Fever in Children
Medically reviewed by Drugs.com. Last updated on Aug 4, 2025.
AMBULATORY CARE:
A fever
is an increase in your child's body temperature. Normal body temperature is 98.6°F (37°C). Fever is generally defined as greater than 100.4°F (38°C).Fever is commonly caused by a viral infection. Your child's body uses a fever to help fight the virus. The cause of your child's fever may not be known. A fever can be serious in young children.
Other symptoms include the following:
- Chills, sweating, or shivers
- More tired or fussy than usual
- Nausea and vomiting
- Not hungry or thirsty
- A headache or body aches
Seek care immediately if:
- Your child's temperature reaches 105°F (40.6°C).
- Your child has a dry mouth, cracked lips, or cries without tears.
- Your baby has a dry diaper for at least 8 hours, or he or she is urinating less than usual.
- Your child is less alert, less active, or is acting differently than he or she usually does.
- Your child has a seizure or has abnormal movements of the face, arms, or legs.
- Your child is drooling and not able to swallow.
- Your child has a stiff neck, severe headache, confusion, or is difficult to wake.
- Your child has a fever for longer than 5 days.
- Your child is crying or irritable and cannot be soothed.
Contact your child's healthcare provider if:
- Your child's ear or forehead temperature is higher than 100.4°F (38°C).
- Your child's oral or pacifier temperature is higher than 100°F (37.8°C).
- Your child's armpit temperature is higher than 99°F (37.2°C).
- Your child's fever lasts longer than 3 days.
- You have questions or concerns about your child's fever.
Related medications
Temperature for a fever in children:
- An ear or forehead temperature of 100.4°F (38°C) or higher
- An oral or pacifier temperature of 100°F (37.8°C) or higher
- An armpit temperature of 99°F (37.2°C) or higher
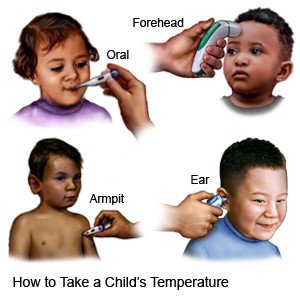
The best way to take your child's temperature
depends on his or her age. The following are guidelines based on a child's age. Ask your child's healthcare provider about the best way to take your child's temperature.
- If your baby is 3 months or younger , take the temperature in his or her armpit.
- If your child is 3 months to 5 years , use an electronic pacifier temperature, depending on his or her age. After age 6 months, you can also take an ear, armpit, or forehead temperature.
- If your child is 5 years or older , take an oral, ear, or forehead temperature.
 |
Treatment
will depend on what is causing your child's fever. The fever might go away on its own without treatment. If the fever continues, the following may help bring the fever down:
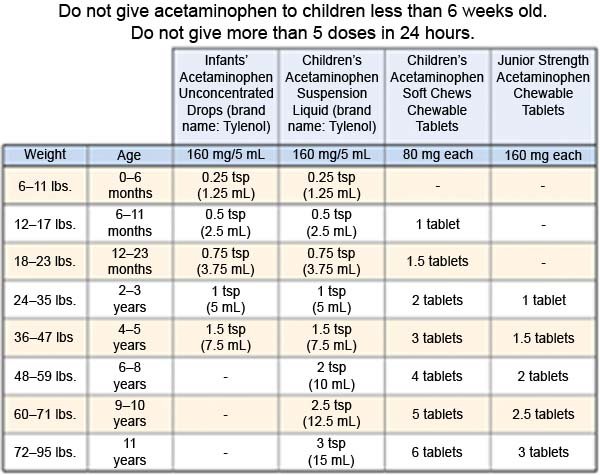
- Acetaminophen decreases pain and fever. It is available without a doctor's order. Ask how much to give your child and how often to give it. Follow directions. Read the labels of all other medicines your child uses to see if they also contain acetaminophen, or ask your child's doctor or pharmacist. Acetaminophen can cause liver damage if not taken correctly.
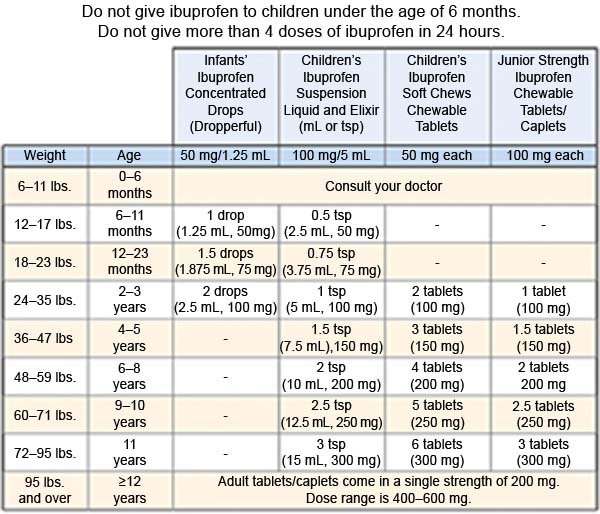
- NSAIDs , such as ibuprofen, help decrease swelling, pain, and fever. This medicine is available with or without a doctor's order. NSAIDs can cause stomach bleeding or kidney problems in certain people. If your child takes blood thinner medicine, always ask if NSAIDs are safe for him or her. Always read the medicine label and follow directions. Do not give these medicines to children younger than 6 months without direction from a healthcare provider.
-
- Do not give aspirin to children younger than 18 years. Your child could develop Reye syndrome if he or she has the flu or a fever and takes aspirin. Reye syndrome can cause life-threatening brain and liver damage. Check your child's medicine labels for aspirin or salicylates.
- Give your child's medicine as directed. Contact your child's healthcare provider if you think the medicine is not working as expected. Tell the provider if your child is allergic to any medicine. Keep a current list of the medicines, vitamins, and herbs your child takes. Include the amounts, and when, how, and why they are taken. Bring the list or the medicines in their containers to follow-up visits. Carry your child's medicine list with you in case of an emergency.
Treatment options
The following list of medications are related to or used in the treatment of this condition.
Make your child more comfortable while he or she has a fever:
- Give your child more liquids as directed. A fever makes your child sweat. This can increase his or her risk for dehydration. Liquids can help prevent dehydration.
- Help your child drink at least 6 to 8 eight-ounce cups of clear liquids each day. Give your child water, juice, or broth. Do not give sports drinks to babies or toddlers.
- Ask your child's healthcare provider if you should give your child an oral rehydration solution (ORS) to drink. An ORS has the right amounts of water, salts, and sugar your child needs to replace body fluids.
- If you are breastfeeding or feeding your child formula, continue to do so. Your baby may not feel like drinking his or her regular amounts with each feeding. If so, feed him or her smaller amounts more often.
- Dress your child in lightweight clothes. Shivers may be a sign that your child's fever is rising. Do not put extra blankets or clothes on him or her. This may cause his or her fever to rise even higher. Dress your child in light, comfortable clothing. Cover him or her with a lightweight blanket or sheet. Change your child's clothes, blanket, or sheets if they get wet.
- Cool your child safely. Use a cool compress or give your child a bath in cool or lukewarm water. Your child's fever may not go down right away after his or her bath. Wait 30 minutes and check his or her temperature again. Do not put your child in a cold water or ice bath.
Follow up with your child's doctor as directed:
Write down your questions so you remember to ask them during your child's visits.
© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.
Learn more about Fever
- Can You Drink Alcohol with Antibiotics?
- Top 9 Things You Must Know About Naproxen
- What are the risks of mixing pain medications and alcohol?
Treatment options
Care guides
Symptoms and treatments
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
