Nitazoxanide (Monograph)
Brand name: Alinia
Drug class: Antiprotozoals, Cryptosporidiosis
Chemical name: 2-acetyloxy-N-(5-nitro-2-thiazolyl)benzamide
Molecular formula: C12H9N3 O5 S
CAS number: 55981-09-4
Introduction
Antiprotozoal; nitrothiazolyl-salicylamide derivative.
Uses for Nitazoxanide
Cryptosporidiosis
Treatment of diarrhea caused by Cryptosporidium parvum in immunocompetent adults, adolescents, and children ≥1 year of age. Designated an orphan drug by FDA for treatment of cryptosporidiosis.
Recommended as drug of choice for treatment of cryptosporidiosis.
Although safety and efficacy not established for treatment of diarrhea caused by C. parvum in HIV-infected or other immunodeficient patients, nitazoxanide has been used for treatment of cryptosporidiosis in such individuals. CDC, NIH, IDSA, and others state that the most appropriate treatment for cryptosporidiosis in HIV-infected individuals is potent antiretroviral therapy (to restore immune function) and supportive care and symptomatic treatment of diarrhea. These experts state that adjunctive use of nitazoxanide can be considered for treatment of cryptosporidiosis in HIV-infected adults, adolescents, or children† [off-label] receiving effective antiretroviral therapy; however, do not use nitazoxanide in HIV-infected patients not receiving antiretroviral therapy.
Giardiasis
Treatment of diarrhea caused by Giardia intestinalis (also known as G. lamblia or G. duodenalis) in immunocompetent adults, adolescents, and children ≥1 year of age. Designated an orphan drug by FDA for treatment of intestinal giardiasis.
Metronidazole, tinidazole, and nitazoxanide are the drugs of choice for treatment of giardiasis; alternatives include paromomycin (especially in pregnant women), furazolidone (no longer commercially available in US), or quinacrine (not commercially available in US).
Safety and efficacy not established for treatment of diarrhea caused by Giardia in HIV-infected or other immunodeficient patients. CDC, NIH, and IDSA state that tinidazole and nitazoxanide are drugs of choice for treatment of giardiasis in HIV-infected infants and children† [off-label] and metronidazole is the preferred alternative in these patients.
Amebiasis
Has been used for treatment of amebiasis caused by Entamoeba † [off-label]. Designated an orphan drug by FDA for treatment of intestinal amebiasis.
Regimen of choice for symptomatic intestinal amebiasis or extraintestinal disease is treatment with a nitroimidazole derivative (tinidazole or metronidazole) followed by treatment with a luminal amebicide (iodoquinol or paromomycin).
Although nitazoxanide has been effective in some patients with mild to moderate intestinal amebiasis, data are limited and some clinicians state that additional study is needed.
Isosporiasis (Cystoisosporiasis)
Has been used in some patients for treatment of isosporiasis† [off-label] (also known as cystoisosporiasis) caused by Isospora belli (Cystoisospora belli).
Co-trimoxazole is drug of choice for treatment of infections caused by I. belli (C. belli); pyrimethamine and ciprofloxacin are recommended alternatives.
Although data are limited, some experts state that nitazoxanide is a potential alternative for treatment of isosporiasis (cystoisosporiasis) in HIV-infected infants and children† [off-label] who cannot tolerate co-trimoxazole.
Cestode (Tapeworm) Infections
Has been used for treatment of hymenolepiasis caused by Hymenolepis nana† (dwarf tapeworm).
Praziquantel is drug of choice for infections caused by H. nana; niclosamide (not commercially available in US) and nitazoxanide are recommended as alternatives.
Nematode (Roundworm) Infections
Has been used for treatment of ascariasis† caused by Ascaris lumbricoides. Albendazole, mebendazole, and ivermectin are the drugs of choice for ascariasis.
Has been used for treatment of trichuriasis† caused by Trichuris trichiura (whipworm). Albendazole is drug of choice for trichuriasis; recommended alternatives are mebendazole and ivermectin.
Trematode (Fluke) Infections
Has been used for treatment of fascioliasis caused by Fasciola hepatica† (sheep liver fluke).
Triclabendazole is considered drug of choice for fascioliasis and bithionol (not commercially available in US) and nitazoxanide are recommended as alternatives.
Nitazoxanide Dosage and Administration
Administration
Oral Administration
Administer orally twice daily with food.
Do not use nitazoxanide 500-mg tablets in pediatric patients ≤11 years of age; amount of drug contained in the tablets exceeds recommended dosage in this age group.
Reconstitution
Reconstitute powder for oral suspension at time of dispensing by adding 48 mL of water according to the manufacturer's directions. Tap the bottle to loosen the powder and add the water in 2 portions; shake vigorously after each addition.
Reconstituted suspension contains 100 mg/5 mL.
Shake suspension well prior to administration of each dose.
Dosage
Nitazoxanide tablets and oral suspension are not bioequivalent.
Pediatric Patients
Cryptosporidiosis
Oral
Children 1–3 years of age: 100 mg every 12 hours for 3 days.
Children 4–11 years of age: 200 mg every 12 hours for 3 days.
Children ≥12 years of age: 500 mg every 12 hours for 3 days.
HIV-infected pediatric patients† receiving optimized antiretroviral regimen: CDC, NIH, and IDSA recommend 100 mg twice daily in those 1–3 years of age, 200 mg twice daily in those 4–11 years of age, and 500 mg twice daily in those ≥12 years of age. Recommended duration is 3–14 days.
Giardiasis
Oral
Children 1–3 years of age: 100 mg every 12 hours for 3 days.
Children 4–11 years of age: 200 mg every 12 hours for 3 days.
Children ≥12 years of age: 500 mg every 12 hours for 3 days.
HIV-infected pediatric patients†: CDC, NIH, and IDSA recommend 100 mg every 12 hours in those 1–3 years of age, 200 mg every 12 hours in those 4–11 years of age, and 500 mg every 12 hours in those ≥12 years of age. Recommended duration is 3 days.
Isosporiasis (Cystoisosporiasis)†
Oral
HIV-infected pediatric patients†: CDC, NIH, and IDSA recommend 100 mg every 12 hours in those 1–3 years of age, 200 mg every 12 hours in those 4–11 years of age, and 500 mg every 12 hours in those ≥12 years of age. Recommended duration is 3 days.
Cestode (Tapeworm) Infections†
Hymenolepiasis†
OralChildren 1–3 years of age: 100 mg twice daily for 3 days.
Children 4–11 years of age: 200 mg twice daily for 3 days.
Children ≥12 years of age: 500 mg twice daily for 3 days.
Nematode (Roundworm) Infections†
Ascariasis†
OralChildren 1–3 years of age: 100 mg twice daily for 3 days.
Children 4–11 years of age: 200 mg twice daily for 3 days.
Children ≥12 years of age: 500 mg twice daily for 3 days.
Trichuriasis†
OralChildren 1–3 years of age: 100 mg twice daily for 3 days.
Children 4–11 years of age: 200 mg twice daily for 3 days.
Trematode (Fluke) Infections†
Fascioliasis†
OralChildren 1–3 years of age: 100 mg twice daily for 7 days.
Children 4–11 years of age: 200 mg twice daily for 7 days.
Children ≥12 years of age: 500 mg twice daily for 7 days.
Adults
Cryptosporidiosis
Oral
500 mg every 12 hours for 3 days.
HIV-infected adults† receiving optimized antiretroviral regimen: CDC, NIH, and IDSA recommend 0.5–1 g twice daily for 14 days.
Giardiasis
Oral
500 mg every 12 hours for 3 days.
Cestode (Tapeworm) Infections†
Hymenolepiasis†
Oral500 mg twice daily for 3 days.
Trematode (Fluke) Infections†
Fascioliasis†
Oral500 mg twice daily for 7 days.
Cautions for Nitazoxanide
Contraindications
-
Hypersensitivity to nitazoxanide or any ingredient in the formulation.
Warnings/Precautions
General Precautions
Immunodeficiency
Has not been more effective than placebo for treatment of diarrhea caused by C. parvum in HIV-infected or other immunodeficient individuals.
Not evaluated for treatment of diarrhea caused by Giardia in HIV-infected or other immunodeficient individuals.
Specific Populations
Pregnancy
Data not available on use of nitazoxanide in pregnant women to inform a drug-associated risk.
In animal reproduction studies, no evidence of teratogenicity or fetotoxicity when nitazoxanide was given to pregnant rats and rabbits during organogenesis at exposures 30 and 2 times, respectively, the human exposure at recommended human dosage of 500 mg twice daily based on body surface area.
Lactation
Not known whether distributed into human milk, affects milk production, or affects breast-fed child.
Consider developmental and health benefits of breast-feeding along with the mother's clinical need for nitazoxanide and potential adverse effects on the breast-fed infant from the drug or the underlying maternal condition.
Pediatric Use
Safety and efficacy not established in children <1 year of age.
Nitazoxanide oral suspension: Safety and efficacy for treatment of diarrhea caused by C. parvum or Giardia established in pediatric patients 1–17 years of age.
Nitazoxanide tablets: Safety and efficacy for treatment of diarrhea caused by C. parvum or Giardia established in pediatric patients 12–17 years of age. Do not use the 500-mg tablets in pediatric patients ≤11 years of age since the tablets contain a greater amount of the drug than is recommended in this age group.
Geriatric Use
Experience in those ≥65 years of age insufficient to determine whether they respond differently than younger individuals.
Consider the greater frequency of decreased hepatic, renal, and/or cardiac function and of concomitant disease or drug therapy in this age group.
Hepatic Impairment
Use with caution; pharmacokinetics not evaluated.
Renal Impairment
Use with caution; pharmacokinetics not evaluated.
Common Adverse Effects
Abdominal pain, headache, chromaturia, nausea.
Drug Interactions
Protein-bound Drugs
Possible pharmacokinetic interactions with other highly protein-bound drugs; monitor closely if used concomitantly with highly protein-bound drugs with a narrow therapeutic index. (See Specific Drugs under Interactions.)
Drugs Metabolized by Hepatic Microsomal Enzymes
Does not inhibit CYP isoenzymes.
Specific Drugs
|
Drug |
Interaction |
Comments |
|---|---|---|
|
Warfarin |
Possible competition for protein binding sites |
Avoid concomitant use |
Nitazoxanide Pharmacokinetics
Absorption
Bioavailability
Following oral administration, nitazoxanide is rapidly hydrolyzed to an active metabolite, tizoxanide, which is converted to tizoxanide glucuronide.
Peak plasma concentrations of tizoxanide and tizoxanide glucuronide usually attained within 1–5 and 2–8 hours, respectively; nitazoxanide undetectable in plasma.
The tablets and oral suspension are not bioequivalent. Bioavailability of the oral suspension is 70% relative to that of the tablet.
Food
Administration of nitazoxanide with food increases tizoxanide and tizoxanide glucuronide AUCs.
Distribution
Plasma Protein Binding
Tizoxanide: >99%.
Elimination
Metabolism
Rapidly hydrolyzed to tizoxanide; tizoxanide subsequently undergoes conjugation, primarily by glucuronidation.
Elimination Route
Tizoxanide eliminated in urine, bile, and feces; tizoxanide glucuronide eliminated in urine and bile.
Half-life
Nitazoxanide: 6 minutes.
Tizoxanide: 1.2–1.5 hours after single dose with food; 1.8–6.4 hours after repeated doses with food.
Tizoxanide glucuronide: 1.9–2.9 hours after single dose with food; 3.5–5.6 hours after repeated doses with food.
Special Populations
Pharmacokinetics not studied in patients with hepatic or renal impairment.
Stability
Storage
Oral
For Suspension
25°C (may be exposed to 15–30°C).
After reconstitution, store at room temperature; discard after 7 days.
Tablets
25°C (may be exposed to 15–30°C).
Actions and Spectrum
-
Nitazoxanide and its metabolite, tizoxanide, have antiprotozoal activity.
-
Antiprotozoal activity may be related principally to interference with the pyruvate:ferredoxin 2-oxidoreductase enzyme-dependent electron transfer reaction essential to anaerobic energy metabolism in susceptible organisms.
-
Protozoa: Active against sporozoites and oocysts of Cryptosporidium parvum and trophozoites of Giardia intestinalis (also known as G. lamblia or G. duodenalis). Also active against Entamoeba histolytica, Trichomonas vaginalis, Cyclospora cayetanensis, and Isospora belli (Cystoisospora belli).
-
Other organisms: Active against certain helminths, including some cestodes (tapeworms). Although clinical importance unclear, active in vitro against some anaerobic and microaerophilic gram-positive and gram-negative bacteria, including Clostridioides difficile (formerly known as Clostridium difficile) and Helicobacter pylori and also active against some viruses.
Advice to Patients
-
Advise patients to take nitazoxanide tablets or oral suspension with food.
-
Advise patients using the oral suspension to keep container tightly closed and shake the suspension well prior to each dose. Inform patients that the oral suspension may be stored at room temperature for up to 7 days and to discard any unused portion after that time.
-
Importance of informing clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs, and any concomitant illnesses. Importance of avoiding concomitant use of warfarin.
-
Importance of women informing clinicians if they are or plan to become pregnant or plan to breast-feed.
-
Importance of informing patients of other important precautionary information. (See Cautions.)
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
For suspension |
100 mg/5 mL |
Alinia |
Romark |
|
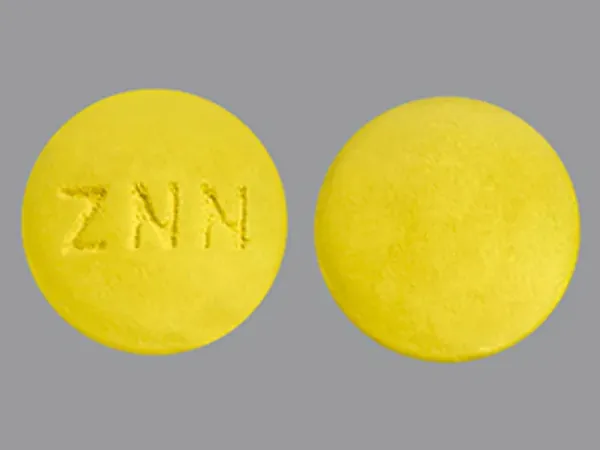
Tablets |
500 mg |
Alinia |
Romark |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions April 10, 2024. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
† Off-label: Use is not currently included in the labeling approved by the US Food and Drug Administration.
Reload page with references included
Related/similar drugs
More about nitazoxanide
- Check interactions
- Compare alternatives
- Reviews (2)
- Drug images
- Side effects
- Dosage information
- During pregnancy
- Drug class: amebicides
- Breastfeeding
- En español