medroxyPROGESTERone (Monograph)
Brand names: Depo-Provera, Depo-subQ provera 104, Provera
Drug class: Progestins
ATC class: G03AC06
VA class: HS800
Chemical name: (6α)-17-(Acetyloxy)-6-methyl-pregn-4-ene-3,20-dione
Molecular formula: C24H34O4
CAS number: 71-58-9
Warning
- Bone Mineral Density
-
Use of parenteral medroxyprogesterone preparations (i.e., Depo-Provera Contraceptive, depo-subQ provera 104, or medroxyprogesterone acetate contraceptive injection) may result in loss of bone mineral density (BMD). Bone loss is greater with increasing duration of therapy and may not be completely reversible.
-
Not known whether use of these parenteral preparations in young women (e.g., during adolescence, early adulthood) will reduce peak bone mass and increase risk of osteoporotic fractures later in life. Loss of BMD is of particular concern during adolescence and early adulthood, a critical period of bone accretion.
-
Use parenteral medroxyprogesterone for long-term contraception (e.g., >2 years) only if other contraceptive methods are inadequate.
Introduction
Synthetic progestin; derivative of 17 α-hydroxyprogesterone.
Uses for medroxyPROGESTERone
Prevention of Endometrial Changes Associated with Estrogens
Reduction of the incidence of endometrial hyperplasia and the attendant risk of endometrial carcinoma in postmenopausal women receiving estrogen replacement therapy.
Contraception in Females
Prevention of pregnancy.
Parenteral medroxyprogesterone: Consider benefits vs risks (e.g., loss of BMD in women of all ages, possible impact on peak bone mass in adolescents, additional impact of pregnancy and/or nursing on BMD). (See Boxed Warning and Effects on Bone under Cautions.)
Endometriosis
Management of pain associated with endometriosis. Benefit of therapy for >6 months not established. Consider benefits vs risk of BMD loss in women of all ages and the possible impact on peak bone mass in adolescents. (See Boxed Warning and Effects on Bone under Cautions.)
Amenorrhea
Treatment of secondary amenorrhea.
Uterine Bleeding
Treatment of abnormal uterine bleeding due to hormonal imbalance in the absence of organic pathology such as fibroids or uterine cancer.
Endometrial Carcinoma
Adjunctive therapy and palliative treatment of inoperable, recurrent, and metastatic endometrial carcinoma.
Renal Carcinoma
Has been used for treatment of metastatic renal cell carcinoma; however, other agents are preferred.
Paraphilia† [off-label] in Males
Management of paraphilia† [off-label] (e.g., homosexual, heterosexual, or bisexual pedophilia; heterosexual fetishism, voyeurism, sexual sadism, or exhibitionism; transvestism) in males.
Precocious Puberty† [off-label]
Management of GnRH-dependent (central) forms of precocious puberty† [off-label]; however, GnRH analogs generally are preferred.
Management of GnRH-independent (peripheral) forms of precocious puberty† [off-label], including familial male precocious puberty (testotoxicosis)† and McCune-Albright syndrome†.
medroxyPROGESTERone Dosage and Administration
Administration
Administer orally, IM, or sub-Q.
Oral Administration
Administer orally.
Oral dosage preparations containing medroxyprogesterone acetate in combination with conjugated estrogens USP as monophasic or biphasic regimens are commercially available in a mnemonic dispensing package that is designed to aid the user in complying with the prescribed dosage schedule.
IM Administration
Administer by IM injection deeply into gluteal, deltoid, or anterior thigh muscle.
Vigorously shake injectable suspension immediately before each use.
Sub-Q Administration
depo-subQ provera 104: Administer by sub-Q injection into anterior thigh or abdomen; not formulated for IM injection.
Vigorously shake injectable suspension before administration.
Dosage
Available as medroxyprogesterone acetate; dosage expressed in terms of the salt.
When used as a contraceptive or for the management of endometriosis, dosage does not need to be adjusted based on weight.
Adults
Prevention of Endometrial Changes Associated with Estrogens
Oral
1.5–5 mg daily. Alternatively, 5–10 mg daily for 12–14 consecutive days per month.
Contraception in Females
Medroxyprogesterone (Depo-Provera Contraceptive, medroxyprogesterone acetate contraceptive)
IM150 mg every 3 months. Exclude possibility of pregnancy before administering the first dose and whenever ≥13 weeks have elapsed since the previous dose. Initiate during the first 5 days of a normal menstrual cycle, at 6 weeks postpartum in women who breast-feed, or within 5 days postpartum in those who do not breast-feed.
Medroxyprogesterone/Estradiol Fixed Combination (Lunelle)
IMMedroxyprogesterone acetate 25 mg and estradiol cypionate 5 mg (0.5 mL) monthly (every 28–30 days; not to exceed 33 days). Initiate during the first 5 days of a normal menstrual cycle, within 5 days of a complete first-trimester abortion, no earlier than 6 weeks postpartum in women who breast-feed, or no earlier than 4 weeks postpartum in those who do not breast-feed.
If >33 days have elapsed since the previous injection, use an alternative (i.e., barrier) method of contraception and rule out pregnancy prior to continuing Lunelle. Shortening the injection interval may alter menstrual pattern.
When switching from other contraceptive methods, initiate Lunelle in a manner that ensures continuous contraceptive coverage based on the mechanism of action of both methods (e.g., patients switching from oral contraceptives should be given an initial injection within 7 days after taking the last hormonally active tablet).
Medroxyprogesterone (depo-subQ provera 104)
Sub-Q104 mg every 3 months (12–14 weeks). Exclude possibility of pregnancy before administering the first dose and whenever ≥14 weeks have elapsed since the previous dose. Initiate during the first 5 days of a normal menstrual cycle or ≥ 6 weeks postpartum in women who breast-feed.
When switching from other contraceptive methods, initiate depo-subQ provera 104 in a manner that ensures continuous contraceptive coverage based on the mechanism of action of both methods. Patients switching from combined contraceptives (estrogen plus progestin) should be given an initial injection within 7 days after taking the last hormonally active tablet or removing a transdermal patch or vaginal ring. Contraceptive coverage will be maintained when switching from medroxyprogesterone acetate contraceptive IM injection (e.g., Depo Provera contraceptive injection) to depo-subQ provera 104 if the next injection is given within the dosing period recommended for the IM contraceptive injection.
Endometriosis
Sub-Q
depo-subQ provera 104: 104 mg every 3 months (12–14 weeks). Exclude possibility of pregnancy before administering the first dose and whenever ≥14 weeks have elapsed since the previous dose. Initiate during the first 5 days of a normal menstrual cycle or ≥ 6 weeks postpartum in women who breast-feed.
Benefit of therapy for >6 months not established; treatment for >2 years not recommended. (See Effects on Bone under Cautions.)
Amenorrhea
Oral
5–10 mg daily for 5–10 days.
To induce optimum secretory transformation of an endometrium that has been adequately primed with endogenous or exogenous estrogen, 10 mg daily for 10 days.
Uterine Bleeding
Oral
5–10 mg daily for 5–10 days beginning on the assumed or calculated 16th or 21st day of the menstrual cycle.
To induce optimum secretory transformation of an endometrium that has been adequately primed with endogenous or exogenous estrogen, 10 mg daily for 10 days, beginning on the calculated 16th day of the menstrual cycle.
Endometrial Carcinoma
IM
Initially, 400–1000 mg once weekly. When improvement is noted and disease has stabilized (within weeks or months), maintain response with as little as 400 mg/month.
Renal Carcinoma
IM
Initially, 400–1000 mg once weekly. When improvement is noted and disease has stabilized (within weeks or months), maintain response with as little as 400 mg/month.
Paraphilia† in Males
IM
Initially, 200 mg 2 or 3 times daily. Alternatively, 500 mg once weekly.
Adjust dose and/or frequency to an effective maintenance level according to patient response and tolerance and/or plasma testosterone concentration. Consult published protocols for more specific dosage information in these males.
Cautions for medroxyPROGESTERone
Contraindications
-
Active thrombophlebitis, current or past history of thromboembolic disorders, or cerebrovascular disease.
-
Undiagnosed vaginal bleeding.
-
Known or suspected pregnancy.
-
Liver dysfunction or disease.
-
Known or suspected malignancy of the breast.
-
Known hypersensitivity to medroxyprogesterone or any ingredient in the formulation.
-
Use as a pregnancy test.
Warnings/Precautions
Warnings
Effects on Bone
When used IM or sub-Q as a contraceptive or sub-Q for the management of endometriosis, possible increased rate of bone loss, especially during initial years of therapy. Bone loss is greater with increasing duration of therapy; may not be reversible. (See Boxed Warning.)
Use as a long-term contraceptive (e.g., >2 years) only if other contraceptive methods are inadequate and benefits are expected to outweigh risks. Evaluate BMD periodically when used long term; consider patient’s age (adult or adolescent) and skeletal maturity when evaluating BMD results.
Consider other therapies in women with existing risk factors for osteoporosis, since use of medroxyprogesterone may pose additional risk.
When used for the management of endometriosis, evaluate BMD prior to initiating a second course of therapy.
Effects of BMD changes in women receiving medroxyprogesterone acetate in fixed combination with estradiol cypionate (Lunelle) not established.
Thromboembolic Disorders
Possible thromboembolic and thrombotic disorders (e.g., thrombophlebitis, pulmonary embolism, cerebrovascular insufficiency, coronary occlusion, retinal thrombosis, mesenteric thrombosis). Observe patients for these effects; discontinue immediately and do not readminister if these disorders occur or are suspected.
Bleeding Irregularities
When used as a contraceptive, possible breakthrough or irregular vaginal bleeding; rarely may be heavy or continuous. If abnormal bleeding persists or is severe, consider organic pathology and perform adequate diagnostic tests in patients with undiagnosed vaginal bleeding.
Carcinoma of Reproductive Organs and Breast
Depo-Provera contraceptive injection associated with slight or no increased risk of breast cancer; no increase in risk of ovarian or cervical cancer, reduced risk of endometrial cancer.
When used with estrogen replacement therapy in postmenopausal women, reduced risk of endometrial cancer compared with estrogen use alone. Perform diagnostic tests (including endometrial sampling) in women with undiagnosed, persistent, or abnormal vaginal bleeding.
Addition of medroxyprogesterone to estrogen replacement therapy increases the risk of breast cancer beyond that associated with estrogen use alone.
Fetal/Neonatal Morbidity and Mortality
Potential adverse effects on the fetus when administered within the first 4 months of pregnancy (masculinization of the female fetus, hypospadias in male neonates, low birth weight). (See Contraindications under Cautions.)
Ectopic Pregnancy
Consider the possibility of ectopic pregnancy if pregnancy or severe abdominal pain occurs in women using medroxyprogesterone contraception.
Ocular Effects
If unexplained, sudden or gradual, partial or complete loss of vision; proptosis or diplopia; papilledema; or retinal vascular lesions occur, discontinue and initiate appropriate diagnostic and therapeutic measures. Do not reinitiate therapy if ocular examination reveals evidence of papilledema or retinal vascular lesions.
Sensitivity Reactions
Hypersensitivity Reactions
Anaphylaxis and anaphylactoid reactions reported. Institute appropriate measures if anaphylactic/anaphylactoid reaction occurs.
Possible allergic reactions, including urticaria, pruritus, angioedema, generalized rash (with or without pruritus).
General Precautions
Physical Examination and Follow-up
Annual medical history and physical examination advised. Physical examination may be deferred until after initiation of parenteral medroxyprogesterone if requested by the woman and judged appropriate by the clinician. Physical examination should include special attention to BP, breasts, abdomen, and pelvic organs and should include a Papanicolaou test (Pap smear) and relevant laboratory tests. Exercise particular care in women with a strong family history of breast cancer or those who have breast nodules.
Fluid Retention
Fluid retention may occur. Exercise caution and carefully monitor patients with conditions (seizures, migraine headache, asthma, cardiac impairment, renal impairment) that might be aggravated by fluid retention.
Weight Change
Possible weight gain.
Fertility
Contraceptive effect is prolonged. Median time to conception after the last dose of parenteral medroxyprogesterone (Depo-Provera Contraceptive Injection) is 10 months (range: 4–31 months) and is unrelated to the duration of contraceptive use.
Median time to ovulation was 10 months after last injection of depo-subQ provera 104 and 80% of women ovulated within 1 year; ovulation may occur as early as 14 weeks after a single dose.
Depression
Possible depression. Exercise caution in women with a history of depression; discontinue if severe depression recurs during use.
Seizures
Seizures reported with IM contraceptive use.
Injection Site Reactions
Injection site reactions, including persistent skin changes (e.g., small areas of induration or atrophy), reported with sub-Q administration.
Sexually Transmitted Diseases
Does not protect against HIV or other sexually transmitted infections.
Endocrine and Metabolic Effects
Possible decreased glucose tolerance. Monitor diabetic patients carefully.
Prolonged Therapy
Effect of long-term therapy on pituitary, ovarian, adrenal, hepatic, or uterine function not determined.
Climacteric
Onset of climacteric may be masked in women.
Hepatic Effects
Possible hepatic dysfunction (e.g., jaundice); discontinue therapy and reevaluate patient if such manifestations occur or are suspected.
Estrogen Therapy
Medroxyprogesterone may adversely affect some beneficial estrogen-associated metabolic effects (lipid metabolism, glucose tolerance).
When used in fixed combination with conjugated estrogens or estradiol cypionate, consider the cautions, precautions, and contraindications associated with estrogens.
Specific Populations
Pregnancy
Category X. (See Contraindications and also Fetal/Neonatal Morbidity and Mortality, under Cautions.)
Lactation
Distributed into milk. No evidence of adverse developmental or behavioral effects through puberty found in infants exposed to the drug via breast milk.
Pediatric Use
Safety and efficacy not established.
Not indicated before menarche. Possible loss of BMD with parenteral medroxyprogesterone; loss of BMD is of particular concern during adolescence. (See Boxed Warning and Effects on Bone under Cautions.)
Safety and efficacy of parenteral medroxyprogesterone in postmenarchal adolescents expected to be the same as in adult women.
Hepatic Impairment
Contraindicated in patients with liver dysfunction or disease.
Common Adverse Effects
Menstrual abnormalities (amenorrhea; frequent, irregular, prolonged, or infrequent bleeding), abdominal pain or discomfort, weight changes, dizziness, headache, asthenia, nervousness.
Drug Interactions
Specific Drugs
|
Drug |
Interaction |
Comment |
|---|---|---|
|
Aminoglutethimide |
Decreased medroxyprogesterone concentrations |
Decreased efficacy with concomitant use |
medroxyPROGESTERone Pharmacokinetics
Absorption
Bioavailability
Rapidly absorbed from the GI tract; peak plasma concentrations achieved within 2–4 hours.
Peak plasma concentrations attained approximately 1 week following sub-Q injection.
Food
Food increases peak plasma concentrations and AUC.
Distribution
Extent
Distributed into human milk.
Plasma Protein Binding
Approximately 86–90% (primarily albumin).
Elimination
Metabolism
Metabolized in the liver by ring A and/or side-chain hydroxylation.
Elimination Route
Excreted in urine, principally as glucuronide conjugates.
Half-life
Oral doses: Approximately 12 hours (single dose) or 17 hours (multiple doses).
IM doses: 50 days reported for Depo-Provera Contraceptive Injection; 15 days reported for Lunelle Monthly Contraceptive Injection.
Sub-Q doses: approximately 40 days for depo-subQ provera 104.
Special Populations
In patients with advanced liver disease, clearance is reduced.
Stability
Storage
Oral
Tablets
20–25°C.
Parenteral
Injection
20–25°C.
Actions
-
Transforms a proliferative endometrium into a secretory one.
-
Androgenic and anabolic effects have been reported; no estrogenic activity reported.
-
At usual IM or sub-Q dosages, inhibits secretion of pituitary gonadotropins, preventing follicular maturation and ovulation and resulting in endometrial thinning. These actions produce a contraceptive effect. Usual oral dosages do not exhibit these effects.
Advice to Patients
-
Importance of women informing clinicians immediately if they are or plan to become pregnant. Necessity for clinicians to advise pregnant women of the risk to fetus.
-
Importance of reading the manufacturer’s patient information.
-
Importance of advising patients of anticipated menstrual effects.
-
Importance of patients notifying their clinician if signs and symptoms of thromboembolic and thrombotic disorders occur.
-
When used as a contraceptive, importance of adhering to the injection schedule.
-
Importance of women informing clinicians if they are breast-feeding or plan to breast-feed.
-
Importance of informing patients of other important precautionary information. (See Cautions.)
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
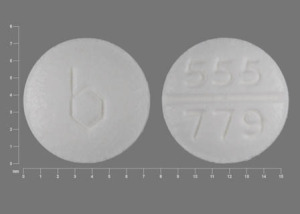
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Tablets |
2.5 mg* |
Provera (scored) |
Pfizer |
|
Medroxyprogesterone Acetate Tablets |
Barr |
|||
|
5 mg* |
Provera (scored) |
Pfizer |
||
|
Medroxyprogesterone Acetate Tablets |
Barr |
|||
|
10 mg* |
Provera (scored) |
Pfizer |
||
|
Parenteral |
Injectable suspension |
104 mg/0.65 mL |
depo-subQ provera 104 (with parabens and povidone, available in prefilled syringes with UltraSafe Passive needle guard) |
Pfizer |
|
150 mg/mL* |
Depo-Provera Contraceptive (with parabens) |
Pfizer |
||
|
Medroxyprogesterone Acetate Contraceptive |
Sicor |
|||
|
400 mg/mL |
Depo-Provera |
Pfizer |
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Tablets, monophasic regimen |
1.5 mg with Conjugated Estrogens 0.3 mg (28 tablets) |
Prempro (with povidone) |
Wyeth |
|
1.5 mg with Conjugated Estrogens 0.45 mg (28 tablets) |
Prempro (with povidone) |
Wyeth |
||
|
2.5 mg with Conjugated Estrogens 0.625 mg (28 tablets) |
Prempro (with povidone) |
Wyeth |
||
|
5 mg with Conjugated Estrogens 0.625 mg (28 tablets) |
Prempro (with povidone) |
Wyeth |
||
|
Tablets, biphasic regimen |
5 mg with Conjugated Estrogens 0.625 mg (14 tablets) and Conjugated Estrogens 0.625 mg (14 tablets) |
Premphase (with povidone) |
Wyeth |
|
|
Parenteral |
Injectable Suspension |
25 mg/0.5 mL with Estradiol Cypionate 5 mg/0.5 mL |
Lunelle Monthly Contraceptive Injection |
Pfizer |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions August 1, 2005. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
† Off-label: Use is not currently included in the labeling approved by the US Food and Drug Administration.
Reload page with references included
Related/similar drugs
Frequently asked questions
More about medroxyprogesterone
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (2,474)
- Drug images
- Side effects
- Dosage information
- During pregnancy
- Support group
- Drug class: contraceptives
- Breastfeeding
Patient resources
Professional resources
- Medroxyprogesterone prescribing information
- Medroxyprogesterone Injection (FDA)
- Medroxyprogesterone Injection ER (FDA)
Other brands
Provera, Depo Provera, depo-subQ provera 104