Dutasteride (Monograph)
Brand name: Avodart
Drug class: 5-alpha-Reductase Inhibitors
Introduction
Selective inhibitor of steroid 5α-reductase isoenzymes, which are necessary for conversion of testosterone to 5α-dihydrotestosterone (DHT).
Uses for Dutasteride
Benign Prostatic Hyperplasia (BPH)
Used as monotherapy for treatment of symptomatic benign prostatic hyperplasia(BPH) in men with an enlarged prostate to improve symptoms, reduce the risk of acute urinary retention, and reduce the risk of the need for surgery. Used alone or in combination with tamsulosin.
A fixed-dose combination preparation containing dutasteride and tamsulosin hydrochloride is commercially available for the treatment of symptomatic BPH in men with an enlarged prostate.
The American Urological Association (AUA) guidelines consider 5α-reductase inhibitor monotherapy an appropriate option for symptomatic treatment of lower urinary tract symptoms in patients with BPH who have evidence of prostatic enlargement. A 5α-reductase inhibitor, alone or in combination with an α1-adrenergic blocker, is recommended as a treatment option to prevent progression of lower urinary tract symptoms/BPH and/or reduce risks of urinary retention and need for future prostate-related surgery in patients with demonstrable prostatic enlargement.
Not indicated for use in women and pediatric patients.
Not approved for prevention of prostate cancer.
Dutasteride Dosage and Administration
Administration
Oral Administration
Administer orally without regard to meals.
Swallow capsules whole; do not chew or open. Contact with the capsule contents may irritate oropharyngeal mucosa.
Dosage
Adults
Benign Prostatic Hyperplasia
Oral
0.5 mg once daily, alone or in combination with tamsulosin (0.4 mg once daily).
While early symptomatic improvement (e.g., within 3 months) may occur, ≥6 months of therapy may be necessary to determine clinical benefit. Generally, therapy is continued for life.
When the fixed-dose combination preparation of dutasteride and tamsulosin is used, the recommended dosage is 0.5 mg of dutasteride and 0.4 mg of tamsulosin hydrochloride taken once daily approximately 30 minutes after the same meal each day.
Special Populations
Hepatic Impairment
No specific dosage recommendations.
Renal Impairment
Dosage adjustment not required.
Geriatric Patients
Dosage adjustment not required.
Cautions for Dutasteride
Contraindications
-
Pregnancy.
-
Known hypersensitivity (e.g., serious skin reactions, angioedema) to dutasteride, other 5α-reductase inhibitors, or any ingredient in the formulation.
Warnings/Precautions
Effects on Prostate Specific Antigen (PSA)
Decreases PSA concentrations; may interfere with interpretation of serum PSA determinations. Concurrent use of tamsulosin does not substantially alter dutasteride’s effect on PSA concentrations.
May decrease serum PSA concentrations in men with prostate cancer; however, clinical benefit has not been demonstrated in patients with prostate cancer treated with dutasteride.
Carefully evaluate any confirmed increase in serum PSA concentration during therapy, even if PSA value is within normal range for men not receiving 5α-reductase inhibitor therapy.
Noncompliance may affect PSA concentrations; consider when evaluating test results.
High-grade Prostate Cancer
5α-Reductase inhibitors may increase risk of development of high-grade prostate cancer.
In 2 placebo-controlled trials evaluating dutasteride (0.5 mg daily for 4 years) or finasteride (5 mg daily for 7 years) for prevention of prostate cancer, overall occurrence of prostate cancer was reduced (due to reduction in lower-grade tumors) but incidence of high-grade tumors (Gleason score 8–10) was increased in men receiving dutasteride or finasteride. Not known whether detection bias (e.g., drug-induced reduction in prostate volume might have aided biopsy detection) or study-related factors influenced results.
Not FDA labeled for prevention of prostate cancer.
Consideration of Other Urological Conditions
Evaluate candidates for dutasteride therapy for other urologic conditions that might mimic BPH, such as infection, prostate or bladder cancer, stricture disease, uncontrolled diabetes mellitus, neurogenic bladder, or CHF.
BPH and prostate cancer may co-exist.
Risk to Male Fetus
May cause fetal harm; teratogenicity demonstrated in animals. Animal studies indicate adverse effects on embryofetal development of male fetuses exposed to the drug during pregnancy (e.g., abnormalities of the external genitalia, decreased prostatic and seminal vesicular weights, distended preputial glands, nipple development).
Because of the potential for absorption through the skin and the subsequent potential risk to a male fetus, pregnant women or women who may become pregnant should not handle the capsules. If contact is made with leaking capsules, wash the affected area immediately with soap and water.
If used during pregnancy or if pregnancy occurs, apprise the pregnant woman of potential fetal hazard to the male fetus.
Seminal drug concentrations not sufficient to warrant the use of condoms to prevent exposure to dutasteride.
Blood Donation
To prevent potential fetal exposure, men receiving the drug should not donate blood during dutasteride therapy and for at least 6 months following discontinuance of the drug.
Effects on Semen Characteristics
Reductions in sperm count, semen volume, and sperm motility reported; sperm concentration and morphology not altered. Clinical relevance not established.
Specific Populations
Pregnancy
Not indicated for use in women and contraindicated in women who are pregnant.
If used during pregnancy or if pregnancy occurs, apprise the pregnant woman of potential fetal hazard to a male fetus.
Because 5α-reductase inhibitors inhibit conversion of testosterone to DHT, dutasteride may cause abnormalities of the external genitalia of male fetuses exposed to the drug during pregnancy.
Because of the possibility of absorption through skin and subsequent risk to a male fetus, women who are pregnant or who potentially may be pregnant should not handle dutasteride capsules; if contact with a leaking dutasteride capsule occurs during pregnancy, wash affected area immediately with soap and water.
Lactation
Not known whether dutasteride is distributed into human milk or if drug has any effects on breastfed infant or on milk product; not indicated for use in women.
Females and Males of Reproductive Potential
Reductions in total sperm count, semen volume, and sperm motility observed; sperm concentration and morphology unaffected. Clinical significance of such effects on individual patient's fertility not known.
Pediatric Use
Safety and efficacy not established; not indicated for use in pediatric patients.
Geriatric Use
No substantial differences in safety and efficacy relative to younger men, but increased sensitivity cannot be ruled out.
Hepatic Impairment
Not studied in patients with hepatic impairment. Increased exposure to the drug is probable. Use with caution.
Renal Impairment
Dosage adjustment not necessary in renal impairment.
Common Adverse Effects
Impotence, decreased libido, ejaculation disorder, breast disorders (tenderness, enlargement). Ejaculation disorders reported more frequently with combined therapy (dutasteride plus tamsulosin) than either drug alone.
Drug Interactions
Metabolized by CYP isoenzymes 3A4 and 3A5 to active metabolites; not metabolized by CYP isoenzymes 1A2, 2A6, 2B6, 2C8, 2C9, 2C19, 2D6, or 2E1.
Drugs Affecting Hepatic Microsomal Enzymes
Potential pharmacokinetic interaction with inhibitors of CYP3A4 and CYP3A5 (decreased clearance and increased serum concentrations of dutasteride). Use with caution in patients receiving chronic therapy with potent CYP3A4 inhibitors.
Specific Drugs and Laboratory Tests
|
Drug or Test |
Interaction |
Comments |
|---|---|---|
|
Amlodipine |
Pharmacokinetic interaction unlikely |
|
|
Cholestyramine |
Pharmacokinetic or pharmacodynamic interaction unlikely |
|
|
Cimetidine |
Possible decreased clearance and increased serum concentrations of dutasteride |
Use concomitantly with care |
|
Ciprofloxacin |
Possible decreased clearance and increased serum concentrations of dutasteride |
Use concomitantly with care |
|
Digoxin |
Effect on digoxin pharmacokinetics unlikely |
|
|
Diltiazem |
Decreased clearance and increased serum concentrations of dutasteride |
Not considered clinically important |
|
Ketoconazole |
Possible decreased clearance and increased serum concentrations of dutasteride |
Use concomitantly with care |
|
Ritonavir |
Possible decreased clearance and increased serum concentrations of dutasteride |
Use concomitantly with care |
|
Tamsulosin |
Effect on tamsulosin pharmacokinetics unlikely |
|
|
Terazosin |
Effect on terazosin pharmacokinetics unlikely |
|
|
Test for PSA |
50% decrease in serum PSA concentration within 3–6 months of treatment No substantial change in ratio of free to total PSA (percentage of free PSA) |
Do not interpret decrease in PSA value as a therapeutic effect on prostate cancer Establish a new baseline PSA 3–6 months after initiation of treatment For clinical interpretation of isolated PSA values in men receiving dutasteride for ≥3 months, double the reported PSA value for comparison with normal values in men not receiving the drug No adjustment of reported value of ratio appears to be necessary |
|
Verapamil |
Decreased clearance and increased serum concentrations of dutasteride |
Not considered clinically important |
|
Warfarin |
Effect on warfarin pharmacokinetics or pharmacodynamics unlikely |
Dutasteride Pharmacokinetics
Absorption
Bioavailability
Absolute bioavailability is approximately 60%.
Onset
Reduces serum and prostatic 5α-dihydroxytestosterone (DHT) concentrations maximally within 1–2 weeks of initiation of therapy.
Duration
Serum drug concentrations are detectable for up to 4–6 months following discontinuance of therapy.
Food
Decreases peak serum concentrations. Not considered clinically important.
Distribution
Extent
Widely distributed; volume of distribution is 300–500 L.
Distributes into semen.
Plasma Protein Binding
Highly bound to albumin (99%) and α-1 acid glycoprotein (96.6%).
Elimination
Metabolism
Metabolized by CYP3A4 and CYP3A5 to active metabolites.
Elimination Route
Excreted in the feces (45%) and urine (<1%) mainly as metabolites; approximately 55% remained unaccounted.
Half-life
Terminal half-life is approximately 5 weeks at steady state.
Special Populations
In patients with hepatic impairment, pharmacokinetics not studied. Metabolized extensively in the liver, and increased exposure to the drug is probable in hepatic impairment.
In adolescents (<18 years of age), pharmacokinetics not studied.
In patients with renal impairment, pharmacokinetics not studied; however, <0.1% of a dose is excreted in urine in healthy individuals.
In women, pharmacokinetics not studied; use contraindicated.
Effects of race on pharmacokinetics not studied.
Stability
Storage
Oral
Capsules
25°C (may be exposed to 15–30°C).
Actions
-
Competitive inhibitor of both the type 1 and type 2 isoenzymes of steroid 5α-reductase. These enzymes convert testosterone to DHT.
-
Reduces serum and prostatic DHT concentrations substantially. DHT appears to be the principal androgen responsible for initial development and subsequent enlargement of the prostate gland.
-
Increases serum testosterone (generally remaining within the normal range) and prostatic testosterone concentrations.
Advice to Patients
-
Advise patients to read the patient information on dutasteride.
-
Inform patients that dutasteride decreases serum PSA concentrations. Advise patients of the importance of appropriate medical evaluation of any increase in PSA concentration. If a PSA test is performed, the patient should inform the clinician that he is taking a 5α-reductase inhibitor.
-
Inform patients that the incidence of high-grade prostate cancer was increased in men receiving 5α-reductase inhibitors (including dutasteride) in clinical trials evaluating efficacy of these drugs for prostate cancer prevention.
-
Risk to male fetuses. Advise patients that pregnant women or women who may become pregnant should not handle the drug; if contact with a leaking capsule occurs during pregnancy, wash affected area immediately with soap and water and inform clinician.
-
Avoid donation of blood during and for ≥6 months following discontinuance of dutasteride therapy.
-
Advise men that dutasteride may affect sperm characteristics but the effect on fertility is unknown.
-
Importance of informing clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs.
-
Inform patients of other important precautionary information.
Additional Information
The American Society of Health-System Pharmacists, Inc. represents that the information provided in the accompanying monograph was formulated with a reasonable standard of care, and in conformity with professional standards in the field. Readers are advised that decisions regarding use of drugs are complex medical decisions requiring the independent, informed decision of an appropriate health care professional, and that the information contained in the monograph is provided for informational purposes only. The manufacturer’s labeling should be consulted for more detailed information. The American Society of Health-System Pharmacists, Inc. does not endorse or recommend the use of any drug. The information contained in the monograph is not a substitute for medical care.
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
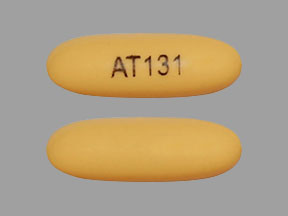
Oral |
Capsules, liquid-filled |
0.5 mg* |
Avodart |
Waylis Therapeutics |
|
Dutasteride Capsules |
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Capsules |
0.5 mg of dutasteride with 0.4 mg of tamsulosin hydrochloride |
Jalyn |
GlaxoSmithKline |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions June 10, 2024. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
Reload page with references included
Related/similar drugs
More about dutasteride
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (73)
- Drug images
- Side effects
- Dosage information
- During pregnancy
- Drug class: 5-alpha-reductase inhibitors
- En español