Diflunisal Dosage
Medically reviewed by Drugs.com. Last updated on Oct 24, 2024.
Applies to the following strengths: 250 mg; 500 mg; 375 mg
Usual Adult Dose for:
Usual Pediatric Dose for:
Additional dosage information:
Usual Adult Dose for Pain
Initial dose: 1000 mg orally once
Maintenance dose: 500 mg every 12 hours; some patients may require 500 mg every 8 hours
Maximum dose: 1500 mg/day
Comments: A lower dose may be appropriate depending on such factors as pain severity, patient response, weight, or advanced age; for example, 500 mg initially, followed by 250 mg every 8 to 12 hours.
Use: For the treatment of mild to moderate pain
Usual Adult Dose for Osteoarthritis
500 to 1000 mg orally per day in 2 divided doses
Comments:
- Dosage may be increased or decreased based on patient response.
- Not to exceed 1500 mg/day.
Uses: For the treatment of osteoarthritis and rheumatoid arthritis
Usual Adult Dose for Rheumatoid Arthritis
500 to 1000 mg orally per day in 2 divided doses
Comments:
- Dosage may be increased or decreased based on patient response.
- Not to exceed 1500 mg/day.
Uses: For the treatment of osteoarthritis and rheumatoid arthritis
Usual Pediatric Dose for Pain
12 years or older:
- Initial dose: 1000 mg orally once
- Maintenance dose: 500 mg every 12 hours; some patients may require 500 mg every 8 hours
- Maximum dose: 1500 mg/day
Comments: A lower dose may be appropriate depending on such factors as pain severity, patient response, weight, or advanced age; for example, 500 mg initially, followed by 250 mg every 8 to 12 hours.
Use: For the treatment of mild to moderate pain
Usual Pediatric Dose for Osteoarthritis
12 years or older: 500 to 1000 mg orally per day in 2 divided doses
Comments:
- Dosage may be increased or decreased based on patient response.
- Not to exceed 1500 mg/day.
Uses: For the treatment of osteoarthritis and rheumatoid arthritis
Usual Pediatric Dose for Rheumatoid Arthritis
12 years or older: 500 to 1000 mg orally per day in 2 divided doses
Comments:
- Dosage may be increased or decreased based on patient response.
- Not to exceed 1500 mg/day.
Uses: For the treatment of osteoarthritis and rheumatoid arthritis
Renal Dose Adjustments
Advanced renal dysfunction: Not recommended; if therapy is necessary, closely monitor renal function.
Liver Dose Adjustments
- Patients who have an abnormal liver test or who develop signs or symptoms of liver dysfunction should be evaluated for a more severe hepatic reaction.
- If liver disease develops or if systemic manifestations such as eosinophilia or rash occur, this drug should be discontinued.
Dose Adjustments
Elderly patients may require lower doses due to increased risk for adverse effects and increased likelihood of concomitant renal impairment.
Precautions
US BOXED WARNINGS: RISK OF SERIOUS CARDIOVASCULAR AND GASTROINTESTINAL EVENTS:
- Nonsteroidal anti-inflammatory drugs (NSAIDs) cause an increased risk of serious cardiovascular (CV) thrombotic events, myocardial infarction, and stroke, which can be fatal. This risk may increase with duration of use. Patients with cardiovascular disease or risk factors for cardiovascular disease may be at greater risk.
- This drug is contraindicated for the treatment of perioperative pain in the setting of coronary artery bypass graft (CABG) surgery.
- NSAIDs cause an increased risk of serious gastrointestinal (GI) adverse events including bleeding, ulceration, and perforation of the stomach or intestines, which can be fatal. These events can occur at any time during use and without warning symptoms. Elderly patients are at greater risk for serious GI events.
Safety and efficacy have not been established in patients younger than 12 years.
Consult WARNINGS section for additional precautions.
Dialysis
Data not available
Other Comments
Administration advice:
- Swallow tablets whole; do not crush or chew.
General:
- Concentration-dependent pharmacokinetics prevail with this drug; a doubling of dosage produces a greater than doubling of drug accumulation and effects become more apparent with repetitive doses.
- Following initial response to therapy, dose and frequency should be adjusted to suit individual patient needs.
- Prior to initiating treatment, the potential benefits and risks of this drug should be weighed against other treatment options.
- The lowest effective dose for the shortest duration consistent with individual patient treatment goals should be used.
- There is an increased risk of heart attack, heart failure, and stroke when taking nonsteroidal anti-inflammatory drugs (NSAIDs); these events may occur at any time during treatment and risk increases with long term use, a history of cardiovascular (CV) disease or risk factors for CV disease, and higher doses.
Monitoring:
- Cardiovascular: Monitor blood pressure closely during initiation and throughout the course of therapy.
- Gastrointestinal: Monitor for signs/symptoms of gastrointestinal bleeding.
- Renal function: Monitor renal status, especially in patients with conditions where renal prostaglandins have a supportive role in the maintenance of renal perfusion.
- Monitor blood counts, renal, and hepatic function periodically for patients receiving long-term therapy.
Patient advice:
- Patients should seek medical advice for signs and symptoms of gastrointestinal events, adverse skin reactions, allergic reactions, hepatotoxicity, or unexplained weight gain or edema.
- Patients should seek medical attention immediately if signs/symptoms of cardiovascular events occur including, shortness of breath, slurred speech, chest pain, or weakness on one side of the body.
- Patients should talk to their health care provider if they are pregnant, planning to become pregnant, or breastfeeding; NSAIDs should not be used at 20 weeks or later in pregnancy unless specifically advised to do so by their health care professional.
More about diflunisal
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (8)
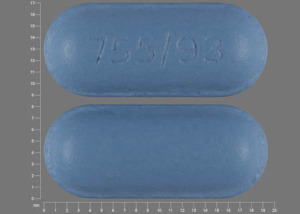
- Drug images
- Latest FDA alerts (4)
- Side effects
- During pregnancy
- Drug class: Nonsteroidal anti-inflammatory drugs
- Breastfeeding
- En español
Patient resources
Other brands
Professional resources
Other brands
Related treatment guides
See also:
Plaquenil
Plaquenil is used to treat or prevent malaria and to treat the symptoms of rheumatoid arthritis ...
Enbrel
Enbrel is used to treat rheumatoid arthritis, ankylosing spondylitis, and psoriasis. Learn about ...
Humira
Humira is a tumor necrosis factor blocker used to treat many inflammatory conditions in adults ...
Remicade
Remicade is used to treat rheumatoid arthritis, psoriatic arthritis, ulcerative colitis and Crohn's ...
Rituxan
Rituxan infusion is used to treat certain leukemias and lymphomas and some non-cancer conditions ...
Orencia
Orencia is a type of biologic that is given by intravenous infusion or subcutaneous injection which ...
Rituximab
Rituximab infusion is used to treat certain leukemias and lymphomas and some non-cancer conditions ...
Adalimumab
Adalimumab is used to treat plaque psoriasis, Crohn's disease, ulcerative colitis, rheumatoid ...
Leflunomide
Leflunomide is used for psoriatic arthritis, rheumatoid arthritis
Sulfasalazine
Sulfasalazine is used to treat ulcerative colitis, rheumatoid arthritis, and polyarticular-course ...
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.