Tipranavir Side Effects
Medically reviewed by Drugs.com. Last updated on Mar 11, 2025.
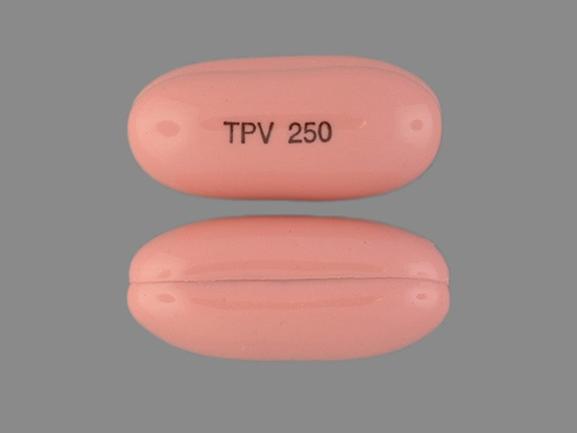
Applies to tipranavir: oral capsule liquid filled.
Important warnings
This medicine can cause some serious health issues
Oral route (capsule; solution)
Hepatotoxicity and Intracranial Hemorrhage. Clinical hepatitis and hepatic decompensation including some fatalities, have been reported.
Extra vigilance is warranted in patients with chronic hepatitis B or hepatitis C co-infection.Fatal and non-fatal intracranial hemorrhage have been reported
Precautions
It is very important that your doctor check the progress of you or your child at regular visits to make sure that this medicine is working properly. Blood tests may be needed to check for unwanted effects.
Do not take other medicines unless they have been discussed with your doctor. This includes prescription or nonprescription (over-the-counter [OTC]) medicines and herbal (eg, St. John's wort) or vitamin supplements.
You should not use tipranavir together with alfuzosin (Uroxatral®), amiodarone (Cordarone®, Pacenone®), bepridil (Vascor®), cisapride (Propulsid®), ergot medicines (eg, dihydroergotamine, ergonovine, ergotamine, methylergonovine, Cafergot®, Methergine®, Migranal®), flecainide (Tambocor®), lovastatin (Altocor®, Mevacor®), oral lurasidone (Latuda®), midazolam (Versed®) pimozide (Orap®), propafenone (Rythmol®), quinidine (Cardioquin®, Quinaglute Dura®), rifampin (Rifadin®, Rimactane®), sildenafil (Revatio®), simvastatin (Simcor®, Vytorin®, Zocor®), or triazolam (Halcion®). Using these medicines together with tipranavir may increase your chance of having serious medical problems.
This medicine may decrease the effects of some oral contraceptives (birth control pills). To keep from getting pregnant, use an additional form of birth control with your pills. Other forms include condoms, a diaphragm, or contraceptive foam or jelly.
This medicine may cause intracranial hemorrhage (bleeding in the brain). Make sure your doctor knows if you or your child have a bleeding disorder, or any medical condition that increases your chance of bleeding. Call your doctor right away if you have any unusual or unexplained bleeding.
Check with your doctor right away if you or your child have pain in the upper stomach, pale stools, dark urine, loss of appetite, nausea, unusual tiredness or weakness, or yellow eyes or skin. These could be symptoms of a serious liver problem.
When you start taking HIV medicines, your immune system may get stronger. If you have certain infections that are hidden in your body, such as pneumonia or tuberculosis, you or your child may notice new symptoms when your body tries to fight them. If this occurs, tell your doctor right away.
Serious skin reactions can occur with this medicine. Check with your doctor right away if you or your child have more than one of the following symptoms while using this medicine: blistering, peeling, or loosening of the skin, fever or chills, itching, joint or muscle pain, severe rash, red skin lesions, sunburn, throat tightness, or sores, ulcers, or white spots in the mouth or on the lips.
This medicine may make your skin more sensitive to sunlight. Use a sunscreen when you are outdoors. Wear protective clothing and hats. Avoid sunlamps and tanning beds.
This medicine may cause you to have excess body fat. Tell your doctor if you or your child notice changes in your body shape, such as an increased amount of fat in the upper back and neck, or around the chest and stomach area, or a loss of fat from the legs, arms, and face.
Common side effects of tipranavir
Some side effects of tipranavir may occur that usually do not need medical attention. These side effects may go away during treatment as your body adjusts to the medicine. Also, your health care professional may be able to tell you about ways to prevent or reduce some of these side effects.
Check with your health care professional if any of the following side effects continue or are bothersome or if you have any questions about them:
More common side effects
- diarrhea
Less common side effects
- abdominal or stomach pain
- cough
- discouragement
- fat redistribution
- feeling sad or empty
- irritability
- lack of appetite
- lack or loss of strength
- loss of interest or pleasure
- rash
- trouble concentrating
- trouble sleeping
Serious side effects of tipranavir
Along with its needed effects, tipranavir may cause some unwanted effects. Although not all of these side effects may occur, if they do occur they may need medical attention.
Check with your doctor immediately if any of the following side effects occur while taking tipranavir:
Less common side effects
- bleeding gums
- confusion
- cough producing mucus
- coughing up blood
- difficulty with breathing or swallowing
- dizziness
- fever
- general feeling of tiredness or weakness
- headache
- increased menstrual flow or vaginal bleeding
- loss of appetite
- nausea or vomiting
- nosebleeds
- paralysis
- prolonged bleeding from cuts
- red or black, tarry, or light-colored stools
- red or dark brown urine
- sudden severe weakness
- tightness in the chest
- unusual bleeding
- upper right abdominal or stomach pain
- yellow eyes and skin
See also:
For healthcare professionals
Applies to tipranavir: oral capsule, oral solution.
General adverse events
The most frequent side effects reported in clinical trials with this drug (plus ritonavir) were diarrhea/loose stools, nausea, fatigue, headache, vomiting, pyrexia, abdominal pain, and hyperlipidemia. Therapy was discontinued due to side effects in 13.3% of patients using tipranavir/ritonavir and 10.8% of patients using the comparator.
The manufacturer product information for ritonavir should be consulted.[Ref]
Metabolic
- Very common (10% or more): Elevated triglycerides (up to 35.9%), elevated cholesterol (up to 15.6%)
- Common (1% to 10%): Hypertriglyceridemia, hyperlipidemia, dehydration, decreased appetite
- Uncommon (0.1% to 1%): Anorexia, diabetes mellitus, hyperamylasemia, hypercholesterolemia, hyperglycemia
- Frequency not reported: Mitochondrial toxicity, porphyria cutanea tarda
Antiretroviral therapy:
- Frequency not reported: Redistribution/accumulation of body fat (including central obesity, dorsocervical fat enlargement, peripheral wasting, facial wasting, breast enlargement, "cushingoid appearance"), increased blood lipid levels, increased glucose levels
Protease inhibitor therapy:
- Postmarketing reports: New onset diabetes mellitus, exacerbation of preexisting diabetes mellitus, hyperglycemia, diabetic ketoacidosis[Ref]
Elevated triglycerides (grade 2 [400 to 750 mg/dL]: 35.9%; grade 3 [greater than 750 to 1200 mg/dL]: 16.9%; grade 4 [greater than 1200 mg/dL]: 8%) and cholesterol (grade 2 [greater than 300 to 400 mg/dL]: 15.6%; grade 3 [greater than 400 to 500 mg/dL]: 3.3%; grade 4 [greater than 500 mg/dL]: 0.9%) have been reported at 48 weeks in controlled trials.[Ref]
Hepatic
- Very common (10% or more): Elevated ALT and/or AST (up to 32.1%), increased hepatic transaminases (up to 20.3%), elevated ALT (up to 14.9%)
- Common (1% to 10%): Elevated AST, elevated GGT
- Uncommon (0.1% to 1%): Increased hepatic enzymes, cytolytic hepatitis, abnormal liver function tests, hepatitis, toxic hepatitis, hepatic steatosis
- Rare (less than 0.1%): Hepatic failure (including fatalities), hyperbilirubinemia
- Frequency not reported: Clinical hepatitis, hepatic decompensation, liver toxicity, hepatic impairment[Ref]
Grade 2 to 4 ALT and/or AST elevations (greater than 2.5 times the upper limit of normal [2.5 x ULN]: 26%), ALT elevations (grade 2 [greater than 2.5 to 5 x ULN]: 14.9%; grade 3 [greater than 5 to 10 x ULN]: 5.6%; grade 4 [greater than 10 x ULN]: 4.1%), and AST elevations (grade 2: 9.9%; grade 3: 4.5%; grade 4: 1.6%) have been reported at 48 weeks in controlled trials. In controlled clinical trials continued up to 96 weeks, 32.1% of patients developed grade 2 to 4 ALT and/or AST elevations.
Grade 3 and 4 hepatic transaminase elevations were reported in 10.3% of therapy-experienced patients in 2 large studies and in 20.3% of therapy-naive patients in 1 study; the studies were through 48 weeks. Elevated ALT or AST at baseline and hepatitis B or C coinfection were risk factors for such elevations in the 2 large studies; most patients were able to continue therapy with this drug (plus ritonavir).
Clinical hepatitis and hepatic decompensation (including some fatalities) have been reported with this drug (plus ritonavir); generally in patients with advanced HIV-1 disease taking multiple concomitant medications.
Significant liver toxicity has been reported with this drug (plus ritonavir). In at least 2 clinical trials, the frequency of transaminase elevations was significantly increased with this drug (plus ritonavir) compared to the comparator.[Ref]
Gastrointestinal
- Very common (10% or more): Diarrhea (15%), nausea
- Common (1% to 10%): Vomiting, elevated amylase, abdominal pain, upper abdominal pain, abdominal distension, dyspepsia, flatulence, elevated lipase
- Uncommon (0.1% to 1%): Gastroesophageal reflux disease, pancreatitis[Ref]
Elevated amylase (grade 3 [greater than 2.5 x ULN]: 5.7%; grade 4 [greater than 5 x ULN]: 0.3%) has been reported at 48 weeks in controlled trials.[Ref]
Dermatologic
- Common (1% to 10%): Rash (including with joint pain/stiffness, throat tightness, generalized pruritus, myalgia, fever, erythema, desquamation, mucosal erosions), pruritus
- Uncommon (0.1% to 1%): Exanthem, lipoatrophy, lipohypertrophy, acquired lipodystrophy
- Rare (less than 0.1%): Facial wasting
- Frequency not reported: Urticarial rash, maculopapular rash, photosensitivity (possible), rash (with joint pain/stiffness, throat tightness, generalized pruritus[Ref]
Rash (including urticarial rash, maculopapular rash, and possible photosensitivity) has been reported in 8% of males and 10% of females using this drug (plus ritonavir) through 48 weeks of therapy. The time to onset and duration of rash averaged 53 and 22 days, respectively. Some cases of rash occurred in conjunction with joint pain or stiffness, throat tightness, and generalized pruritus. Cases of rash (some severe) with myalgia, fever, erythema, desquamation, and mucosal erosions have been reported. Rash has been reported more often in pediatric patients than in adults.[Ref]
Hematologic
- Common (1% to 10%): Decreased WBC counts, anemia, neutropenia
- Uncommon (0.1% to 1%): Thrombocytopenia
- Frequency not reported: Bleeding event (not otherwise specified)
Protease inhibitor therapy:
- Frequency not reported: Increased bleeding (including spontaneous skin hematomas, hemarthrosis) in hemophiliacs[Ref]
Decreased WBC count (grade 3 [less than 2000/mcL]: 5.4%; grade 4 [less than 1000/mcL]: 0.3%) has been reported at 48 weeks in controlled trials.
Increased bleeding (including spontaneous skin hematomas and hemarthrosis) in patients with hemophilia type A and B has been associated with protease inhibitors. In many of the reported cases, treatment with protease inhibitors was continued or restarted and some patients required additional factor VIII. A causal relationship between protease inhibitor therapy and these episodes has not been established.[Ref]
Musculoskeletal
- Common (1% to 10%): Myalgia
- Uncommon (0.1% to 1%): Muscle spasms
- Frequency not reported: Muscle cramps, elevated creatine phosphokinase (CPK)
Combination antiretroviral therapy:
- Frequency not reported: Osteonecrosis
Protease inhibitor therapy:
- Rare (less than 0.1%): Rhabdomyolysis
- Frequency not reported: Increased CPK, myalgia, myositis[Ref]
Nervous system
- Common (1% to 10%): Headache, peripheral neuropathy
- Uncommon (0.1% to 1%): Dizziness, somnolence, intracranial hemorrhage
- Frequency not reported: Cerebrovascular accident[Ref]
Cases of fatal and nonfatal intracranial hemorrhage have been reported with this drug (plus ritonavir). Many of the patients had other medical conditions or were using concomitant medications that may have contributed to or caused these events. No pattern of abnormal hematologic or coagulation parameters was observed in patients in general or preceding development of intracranial hemorrhage.
An increased risk of intracranial hemorrhage was previously observed in patients with advanced HIV disease/AIDS, such as those treated in clinical trials with this drug.[Ref]
Other
- Common (1% to 10%): Pyrexia, fatigue, decreased weight
- Uncommon (0.1% to 1%): Influenza-like illness, malaise
- Frequency not reported: Asthenia, reactivation of herpes simplex, reactivation of varicella zoster, sepsis
Antiretroviral therapy:
- Frequency not reported: Increased weight[Ref]
Psychiatric
- Common (1% to 10%): Insomnia
- Uncommon (0.1% to 1%): Sleep disorder
- Frequency not reported: Depression[Ref]
Respiratory
- Common (1% to 10%): Dyspnea
- Frequency not reported: Bronchitis, cough, nasopharyngitis, upper respiratory tract infection, pneumonia, epistaxis[Ref]
Hypersensitivity
- Uncommon (0.1% to 1%): Hypersensitivity reactions[Ref]
Renal
- Uncommon (0.1% to 1%): Renal failure
- Frequency not reported: Renal insufficiency[Ref]
Immunologic
- Frequency not reported: Immune reconstitution/reactivation syndrome, autoimmune disorders in the setting of immune reconstitution (e.g., Graves' disease, polymyositis, Guillain-Barre syndrome)[Ref]
References
1. (2005) "Product Information. Aptivus (tipranavir)." Boehringer-Ingelheim
2. Cerner Multum, Inc. "UK Summary of Product Characteristics."
3. Dong BJ, Cocohoba JM (2006) "Tipranavir: a protease inhibitor for HIV salvage therapy." Ann Pharmacother, 40, 1311-21; quiz 1491-2
4. King JR, Acosta EP (2006) "Tipranavir : A Novel Nonpeptidic Protease Inhibitor of HIV." Clin Pharmacokinet, 45, p. 665-82
5. Piacenti FJ (2006) "An update and review of antiretroviral therapy." Pharmacotherapy, 26, p. 1111-33
6. Hammer SM, Saag MS, Schechter M, et al. (2006) "Treatment for adult HIV infection: 2006 recommendations of the International AIDS Society-USA panel." JAMA, 296, p. 827-43
7. Cahn P, Villacian J, Lazzarin A, et al. (2006) "Ritonavir-Boosted Tipranavir Demonstrates Superior Efficacy to Ritonavir-Boosted Protease Inhibitors in Treatment-Experienced HIV-Infected Patients: 24-Week Results of the RESIST-2 Trial." Clin Infect Dis, 43, p. 1347-56
8. Gathe J, Cooper DA, Farthing C, et al. (2006) "Efficacy of the Protease Inhibitors Tipranavir plus Ritonavir in Treatment-Experienced Patients: 24-Week Analysis from the RESIST-1 Trial." Clin Infect Dis, 43, p. 1337-46
9. Chen L, Sabo JP, Philip E, et al. (2007) "Steady state disposition of the nonpeptidic protease inhibitor tipranavir when coadministered with ritonavir." Antimicrob Agents Chemother, 51, p. 2436-44
10. Hoffman CJ, Gallant JE (2007) "When and how to use tipranavir and darunavir." AIDS Read, 17, 194-8, 201
11. Celesia BM, Onorante A, Nunnari G, et al. (2007) "Porphyria cutanea tarda in an HIV-1-infected patient after the initiation of tipranavir/ritonavir: case report." AIDS, 21, p. 1495-6
12. Temesgen Z, Feinberg J (2007) "Tipranavir: a new option for the treatment of drug-resistant HIV infection." Clin Infect Dis, 45, p. 761-9
13. Warnke D, Barreto J, Temesgen Z (2007) "Antiretroviral drugs." J Clin Pharmacol, 47, p. 1570-9
14. Cerner Multum, Inc. "Australian Product Information."
15. Orman JS, Perry CM (2008) "Tipranavir: A Review of its Use in the Management of HIV Infection." Drugs, 68, p. 1435-63
16. Lind L (2006) "Systolic and diastolic hypertension impair endothelial vasodilatory function in different types of vessels in the elderly: the Prospective Investigation of the Vasculature in Uppsala Seniors (PIVUS) study." J Hypertens, 24, p. 1319-27
17. Bergersen BM (2006) "Cardiovascular Risk in Patients with HIV Infection : Impact of Antiretroviral Therapy." Drugs, 66, p. 1971-87
18. Chapman SJ, Woolley IJ, Visvanathan K, Korman TM (2007) "Acute pancreatitis caused by tipranavir/ritonavir-induced hypertriglyceridaemia." AIDS, 21, p. 532-533
19. Panel on Antiretroviral Guidelines for Adults and Adolescents (2015) Guidelines for the use of antiretroviral agents in HIV-1-infected adults and adolescents. Department of Health and Human Services. https://aidsinfo.nih.gov/contentfiles/lvguidelines/adultandadolescentgl.pdf
20. AIDSinfo. NIH. National Institutes of Health (2016) Guidelines for the Use of Antiretroviral Agents in Pediatric HIV Infection. https://aidsinfo.nih.gov/contentfiles/lvguidelines/pediatricguidelines.pdf
21. Julg B, Bogner J, Goebel F (2006) "Severe hepatotoxicity associated with the combination of enfuvirtide and tipranavir/ritonavir: case report." AIDS, 20, p. 1563
22. Soriano V, Puoti M, Sulkowski M, et al. (2007) "Care of patients coinfected with HIV and hepatitis C virus: 2007 updated recommendations from the HCV-HIV International Panel." AIDS, 21, p. 1073-89
23. (2004) "Anti-HIV agents. Unexpected results from a tipranavir study." TreatmentUpdate, 16, p. 6-7
24. Borras-Blasco J, Navarro-Ruiz A, Borras C, Castera E (2008) "Adverse cutaneous reactions associated with the newest antiretroviral drugs in patients with human immunodeficiency virus infection." J Antimicrob Chemother, 62, p. 879-88
25. Justice AC, Zingmond DS, Gordon KS, et al. (2008) "Drug toxicity, HIV progression, or comorbidity of aging: does tipranavir use increase the risk of intracranial hemorrhage?" Clin Infect Dis, 47, p. 1226-30
More about tipranavir
- Check interactions
- Compare alternatives
- Dosage information
- During pregnancy
- Drug class: protease inhibitors
- Breastfeeding
- En español
Patient resources
Other brands
Professional resources
Other brands
Related treatment guides
Further information
Tipranavir side effects can vary depending on the individual. Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
Note: Medication side effects may be underreported. If you are experiencing side effects that are not listed, submit a report to the FDA by following this guide.