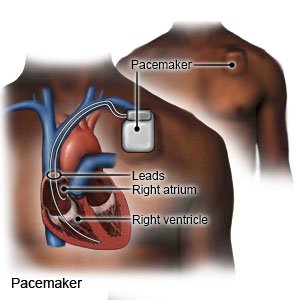
Pacemaker
Medically reviewed by Drugs.com. Last updated on Aug 4, 2025.
What is a pacemaker?
A pacemaker is a small device placed in your chest to help control your heartbeat. You may need a pacemaker if your heartbeat is too slow, too fast, or irregular. A pacemaker is about the size of a large wristwatch. It contains flexible wires (leads) with sensors, a battery, pulse generator, and a small computer. The sensors measure your heartbeat and send the information to the computer. The computer causes the generator to send electrical impulses to your heart. This makes your heart beat correctly. Some pacemakers can also record your heart rate and rhythm.
 |
How do I prepare for a pacemaker insertion?
- Your healthcare provider will tell you how to prepare for the procedure. He or she may tell you not to eat or drink anything after midnight on the day of your procedure. Arrange to have someone drive you home after you leave the hospital.
- You may need a blood test, chest x-ray, or other tests to help your provider plan your procedure.
- Tell your provider about all your current medicines. He or she will tell you if you need to stop any medicine for the procedure. He or she will tell you which medicines to take or not take on the day of your procedure.
- You may be given an antibiotic to prevent infection. Tell your provider if you have ever had an allergic reaction to an antibiotic.
- Make arrangements at home and work, if needed. You will not be able to lift anything heavy for several days after the procedure. Someone may need to help you around the house during this time. Ask your provider when you can return to work after the procedure. You may need to arrange for time off.
Related medications
What will happen during a pacemaker insertion?
- You may be given IV sedation to make you feel calm and relaxed during the procedure. You may also be given local anesthesia to numb the procedure area. With local anesthesia, you may still feel pressure or pushing, but you should not feel pain.
- Your healthcare provider will insert a needle into a large vein in your chest or neck. Next, he or she will guide the wires through the needle and into your heart. Your provider will make an incision in your chest and insert the pacemaker. He or she will connect the wires in your heart to the pacemaker. He or she will also make sure the pacemaker is working correctly.
- Your incisions will be closed with stitches, medical glue, or medical tape. They will be covered with a bandage to prevent an infection.
What should I expect after a pacemaker insertion?
- Healthcare providers will monitor your heartbeat.
- You may need a chest x-ray and an EKG. These tests will make sure your pacemaker is in the correct position and working as it should.
- You may have bruising or pain near your incision. These should get better in a few days.
- You may need to spend a night in the hospital.
What are the risks of a pacemaker insertion?
You may bleed more than expected or get an infection. The pacemaker could move out of place and cause pain and bleeding. The leads may cause a hole in your lung, heart, or blood vessel. Your pacemaker may stop working correctly. This can cause an irregular heartbeat, heart failure, blood clots, or other problems. These problems may become life-threatening.
Care Agreement
You have the right to help plan your care. Learn about your health condition and how it may be treated. Discuss treatment options with your healthcare providers to decide what care you want to receive. You always have the right to refuse treatment. The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
