are black or bloody.
- Your incision site is red, swollen, or draining pus.
- Your pain does not get better with medicine, or it gets worse.
Call your doctor or surgeon if:
- You have nausea that does not get better with medicine, or it gets worse.
- You are constipated.
- You have questions or concerns about your condition or care.
Medicines:
You may need any of the following:
- A multivitamin may be recommended by your healthcare provider or dietitian. This will help replace vitamins and minerals you may lose from eating less food.
- Acid reflux medicine helps decrease stomach acid and heartburn.
- Nausea medicine may be needed to help decrease nausea and prevent vomiting.
- Acetaminophen decreases pain and fever. It is available without a doctor's order. Ask how much to take and how often to take it. Follow directions. Read the labels of all other medicines you are using to see if they also contain acetaminophen, or ask your doctor or pharmacist. Acetaminophen can cause liver damage if not taken correctly.
- Prescription pain medicine may be given. Ask your healthcare provider how to take this medicine safely. Some prescription pain medicines contain acetaminophen. Do not take other medicines that contain acetaminophen without talking to your healthcare provider. Too much acetaminophen may cause liver damage. Prescription pain medicine may cause constipation. Ask your healthcare provider how to prevent or treat constipation.
- Blood thinners help prevent blood clots. Clots can cause strokes, heart attacks, and death. Many types of blood thinners are available. Your healthcare provider will give you specific instructions for the type you are given. The following are general safety guidelines to follow while you are taking a blood thinner:
- Watch for bleeding and bruising. Watch for bleeding from your gums or nose. Watch for blood in your urine and bowel movements. Use a soft washcloth on your skin, and a soft toothbrush to brush your teeth. This can keep your skin and gums from bleeding. If you shave, use an electric shaver. Do not play contact sports.
- Tell your dentist and other healthcare providers that you take a blood thinner. Wear a bracelet or necklace that says you take this medicine.
- Do not start or stop any other medicines or supplements unless your healthcare provider tells you to. Many medicines and supplements cannot be used with blood thinners.
- Take your blood thinner exactly as prescribed by your healthcare provider. Do not skip a dose or take less than prescribed. Tell your provider right away if you forget to take your blood thinner, or if you take too much.
- Take your medicine as directed. Contact your healthcare provider if you think your medicine is not helping or if you have side effects. Tell your provider if you are allergic to any medicine. Keep a list of the medicines, vitamins, and herbs you take. Include the amounts, and when and why you take them. Bring the list or the pill bottles to follow-up visits. Carry your medicine list with you in case of an emergency.
Care for the incision sites as directed:
Wear loose-fitting clothing over the area. Do not get the sites wet until your healthcare provider says it is okay. When it is okay to bathe, do not scrub the sites. Just let water run over them. Dry the area and put on new, clean bandages as directed. Change your bandages when they get wet or dirty. Do not put powders or lotions over your incision sites. Check the area every day for signs of infection, such as swelling, redness, or pus.
Follow your nutrition plan:
Ask your dietitian or nutritionist any questions you have about your nutrition plan. The plan will include which foods to eat and how much of each to eat during a meal.
- Prevent dumping syndrome. Dumping syndrome happens when high-sugar or high-fat foods and drinks go into your intestine too quickly after a meal. Dumping syndrome may also occur if you drink liquids during a meal. Dumping syndrome may cause you to sweat, or feel faint, weak, and dizzy. You may have stomach cramps, an upset stomach, and diarrhea.
- Eat slowly. Chew your food well before you swallow. Large bits of food may cause choking or may block your stomach. If you eat too much or do not chew well enough before you swallow, you may vomit.
- Eat 3 small meals each day. Do not eat snacks between meals unless your healthcare provider says it is okay. Stop eating when you feel full, even if you have not eaten all of your meal. If you often eat too much and do not follow instructions, you may stretch out your stomach pouch.
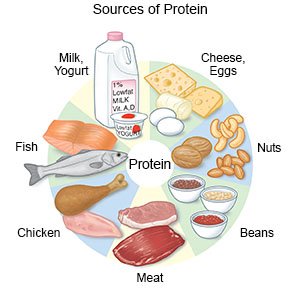
- Eat nutritious foods. Eat plenty of protein. Foods that contain protein include chicken, fish, eggs, and dairy products. You may need protein drinks for the first week after surgery. Avoid candy, cookies, ice cream, and fried foods.
- Drink liquids between meals. Wait at least 1 or 2 hours after a meal before you drink liquids. Do not drink liquids with meals. Drink water, diet drinks, or other drinks that have few or no calories. Do not drink carbonated liquids, such as soft drinks.
Follow up with your doctor or surgeon as directed:
You will need to come in to have your surgery area checked. You will also need to come in over time to have your vitamin levels checked and to monitor your progress. Write down your questions so you remember to ask them during your visits.
© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
