Ramipril Side Effects
Medically reviewed by Drugs.com. Last updated on Oct 28, 2024.
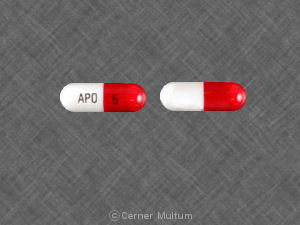
Applies to ramipril: oral capsule.
Important warnings
This medicine can cause some serious health issues
Oral route (capsule; tablet)
When pregnancy is detected, discontinue ramipril as soon as possible.
Drugs that act directly on the renin-angiotensin system can cause injury and death to the developing fetus.
Precautions
It is very important that your doctor check your progress at regular visits to make sure this medicine is working properly. Blood tests may be needed to check for unwanted effects.
Using this medicine while you are pregnant can harm your unborn baby. Use an effective form of birth control to keep from getting pregnant. If you think you have become pregnant while using this medicine, tell your doctor right away.
You should not use this medicine together with sacubitril. Do not use this medicine and sacubitril/valsartan (Entresto®) within 36 hours of each other.
This medicine may cause serious allergic reactions, including anaphylaxis. Anaphylaxis can be life-threatening and requires immediate medical attention. Call your doctor right away if you have a rash, itching, hoarseness, trouble breathing, trouble swallowing, or any swelling of your hands, face, lips, tongue, or throat while you are using this medicine.
Call your doctor right away if you have severe stomach pain (with or without nausea or vomiting). This could be a symptom of a condition called intestinal angioedema.
Dizziness, lightheadedness, or fainting may occur especially when you get up from a lying or sitting position or if you have been taking a diuretic (water pill). Make sure you know how you react to this medicine before you drive, use machines, or do other things that could be dangerous if you are dizzy or not alert. Then sit for a few moments before standing to prevent the dizziness from returning.
Check with your doctor right away if you have pain or tenderness in the upper stomach, pale stools, dark urine, loss of appetite, nausea, unusual tiredness or weakness, or yellow eyes or skin. These could be symptoms of a serious liver problem.
Check with your doctor right away if you have lower back or side pain, decreased frequency or amount of urine, bloody urine, increased thirst, swelling of the face, fingers, or lower legs, weight gain, or increased blood pressure. These could be symptoms of a serious kidney problem.
Check with your doctor if you have a fever, chills, or sore throat. These may be symptoms of an infection resulting from low white blood cells.
Hyperkalemia (high potassium in the blood) may occur while you are using this medicine. Check with your doctor right away if you have the following symptoms: abdominal or stomach pain, confusion, difficulty with breathing, irregular heartbeat, nausea or vomiting, nervousness, numbness or tingling in the hands, feet, or lips, shortness of breath, or weakness or heaviness of the legs. Ask your doctor before you use any medicine, supplement, or salt substitute that contains potassium.
Make sure any doctor or dentist who treats you knows that you are using this medicine. You may need to stop using this medicine several days before having surgery or medical tests.
This medicine may be less effective in black patients. Black patients also have an increased risk of swelling of the hands, arms, face, mouth, or throat. Talk with your doctor if you have concerns about this.
Do not take other medicines unless they have been discussed with your doctor. This includes over-the-counter (nonprescription) medicines for appetite control, asthma, colds, cough, hay fever, or sinus problems, since they may tend to increase your blood pressure.
Serious side effects of ramipril
Along with its needed effects, ramipril may cause some unwanted effects. Although not all of these side effects may occur, if they do occur they may need medical attention.
Check with your doctor immediately if any of the following side effects occur while taking ramipril:
More common side effects
- blurred vision
- confusion
- dizziness, faintness, or lightheadedness when getting up suddenly from a lying or sitting position
- sweating
- unusual tiredness or weakness
Less common side effects
- arm, back, or jaw pain
- chest pain or discomfort
- chest tightness or heaviness
- chills
- cloudy urine
- cold sweats
- decrease in urine output or decrease in urine-concentrating ability
- diarrhea
- fainting
- fast or irregular heartbeat
- shortness of breath
Rare side effects
- seizures
- unexplained bleeding or bruising
Other side effects of ramipril
Some side effects of ramipril may occur that usually do not need medical attention. These side effects may go away during treatment as your body adjusts to the medicine. Also, your health care professional may be able to tell you about ways to prevent or reduce some of these side effects.
Check with your health care professional if any of the following side effects continue or are bothersome or if you have any questions about them:
More common side effects
- cough
Less common side effects
- nausea
- vomiting
Rare side effects
- feeling of constant movement of self or surroundings
- muscle pain or stiffness
- sensation of spinning
- stomach pain
- weight loss
See also:
For healthcare professionals
Applies to ramipril: oral capsule, oral tablet.
General adverse events
The most common adverse reaction is hypotension.[Ref]
Cardiovascular
- Very common (10% or more): Hypotension (11%)
- Common (1% to 10%): Angina pectoris, postural hypotension, orthostatic blood pressure decreased
- Uncommon (0.1% to 1%): Symptomatic hypotension, myocardial ischemia, myocardial infarction, tachycardia, arrhythmia, palpitation, flushing
- Rare (less than 0.1%): Vascular stenosis, hypoperfusion, vasculitis
- Frequency not reported: Disturbed orthostatic regulation, Raynaud's phenomenon[Ref]
Gastrointestinal
- Common (1% to 10%): Nausea, vomiting, diarrhea, gastrointestinal inflammation, digestive disturbances, abdominal discomfort, dyspepsia
- Uncommon (0.1% to 1%): Pancreatitis, pancreatic enzymes increased, abdominal pain, small bowel angioedema, gastritis, constipation, dry mouth
- Rare (less than 0.1%): Glossitis
- Frequency not reported: Dysphagia, gastroenteritis, increased salivation, gastric pain, aphthous stomatitis[Ref]
Other
- Common (1% to 10%): Fatigue, asthenia, vertigo, bronchitis, sinusitis, chest pain
- Uncommon (0.1% to 1%): Peripheral edema, pyrexia, libido decreased
- Rare (less than 0.1%): Conjunctivitis, hearing impaired, tinnitus
- Frequency not reported: Hearing loss, edema, malaise, gynecomastia[Ref]
Respiratory
- Common (1% to 10%): Cough, nonproductive tickling cough, cough increased, dyspnea
- Uncommon (0.1% to 1%): Bronchospasm, asthma aggravated
- Frequency not reported: Eosinophilic pneumonitis, epistaxis, nasal congestion[Ref]
Psychiatric
- Uncommon (0.1% to 1%): Depressed mood, anxiety, nervousness, restlessness, sleep disorder
- Rare (less than 0.1%): Confusional state
- Frequency not reported: Depression, insomnia, disturbance in attention[Ref]
Nervous system
- Common (1% to 10%): Headache, dizziness, syncope
- Uncommon (0.1% to 1%): Paresthesia, dysgeusia, ageusia, somnolence
- Rare (less than 0.1%): Tremor, balance disorder
- Frequency not reported: Smell disturbance, amnesia, convulsions, neuralgia, neuropathy, cerebral ischemia, ischemic stroke, transient ischemic attack, psychomotor skills impaired, burning sensation, parosmia[Ref]
Musculoskeletal
- Common (1% to 10%): Muscle spasm, myalgia
- Uncommon (0.1% to 1%): Arthralgia
- Frequency not reported: Arthritis[Ref]
Dermatologic
- Common (1% to 10%): Maculopapular rash
- Uncommon (0.1% to 1%): Pruritus, hyperhidrosis
- Rare (less than 0.1%): Exfoliative dermatitis, urticaria, onycholysis
- Frequency not reported: Purpura, pemphigus, pemphigoid, erythema multiforme, toxic epidermal necrolysis, Stevens Johnson syndrome, sweating increased, alopecia, psoriasis aggravated, dermatitis psoriasiform, lichenoid exanthema, enanthema[Ref]
Renal
- Common (1% to 10%): Abnormal kidney function
- Uncommon (0.1% to 1%): Renal impairment, acute renal failure[Ref]
Metabolic
- Common (1% to 10%): Creatinine increased, blood potassium increased
- Uncommon (0.1% to 1%): Anorexia, decreased appetite, BUN increased
- Frequency not reported: Weight gain, hyponatremia, loss of appetite, uric acid elevated, blood glucose elevated, blood sodium decreased
- Postmarketing reports: Hypoglycemia[Ref]
Genitourinary
- Uncommon (0.1% to 1%): Worsening of preexisting proteinuria, urine output increased, transient erectile impotence
- Frequency not reported: Proteinuria, impotence[Ref]
Ocular
- Uncommon (0.1% to 1%): Visual disturbance, blurred vision[Ref]
Hematologic
- Uncommon (0.1% to 1%): Eosinophilia, hemoglobin or hematocrit decreased
- Rare (less than 0.1%): Neutropenia, agranulocytosis, white blood cell count decreased, red blood cell count decreased, platelet count decreased
- Frequency not reported: Pancytopenia, hemolytic anemia, thrombocytopenia, leucopenia, bone marrow failure[Ref]
Hepatic
- Uncommon (0.1% to 1%): Hepatic enzymes increased, conjugated bilirubin increased
- Rare (less than 0.1%): Cholestatic jaundice, hepatocellular damage
- Frequency not reported: Hepatic failure, hepatitis, jaundice, acute liver failure, hepatocellular damage, cholestatic hepatitis, cytolytic hepatitis, serum bilirubin elevated[Ref]
Immunologic
- Uncommon (0.1% to 1%): Angioneurotic edema, angioedema
- Very rare (less than 0.01%): Photosensitivity
- Frequency not reported: Anaphylactic reaction, anaphylactoid reaction, apparent hypersensitivity reaction, antinuclear antibody increased[Ref]
Endocrine
- Frequency not reported: Syndrome of inappropriate antidiuretic hormone secretion[Ref]
References
1. Cerner Multum, Inc. "UK Summary of Product Characteristics."
2. Cerner Multum, Inc. "Australian Product Information."
3. (2001) "Product Information. Altace (ramipril)." Hoechst Marion Roussel
Frequently asked questions
More about ramipril
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (135)
- Drug images
- Dosage information
- Patient tips
- During pregnancy
- Support group
- Drug class: Angiotensin Converting Enzyme Inhibitors
- Breastfeeding
- En español
Patient resources
Other brands
Professional resources
Other brands
Related treatment guides
Further information
Ramipril side effects can vary depending on the individual. Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
Note: Medication side effects may be underreported. If you are experiencing side effects that are not listed, submit a report to the FDA by following this guide.