Decision Aid for Pancreatic Cancer Risk Assessment
Medically reviewed by Drugs.com. Last updated on Aug 4, 2025.
What do I need to know about pancreatic cancer risk assessment?
Assessment means figuring out your risk factors for pancreatic cancer. A risk factor is anything that makes it more likely you will develop pancreatic cancer. You can have certain risk factors but not develop pancreatic cancer. You can also have no risk factors but still develop pancreatic cancer. If your risk is high, you may be able to take steps to lower your risk. Your healthcare provider may send you to a pancreatic cancer specialist such as an oncologist, genetics specialist, or gastroenterologist. These providers can help you make an informed decision.
What do I need to know about pancreatic cancer?
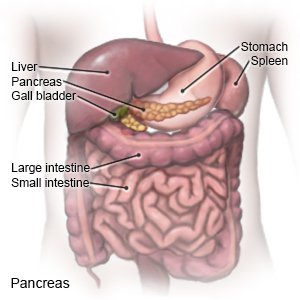
- The pancreas is located just behind the stomach. It helps digest food by making enzymes. The pancreas also makes hormones, such as insulin, to help balance blood sugar levels.
- The average risk for pancreatic cancer is about 1%. In the United States, about 55,000 people find out they have pancreatic cancer each year. About 3% of all cancers are pancreatic cancer. It is the cause of about 7% of all cancer deaths.
- Pancreatic cancer can develop in adults of any age, usually between ages 45 and 71. It is most commonly diagnosed at about age 65.
What increases my risk for pancreatic cancer?
Some risk factors are known to increase the risk for pancreatic cancer. Other factors are believed to increase the risk, but it is not known for sure if there is a connection.
- Being overweight increases the risk, and obesity increases the risk by about 20%.
- Certain genetic conditions , such as hereditary breast and ovarian cancer syndrome, Lynch syndrome, and familial atypical multiple mole melanoma syndrome. Genetic testing may be available to find out if you have any of these.
- A health condition such as long-term pancreatitis or type 2 diabetes increases your risk. A liver disease such as cirrhosis or hepatitis B can also increase your risk.
- Tobacco makes your risk about 2 times higher than for a person who does not use tobacco. The risk is the same if you smoke cigarettes or pipes, or use smokeless tobacco products. Up to 30% of pancreatic cancers can be tied to tobacco use.
- Alcohol increases your risk for any cancer. Heavy alcohol use increases your risk for pancreatitis and cirrhosis of the liver. Pancreatitis or cirrhosis can increase your risk for pancreatic cancer.
- Exposure to certain chemicals increases the risk, such as pesticides or certain dyes.
- An H. pylori infection mainly increases the risk for stomach cancer, but it can also increase the risk for pancreatic cancer.
- Certain foods possibly increase the risk. Examples include red meat (such as beef) or processed meat (such as sausage). A lack of fruits and vegetables may also increase the risk.
Am I a good candidate for pancreatic cancer risk assessment?
Risk assessment may be helpful for you if:
- You are 45 years or older or have a genetic or medical condition that increases your risk for pancreatic cancer.
- You have at least 2 close relatives who have had pancreatic cancer.
- You have a family history of pancreatic cancer defined as familial pancreatic cancer.
- You have at least 3 family members on the same side of the family who have had pancreatic cancer.
- You have pancreatic adenocarcinoma.
- You use tobacco or regularly drink alcohol.
Related medications
How is the assessment done?
- A family history is used to find any pattern of pancreatic cancer in certain family members. Healthcare providers will ask if anyone in your family has had cancer, and what kind.
- A blood test may be used to find genetic changes that increase your risk for pancreatic cancer.
What are the benefits and risks of assessment?
Talk with your healthcare provider about the risks and benefits:
- Benefits include knowing how high your risk is for pancreatic cancer. If your risk is high, you can take steps to lower your risk and prevent disease. You may also be able to help family members lower their risk.
- Risks include a false belief that you will not develop pancreatic cancer if your tests show your risk is low. You can still develop pancreatic cancer later on. Genetic tests may show other family members have an increased risk for pancreatic cancer. This may cause you to worry that someone in your family will develop it even if you do not.
What happens after I have the assessment?
You will meet with your healthcare provider to go over the results. Your provider may recommend genetic counseling and testing to help you know and understand your risk. He or she may also recommend other tests or refer you to specialists.
What can I do to lower my risk for pancreatic cancer?
If your risk is high, your healthcare provider can help you create a specific plan to lower your risk. The following are general lifestyle changes anyone can make:
- Do not smoke. Ask your healthcare provider for information if you currently smoke and need help to quit. E-cigarettes or smokeless tobacco still contain nicotine.
- Reach or maintain a healthy weight. Your healthcare provider can tell you what weight is healthy for you. He or she can help you create a weight loss program, if needed.
- Limit or do not drink alcohol. Your provider can give you daily and weekly limits if you choose to drink. Ask him or her for information if you want to quit drinking and need help to quit.
- Eat a variety of healthy foods. Healthy foods include fruits, vegetables, whole grains, low-fat dairy products, nuts, fish, lean meats, and cooked beans. Your provider or a dietitian can help you create a healthy meal plan.
- Get more physical activity. Aim to get at least 30 minutes of physical activity on most days of the week. Your provider can help you create an activity plan that is right for you.
Care Agreement
You have the right to help plan your care. Learn about your health condition and how it may be treated. Discuss treatment options with your healthcare providers to decide what care you want to receive. You always have the right to refuse treatment. The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
