Neostigmine (Monograph)
Brand name: Bloxiverz
Drug class: Parasympathomimetic (Cholinergic) Agents
Introduction
Anticholinesterase agent.105 109 120 130
Uses for Neostigmine
Reversal of Neuromuscular Blockade
Reversal of the effects of nondepolarizing neuromuscular blocking agents (e.g., atracurium, cisatracurium, pancuronium, rocuronium, vecuronium).23 24 39 105 119 126 139
Use in conjunction with an anticholinergic agent (atropine sulfate or glycopyrrolate) to counteract adverse muscarinic effects (e.g., bradycardia, bradyarrhythmias, increased secretions, bronchoconstriction).105 120 121
Reduces time to recovery of neuromuscular function (defined as a return of train-of-four [TOF] twitch ratio to 0.9).105 119 123 126
Not effective in antagonizing deep levels of neuromuscular blockade; attempt reversal only after some degree of spontaneous recovery has occurred (e.g., when there is a detectable twitch response to the first TOF stimulus).105 119 121 122 129
Do not use in patients with complete neuromuscular recovery; paradoxical neuromuscular effects (e.g., weakness of upper airway muscles, increased airway collapsibility) may occur.122 125 127 128 129
Not effective and should not be used for reversal of depolarizing neuromuscular agents (e.g., succinylcholine).a
Appropriate reversal of neuromuscular blocking agents is critical for preventing postoperative residual neuromuscular blockade.120 121 122 123 150 151 Reversal of neuromuscular blockade should routinely be considered unless there is quantitative evidence indicating that no reversal is needed (TOF >0.9).122 139 154
Myasthenia Gravis
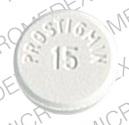
Has been used for symptomatic treatment of myasthenia gravis† [off-label] to improve muscle strength; however, oral preparation (e.g., Prostigmin) previously used for this indication no longer commercially available in the US.106 107 108 109 110 138
If an anticholinesterase agent is required for symptomatic treatment of myasthenia gravis, pyridostigmine is the preferred drug.107 109 132
GI Disorders
Has been used for treatment of acute colonic pseudo-obstruction or Ogilvie syndrome† [off-label].112 113 114 133 May be effective as second-line therapy in patients who fail conservative therapy.112 113 114 133
Has been used as a prokinetic agent in patients with postoperative ileus following surgery† [off-label]; however, clinical usefulness may be limited by adverse muscarinic effects (e.g., bradycardia, increased bronchial secretions).115 116 117
Has been used in the management of severe constipation in patients with thoracic spinal cord injury† [off-label].100 101 102
Neostigmine Dosage and Administration
General
Patient Monitoring
-
When used for reversal of neuromuscular blockade, patients must be well ventilated and have a patent airway prior to administration and until complete recovery of normal respiration.105 Continuous monitoring of neuromuscular function is recommended to ensure adequate reversal from the neuromuscular block.105 To exclude with certainty the possibility of residual paralysis, use an objective (quantitative) method of monitoring such as peripheral nerve stimulation in conjunction with other clinical assessments (e.g., observation of skeletal muscle tone, respiratory measurements).105 120 122 123 124 127 130 Adequate recovery of neuromuscular function generally is defined as a train-of-four (TOF) ratio of 0.9 in addition to the patient's ability to maintain satisfactory ventilation and a patent airway.105 120 Recovery times may vary based on the patient's medical condition and duration of action of the specific neuromuscular blocking agent used.105 119
Dispensing and Administration Precautions
-
Administer only by trained clinicians experienced in the use of neuromuscular blocking agents and their reversal agents.105
-
Always have atropine and medications to treat anaphylaxis (e.g., epinephrine) readily available in case of hypersensitivity reaction.103 105
Other General Considerations
-
Administer IV atropine sulfate or glycopyrrolate immediately prior to or concurrently (in separate syringes) with neostigmine to counteract adverse muscarinic effects.103 If patient is bradycardic, give IV antimuscarinic before neostigmine.105
Administration
Administer by slow IV injection over a period of at least 1 minute.105 Also has been administered by IM or sub-Q injection.103 109 131 † [off-label]
Dosage
Available as neostigmine methylsulfate; dosage expressed in terms of the salt.105
Pediatric Patients
Reversal of Neuromuscular Blockade
IV
Manufacturer states that pediatric patients may receive the same doses recommended for adults.105 (See Adults under Dosage and Administration.)
Other experts have recommended IV doses of 0.025 to 0.07 mg/kg in neonates, 0.025–0.1 mg/kg in infants, and 0.025–0.08 mg/kg in children.103
Adults
Reversal of Neuromuscular Blockade
IV
Manufacturer states that a dose of 0.03–0.07 mg/kg usually is sufficient to achieve adequate recovery of neuromuscular function (i.e., TOF ratio of 0.9) within 10–20 minutes.105 119
Individualize selection of dose based on half-life of neuromuscular blocking agent administered, degree of spontaneous recovery, and need for rapid reversal.105
To reverse neuromuscular blocking agents with shorter half-lives (e.g., rocuronium) or shallower blocks (i.e., first twitch response substantially >10% of baseline or when a second twitch is present): 0.03 mg/kg recommended.105
To reverse longer-acting neuromuscular blocking agents (e.g., pancuronium, vecuronium) or deeper blocks (i.e., first twitch response not substantially >10% of baseline), or when more rapid recovery is needed: 0.07 mg/kg recommended.105
Determine need for additional doses based on TOF monitoring and extent of recovery of neuromuscular function.105
Prescribing Limits
Pediatric Patients
Reversal of Neuromuscular Blockade
IV
Maximum total dose of 0.07 mg/kg or 5 mg, whichever is less.105 Higher doses unlikely to provide additional clinical benefit.125
Adults
Reversal of Neuromuscular Blockade
IV
Maximum total dose of 0.07 mg/kg or 5 mg, whichever is less.105 Higher doses unlikely to provide additional clinical benefit.125
Special Populations
Hepatic Impairment
Dosage adjustment not necessary.105
Renal Impairment
Dosage adjustment not necessary.105
Geriatric Patients
Dosage adjustment not required.105
Cautions for Neostigmine
Contraindications
-
Known hypersensitivity to neostigmine.105
-
Mechanical obstruction of the intestinal or urinary tract.105
-
Peritonitis.105
Warnings/Precautions
Warnings
Bradycardia
Bradycardia may occur.105 Administer atropine or glycopyrrolate prior to neostigmine to lessen risk.105
Serious Reactions with Coexisting Conditions
Risk of adverse cardiovascular effects such as bradycardia, hypotension, tachycardia, and cardiac arrhythmias.105 107 120 121 Use with caution in patients with coronary artery disease, cardiac arrhythmias, recent acute coronary syndrome, or myasthenia gravis; risk of cardiovascular complications may be increased in such patients.105
Administer an anticholinergic agent (e.g., atropine) prior to or concomitantly with neostigmine to minimize risk.105
Neuromuscular Dysfunction
Paradoxical neuromuscular effects (e.g., weakness of upper airway muscles and increased airway collapsibility) can occur if neostigmine is administered to patients with complete or near complete neuromuscular recovery.105 122 125 127 129 Reduce dose if neuromuscular recovery is almost complete.105
Cholinergic Crisis
Overdosage may result in cholinergic crisis (e.g., excessive salivation and sweating, miosis, nausea, vomiting, diarrhea, bradycardia or tachycardia, hypotension, confusion, seizures, coma, severe muscle weakness, paralysis); may result in death.105 a If overdosage occurs, withdraw all anticholinesterase drugs, maintain adequate respiration, and administer IV atropine.105
Myasthenic crisis, a complication of myasthenia gravis, can also cause extreme muscle weakness.105 141 It is extremely important to differentiate between the conditions since treatment methods differ considerably.105 Whereas more intensive anticholinesterase therapy is required in myasthenic crisis, higher doses of neostigmine can have serious consequences in cholinergic crisis.105
Sensitivity Reactions
Hypersensitivity
Hypersensitivity reactions, including urticaria, angioedema, erythema multiforme, generalized rash, facial swelling, peripheral edema, pyrexia, flushing, hypotension, bronchospasm, bradycardia, and anaphylaxis, reported.105
Atropine and other drugs for treatment of anaphylaxis should be readily available.105
Specific Populations
Pregnancy
Not known whether neostigmine can cause fetal harm when administered to pregnant women or can affect reproductive capacity; use during pregnancy only if clearly indicated.105
May induce premature labor if given IV to pregnant women near term.105
Lactation
Not known whether neostigmine is distributed into milk.105 Caution advised.105
Pediatric Use
May be used in pediatric patients of all ages to reverse the effects of nondepolarizing neuromuscular blocking agents.105 119 130
Although some pharmacokinetic parameters may differ in children compared with adults,130 manufacturer recommends same dosing guideline as in adults.105
Smaller doses usually required to reverse neuromuscular blockade in infants and children compared with adults;105 130 however, pediatric patients have a greater risk of incomplete reversal of neuromuscular blockade due to decreased respiratory reserve.105 Risk of administering higher doses of neostigmine (up to maximum recommended dosage) should not outweigh risk associated with incomplete reversal.105
Geriatric Use
Use with caution and increased monitoring.105 Duration of action of neostigmine is prolonged in geriatric patients; however, such patients also experience slower spontaneous recovery from neuromuscular blocking agents.105 Monitor for longer periods to ensure that additional doses of neostigmine are not necessary to adequately reverse neuromuscular blockade.105
Hepatic Impairment
Carefully monitor if neuromuscular blocking agents with hepatic elimination or active metabolites are administered to patients with hepatic impairment; duration of the neuromuscular blocking agent may be prolonged and persist beyond the effects of neostigmine.105
Renal Impairment
Closely monitor patients with renal impairment if a renally eliminated neuromuscular blocking agent is administered; effects of the neuromuscular blocking agent may persist beyond those of neostigmine.105
Common Adverse Effects
Bradycardia, nausea, vomiting.105
Drug Interactions
Drug interaction studies not conducted to date.105 Clinically important drug interactions not likely to occur if neuromuscular monitoring is employed and both relaxants and reversal agents are titrated to effect.120
Drugs Affecting Hepatic Microsomal Enzymes
Metabolized by hepatic microsomal enzymes; caution advised when used concomitantly with drugs that inhibit or induce these enzymes.105
Specific Drugs
|
Drug |
Interaction |
Comments |
|---|---|---|
|
Anticholinergic agents (atropine, glycopyrrolate) |
Antagonize muscarinic effects of neostigmine105 |
Interaction used to therapeutic advantage to counteract muscarinic symptoms of neostigmine toxicity; however, atropine also may mask manifestations of neostigmine overdose and prevent early detection of cholinergic crisis105 |
|
Neuromuscular blocking agents, depolarizing (e.g., succinylcholine) |
Possible enhanced and/or prolonged neuromuscular blockade140 |
Neostigmine is not indicated for reversal of depolarizing neuromuscular blocking agents140 |
|
Neuromuscular blocking agents, nondepolarizing (e.g., atracurium, cisatracurium, pancuronium, rocuronium, vecuronium) |
Antagonism of nondepolarizing muscle relaxant effects105 |
Interaction used to therapeutic advantage to reverse muscle relaxation induced by neuromuscular blocking agents after surgery105 |
Neostigmine Pharmacokinetics
Distribution
Extent
Not known whether distributed into human milk.105
Plasma Protein Binding
15–25% to serum albumin.105
Elimination
Metabolism
Metabolized by microsomal enzymes in the liver.105 121
Elimination Route
Excreted in urine as unchanged drug (50%).121
Half-life
IV: 24–113 minutes.105
Special Populations
Hepatic impairment: Pharmacokinetics not studied.105
Renal impairment reduces neostigmine clearance.119 Elimination half-life is prolonged in anephric individuals.105 119
Elimination half-life approximately 39, 48, or 67 minutes in infants 2–10 months of age, children 1–6 years of age, or adults 29–48 years of age, respectively.105
Stability
Storage
Parenteral
Injection
20–25°C (may be exposed to 15–30°C).105 Protect from light and store in original carton until use.105
Actions
-
Competitively inhibits acetylcholinesterase, reducing degradation of acetylcholine; as a result, acetylcholine accumulates at cholinergic synapses producing prolonged and exaggerated effects.105 109 120 130 Has direct cholinomimetic effect on skeletal muscle.a
-
Increased acetylcholine at neuromuscular junction competes with and reverses the effects of nondepolarizing neuromuscular blocking agents.105 121
-
In patients with myasthenia gravis, enhances neuromuscular transmission, providing symptomatic improvement.106 107 109
-
Produces generalized cholinergic effects including miosis, bradycardia, increased tonus of intestinal musculature, constriction of bronchi and ureters, and stimulation of secretion by salivary and sweat glands.a
-
Does not readily cross blood-brain barrier.105
Advice to Patients
-
Importance of informing clinician of existing or contemplated concomitant therapy, including prescription and OTC drugs and dietary or herbal supplements, as well as any concomitant illnesses.105
-
Importance of women informing clinicians if they are or plan to become pregnant or plan to breast-feed.105
-
Importance of informing patients of other important precautionary information.105
Additional Information
The American Society of Health-System Pharmacists, Inc. represents that the information provided in the accompanying monograph was formulated with a reasonable standard of care, and in conformity with professional standards in the field. Readers are advised that decisions regarding use of drugs are complex medical decisions requiring the independent, informed decision of an appropriate health care professional, and that the information contained in the monograph is provided for informational purposes only. The manufacturer’s labeling should be consulted for more detailed information. The American Society of Health-System Pharmacists, Inc. does not endorse or recommend the use of any drug. The information contained in the monograph is not a substitute for medical care.
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Parenteral |
Injection |
0.5 mg/mL* |
Bloxiverz |
Avadel Legacy |
|
Neostigmine Methylsulfate Injection |
||||
|
1 mg/mL* |
Bloxiverz |
Avadel Legacy |
||
|
Neostigmine Methylsulfate Injection |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions June 10, 2025. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
† Off-label: Use is not currently included in the labeling approved by the US Food and Drug Administration.
References
Only references cited for selected revisions after 1984 are available electronically.
23. De Angelis J. Clinical studies involving neostigmine reversal of d-tubocurarine, gallamine, and pancuronium in man. Anesth Analg. 1974 Mar-Apr; 53:268-70.
24. Miller RD, Larson CP, Way WL. Comparative antagonism of d-tubocurarine-, gallamine-, and pancuronium-induced neuromuscular blockades by neostigmine. Anesthesiology. 1972; 37:503-9. https://pubmed.ncbi.nlm.nih.gov/4263447
39. Bridenbaugh PO, Churchll-Davidson HC. Response to tubocurarine chloride and its reversal by neostigmine methylsulfate in man. JAMA. 1968; 203:541-4. https://pubmed.ncbi.nlm.nih.gov/5694188
100. Miller LS, Staas WE Jr, Herbison GJ. Abdominal problems in patients with spinal cord lesions. Arch Phys Med Rehabil. 1975; 56:405-8. https://pubmed.ncbi.nlm.nih.gov/1164181
101. Glick ME, Meshkinpour H, Haldeman S et al. Colonic dysfunction in patients with thoracic spinal cord injury. Gastroenterology. 1984; 86:287-94. https://pubmed.ncbi.nlm.nih.gov/6690355
102. Miller LS. Neostigmine for severe constipation with spinal cord lesions. Ann Intern Med. 1984; 101:279.
103. Kleinman K, McDaniel L, Molloy M, eds. The Harriet Lane handbook: a manual for pediatric house officers. 22nd ed. Philadelphia, PA: Elsevier, Inc; 2021.
105. Avadel Legacy. Bloxiverz (neostigmine methylsulfate injection) prescribing information. Chesterfield, MO; 2019 Sept.
106. Drachman DB. Myasthenia gravis. N Engl J Med. 1994; 330:1797-810. https://pubmed.ncbi.nlm.nih.gov/8190158
107. Nicolle MW. Myasthenia gravis. Neurologist. 2002; 8:2-21. https://pubmed.ncbi.nlm.nih.gov/12803656
108. Mehndiratta MM, Pandey S, Kuntzer T. Acetylcholinesterase inhibitor treatment for myasthenia gravis. Cochrane Database Syst Rev. 2014; 10:CD006986.
109. Myasthenia Gravis Foundation of America. Myasthenia Gravis: A manual for the healthcare provider (2008). From Myasthenia Gravis Foundation of American website. http://www.myasthenia.org/HealthProfessionals/EducationalMaterials.aspx
110. Richman DP, Agius MA. Treatment of autoimmune myasthenia gravis. Neurology. 2003; 61:1652-61. https://pubmed.ncbi.nlm.nih.gov/14694025
112. Elsner JL, Smith JM, Ensor CR. Intravenous neostigmine for postoperative acute colonic pseudo-obstruction. Ann Pharmacother. 2012; 46:430-5. https://pubmed.ncbi.nlm.nih.gov/22388328
113. Ponec RJ, Saunders MD, Kimmey MB. Neostigmine for the treatment of acute colonic pseudo-obstruction. N Engl J Med. 1999; 341:137-41. https://pubmed.ncbi.nlm.nih.gov/10403850
114. Valle RG, Godoy FL. Neostigmine for acute colonic pseudo-obstruction: A meta-analysis. Ann Med Surg (Lond). 2014; 3:60-4. https://pubmed.ncbi.nlm.nih.gov/25568788
115. Traut U, Brügger L, Kunz R et al. Systemic prokinetic pharmacologic treatment for postoperative adynamic ileus following abdominal surgery in adults. Cochrane Database Syst Rev. 2008; :CD004930. https://pubmed.ncbi.nlm.nih.gov/18254064
116. Gannon RH. Current strategies for preventing or ameliorating postoperative ileus: a multimodal approach. Am J Health Syst Pharm. 2007; 64(20 Suppl 13):S8-12. https://pubmed.ncbi.nlm.nih.gov/17909275
117. Zeinali F, Stulberg JJ, Delaney CP. Pharmacological management of postoperative ileus. Can J Surg. 2009; 52:153-7. https://pubmed.ncbi.nlm.nih.gov/19399212
119. Food and Drug Administration. Summary Review: NDA#204078/S-000. From FDA website. http://www.accessdata.fda.gov/drugsatfda_docs/nda/2013/204078Orig1s000SumR.pdf
120. Bevan DR, Donati F, Kopman AF. Reversal of neuromuscular blockade. Anesthesiology. 1992; 77:785-805. https://pubmed.ncbi.nlm.nih.gov/1416176
121. Srivastava A, Hunter JM. Reversal of neuromuscular block. Br J Anaesth. 2009; 103:115-29. https://pubmed.ncbi.nlm.nih.gov/19468024
122. Brull SJ, Murphy GS. Residual neuromuscular block: lessons unlearned. Part II: methods to reduce the risk of residual weakness. Anesth Analg. 2010; 111:129-40. https://pubmed.ncbi.nlm.nih.gov/20442261
123. Murphy GS, Brull SJ. Residual neuromuscular block: lessons unlearned. Part I: definitions, incidence, and adverse physiologic effects of residual neuromuscular block. Anesth Analg. 2010; 111:120-8. https://pubmed.ncbi.nlm.nih.gov/20442260
124. Murray MJ, DeBlock H, Erstad B et al. Clinical Practice Guidelines for Sustained Neuromuscular Blockade in the Adult Critically Ill Patient. Crit Care Med. 2016; 44:2079-2103. https://pubmed.ncbi.nlm.nih.gov/27755068
125. Kopman AF, Eikermann M. Antagonism of non-depolarising neuromuscular block: current practice. Anaesthesia. 2009; 64 Suppl 1:22-30. https://pubmed.ncbi.nlm.nih.gov/19222428
126. Lederer W, Reiner T, Khuenl-Brady KS. Neostigmine injected 5 minutes after low-dose rocuronium accelerates the recovery of neuromuscular function. J Clin Anesth. 2010; 22:420-4. https://pubmed.ncbi.nlm.nih.gov/20868962
127. Herbstreit F, Zigrahn D, Ochterbeck C et al. Neostigmine/glycopyrrolate administered after recovery from neuromuscular block increases upper airway collapsibility by decreasing genioglossus muscle activity in response to negative pharyngeal pressure. Anesthesiology. 2010; 113:1280-8. https://pubmed.ncbi.nlm.nih.gov/20980910
128. Caldwell JE. Reversal of residual neuromuscular block with neostigmine at one to four hours after a single intubating dose of vecuronium. Anesth Analg. 1995; 80:1168-74. https://pubmed.ncbi.nlm.nih.gov/7762847
129. Sasaki N, Meyer MJ, Malviya SA et al. Effects of neostigmine reversal of nondepolarizing neuromuscular blocking agents on postoperative respiratory outcomes: a prospective study. Anesthesiology. 2014; 121:959-68. https://pubmed.ncbi.nlm.nih.gov/25225821
130. Meretoja OA. Neuromuscular block and current treatment strategies for its reversal in children. Paediatr Anaesth. 2010; 20:591-604. https://pubmed.ncbi.nlm.nih.gov/20642658
131. Fresenius Kabi. Neostigmine methylsulfate injection prescribing information. Lake Zurich, IL; 2015 Sept.
132. Sanders DB, Wolfe GI, Benatar M et al. International consensus guidance for management of myasthenia gravis: Executive summary. Neurology. 2016; 87:419-25. https://pubmed.ncbi.nlm.nih.gov/27358333
133. Naveed M, Jamil LH, Fujii-Lau LL et al. American Society for Gastrointestinal Endoscopy guideline on the role of endoscopy in the management of acute colonic pseudo-obstruction and colonic volvulus. Gastrointest Endosc. 2020; 91:228-235. https://pubmed.ncbi.nlm.nih.gov/31791596
134. Blobner M, Eriksson LI, Scholz J et al. Reversal of rocuronium-induced neuromuscular blockade with sugammadex compared with neostigmine during sevoflurane anaesthesia: results of a randomised, controlled trial. Eur J Anaesthesiol. 2010; 27:874-81. https://pubmed.ncbi.nlm.nih.gov/20683334
135. Khuenl-Brady KS, Wattwil M, Vanacker BF et al. Sugammadex provides faster reversal of vecuronium-induced neuromuscular blockade compared with neostigmine: a multicenter, randomized, controlled trial. Anesth Analg. 2010; 110:64-73. https://pubmed.ncbi.nlm.nih.gov/19713265
136. Jones RK, Caldwell JE, Brull SJ et al. Reversal of profound rocuronium-induced blockade with sugammadex: a randomized comparison with neostigmine. Anesthesiology. 2008; 109:816-24. https://pubmed.ncbi.nlm.nih.gov/18946293
137. Lemmens HJ, El-Orbany MI, Berry J et al. Reversal of profound vecuronium-induced neuromuscular block under sevoflurane anesthesia: sugammadex versus neostigmine. BMC Anesthesiol. 2010; 10:15. https://pubmed.ncbi.nlm.nih.gov/20809967
138. APP. Neostigmine methylsulfate injection prescribing information.Schaumburg, IL; 2008 Apr.
139. Murphy GS, Szokol JW, Avram MJ et al. Neostigmine Administration after Spontaneous Recovery to a Train-of-Four Ratio of 0.9 to 1.0: A Randomized Controlled Trial of the Effect on Neuromuscular and Clinical Recovery. Anesthesiology. 2018; 128:27-37. https://pubmed.ncbi.nlm.nih.gov/28953501
140. Hospira. Quelicin (succinylcholine chloride injection) prescribing information. Lake Forest, IL; 2019 Feb.
141. Wijdicks EFM. Breaking Down Myasthenic Crisis. Neurocrit Care. 2020; 32:875-879. https://pubmed.ncbi.nlm.nih.gov/31981022
150. Miskovic A, Lumb AB. Postoperative pulmonary complications. Br J Anaesth. 2017; 118:317-334. https://pubmed.ncbi.nlm.nih.gov/28186222
151. Hristovska AM, Duch P, Allingstrup M et al. Efficacy and safety of sugammadex versus neostigmine in reversing neuromuscular blockade in adults. Cochrane Database Syst Rev. 2017; 8:CD012763. https://pubmed.ncbi.nlm.nih.gov/28806470
153. Murphy GS. Neuromuscular Monitoring in the Perioperative Period. Anesth Analg. 2018; 126:464-468. https://pubmed.ncbi.nlm.nih.gov/28795964
154. Bronsert MR, Henderson WG, Monk TG et al. Intermediate-Acting Nondepolarizing Neuromuscular Blocking Agents and Risk of Postoperative 30-Day Morbidity and Mortality, and Long-term Survival. Anesth Analg. 2017; 124:1476-1483. https://pubmed.ncbi.nlm.nih.gov/28244947
155. Kheterpal S, Vaughn MT, Dubovoy TZ et al. Sugammadex versus Neostigmine for Reversal of Neuromuscular Blockade and Postoperative Pulmonary Complications (STRONGER): A Multicenter Matched Cohort Analysis. Anesthesiology. 2020; 132:1371-1381. https://pubmed.ncbi.nlm.nih.gov/32282427
a. AHFS drug information 2022. Neostigmine methylsulfate. Bethesda, MD: American Society of Health-System Pharmacists.
Related/similar drugs
More about neostigmine
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (1)
- Latest FDA alerts (1)
- Side effects
- Dosage information
- During pregnancy
- Drug class: cholinergic muscle stimulants
- Breastfeeding
- En español