Gefitinib (Monograph)
Brand name: Iressa
Drug class: Antineoplastic Agents
- Epidermal Growth Factor Receptor Inhibitors
- EGFR Inhibitors
- EGF Receptor Inhibitors
- Kinase Inhibitors
- Receptor Tyrosine Kinase Inhibitors
- Tyrosine Kinase Inhibitors
VA class: AN900
Chemical name: N-(3-chloro-4-fluorophenyl)-7-methoxy-6-[3-(4-morpholin)propoxy]-4-quinazolamine
Molecular formula: C22H24ClFN4O3
CAS number: 184475-35-2
Introduction
Antineoplastic agent; epidermal growth factor receptor (EGFR) tyrosine kinase inhibitor.
Uses for Gefitinib
Non-small Cell Lung Cancer (NSCLC)
First-line treatment of metastatic NSCLC in patients with tumors positive for EGFR exon 19 deletions (del19) or exon 21 (L858R) substitution mutations as detected by an FDA-approved diagnostic test (e.g., therascreen EGFR RGQ PCR Kit). Information on FDA-approved companion diagnostic tests for the detection of EGFR mutations in NSCLC is available at [Web].
Designated an orphan drug by FDA for treatment of EGFR mutation-positive NSCLC.
Gefitinib originally received accelerated approval in 2003 for the treatment of locally advanced or metastatic NSCLC following failure of a platinum-based and docetaxel regimen, but was voluntarily withdrawn from the market when subsequent confirmatory clinical trials failed to verify clinical benefit. The current approval is for a different patient population (i.e., previously untreated, EGFR-mutation positive) than the 2003 approval.
Safety and efficacy not established in patients with metastatic NSCLC whose tumors harbor EGFR mutations other than exon 19 deletions or exon 21 substitution mutations. Guidelines such as the American Society of Clinical Oncology (ASCO)/Ontario Health (OH; formerly known as Cancer Care Ontario) generally support use of gefitinib among other first- and second-line treatment options for stage IV NSCLC with driver alterations in EGFR in certain circumstances.
Gefitinib Dosage and Administration
General
Pretreatment Screening
-
Confirm presence of epidermal growth factor receptor (EGFR) exon 19 deletions (del19) or exon 21 (L858R) substitution mutations in tumor or plasma specimens of patients with non-small cell lung cancer (NSCLC) by an FDA-approved diagnostic test prior to initiating first-line therapy with gefitinib. Re-evaluate patients with a negative plasma del19 or L858R mutation result for the feasibility of a tumor biopsy.
Patient Monitoring
-
Monitor liver function tests periodically during treatment.
-
Monitor for new or worsening pulmonary symptoms such as dyspnea, cough, and fever.
-
Monitor for severe or persistent diarrhea or symptoms of GI perforation.
-
Monitor for the development of bullous, blistering, or exfoliating skin conditions.
-
Monitor for acute or worsening ocular disorders.
-
Closely monitor patients with a known cytochrome P-450 (CYP) 2D6 poor metabolizer genotype for adverse effects.
.
Administration
Oral Administration
Administer orally once daily without regard to meals.
For patients with difficulty swallowing solids, may disperse tablet in a container with 120–240 mL (4–8 ounces) of water. Stir the tablet in water for approximately 15 minutes until it is dispersed. Immediately drink liquid (containing dispersed tablet) or administer through a nasogastric tube, then rinse container with 120–240 mL of water and immediately drink liquid or administer through a nasogastric tube.
If a dose of gefitinib is missed and cannot be taken within 12 hours, do not take the missed dose and take the next dose at the regularly scheduled time.
Dosage
Adults
NSCLC
Oral
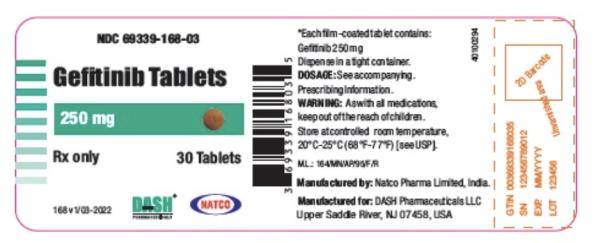
250 mg once daily. Continue therapy until disease progression or unacceptable toxicity occurs.
If used concomitantly with a potent CYP3A4 inducer, increase dosage to 500 mg once daily in the absence of severe adverse drug reactions. When the CYP3A4 inducer is discontinued, resume gefitinib at 250 mg once daily after 7 days.
Therapy Interruption for Toxicity
Temporarily interrupt (for up to 14 days) therapy in patients who develop new or worsening pulmonary symptoms (e.g., dyspnea, cough, fever), grade 2 or greater elevations in ALT and/or AST concentrations, grade 3 or greater diarrhea, severe or worsening ocular disorders (including keratitis), or grade 3 or greater dermatologic reactions. May resume gefitinib therapy when toxicity resolves completely or improves to grade 1.
Permanently discontinue therapy in patients who develop confirmed interstitial lung disease, severe hepatic impairment, GI perforation, or persistent ulcerative keratitis.
Special Populations
Hepatic Impairment
No specific dosage recommendations. Monitor patients with hepatic impairment for adverse effects. Discontinue in patients with severe hepatic impairment.
Renal Impairment
No specific dosage recommendations.
Geriatric Patients
No specific dosage recommendations.
Poor CYP2D6 Metabolizers
Because of possible increased systemic exposure, monitor patients with known CYP2D6 metabolizer genotype closely for adverse effects. Routine dosage adjustment not necessary.
Gender
No dosage adjustment required.
Cautions for Gefitinib
Contraindications
-
Manufacturer states none known.
Warnings/Precautions
Interstitial Lung Disease
Interstitial lung disease or interstitial lung disease-like events (e.g., lung infiltration, pneumonitis, ARDS, pulmonary fibrosis), sometimes fatal, reported. Patients with CYP2D6 poor metabolizer genotype may be at increased risk for ILD.
In patients who develop worsening pulmonary symptoms (e.g., dyspnea, cough, fever), temporarily interrupt therapy for up to 14 days and promptly evaluate patient for interstitial lung disease. If diagnosis of interstitial lung disease is confirmed, permanently discontinue gefitinib.
Hepatic Toxicity
Abnormal liver function tests (e.g., elevations in ALT, AST, and bilirubin concentrations), sometimes fatal, reported.
Perform liver function tests periodically during therapy. Temporarily interrupt therapy for up to 14 days in patients who develop grade 2 or greater elevations in ALT and/or AST concentrations. Permanently discontinue gefitinib in patients who develop severe hepatic impairment.
GI Perforation
GI perforation reported.
Permanently discontinue gefitinib in patients who develop GI perforation.
Diarrhea
Severe diarrhea reported.
If severe (grade 3 or greater) or persistent (lasting up to 14 days) diarrhea occurs, temporarily interrupt therapy for up to 14 days.
Ocular Disorders including Keratitis
Ocular disorders (e.g., keratitis, corneal erosion, abnormal eyelash growth, conjunctivitis, blepharitis, dry eye) reported.
Temporarily interrupt therapy for up to 14 days in patients who develop severe or worsening ocular disorders, including keratitis. Permanently discontinue gefitinib in patients who develop persistent ulcerative keratitis.
Dermatologic Effects
Bullous conditions, including toxic epidermal necrolysis, Stevens-Johnson syndrome, and erythema multiforme, reported rarely.
Temporarily interrupt therapy for up to 14 days or discontinue therapy in patients who develop severe bullous, blistering, or exfoliating conditions.
Fetal/Neonatal Morbidity and Mortality
May cause fetal harm. Fetal toxicity (e.g., decreased fetal weight, abortion) and neonatal mortality shortly after parturition observed in animals. Crosses the placenta.
Avoid pregnancy during therapy. Women of childbearing potential should use effective contraception while receiving the drug and for ≥2 weeks after the drug is discontinued. If used during pregnancy or patient becomes pregnant, apprise of potential fetal hazard.
Specific Populations
Pregnancy
May cause fetal harm.
Lactation
Gefitinib and its metabolites are distributed into milk in rats; not known whether distributed into human milk. Women receiving gefitinib should not breast-feed.
Females and Males of Reproductive Potential
Women of childbearing potential should use effective contraception while receiving the drug and for ≥2 weeks after the drug is discontinued.
Results of animal studies suggest that gefitinib may decrease female fertility.
Pediatric Use
Safety and efficacy not established.
Geriatric Use
No overall differences in safety relative to younger adults in 2 controlled studies. Insufficient experience in patients ≥65 years of age to determine differences in efficacy between geriatric patients and younger adults.
Hepatic Impairment
Increased systemic exposure has been reported in patients with mild (Child-Pugh class A), moderate (Child-Pugh class B), or severe (Child-Pugh class C) hepatic impairment due to cirrhosis.
Monitor patients with hepatic impairment for adverse effects.
Renal Impairment
Not studied in patients with severe renal impairment; however, <4% of the drug and its metabolites are excreted by the kidneys.
Pharmacogenomic Considerations
Because a clinically important increase in systemic exposure of gefitinib may occur in poor metabolizers of the cytochrome P-450 (CYP) isoenzyme 2D6, closely monitor patients with a known CYP2D6 poor metabolizer genotype for adverse effects.
Common Adverse Effects
Adverse effects reported in ≥20% of patients: Skin reactions/rash (e.g., acne, maculopapular rash, erythema, generalized rash, papular rash, pruritic rash, macular rash, dry skin), diarrhea.
Drug Interactions
Metabolized principally by CYP3A4 and, to a lesser extent, by CYP2D6. Does not inhibit CYP isoenzymes 1A2, 2C9, or 3A4 in vitro, but may inhibit 2C19 and 2D6 at high drug concentrations.
Drugs Affecting Hepatic Microsomal Enzymes
CYP3A4 and CYP2D6 inhibitors: Potential pharmacokinetic interaction (decreased metabolism and increased systemic exposure of gefitinib). If used concomitantly with a potent CYP3A4 or CYP2D6 inhibitor, monitor for signs of toxicity.
CYP3A4 inducers: Potential pharmacokinetic interaction (increased metabolism and decreased plasma concentrations of gefitinib). If used concomitantly with a potent CYP3A4 inducer, increase gefitinib dosage to 500 mg daily in the absence of severe adverse effects. When the CYP3A4 inducer is discontinued, resume gefitinib at 250 mg once daily after 7 days.
Drugs Affecting Gastric Acidity
Possible pharmacokinetic interaction (decreased plasma gefitinib concentrations and possible reduction in efficacy) with drugs that cause gastric pH elevation.
Specific Drugs
|
Drug |
Interaction |
Comments |
|---|---|---|
|
Antacids |
Possible decreased gefitinib concentrations Sodium bicarbonate and ranitidine (to achieve gastric pH ≥5) decreased gefitinib AUC by 47% |
Administer antacid 6 hours before or after gefitinib |
|
Antidepressants, tricyclics (TCAs) |
Increased metabolism and decreased plasma concentrations of gefitinib |
Increase gefitinib dosage to 500 mg daily in the absence of severe adverse effects When the TCA is discontinued, resume gefitinib at 250 mg once daily after 7 days |
|
Antifungals, azoles (e.g., itraconazole, ketoconazole) |
Itraconazole (CYP3A4 inhibitor) increased gefitinib AUC and peak concentrations by approximately 80 and 51%, respectively |
Monitor for adverse effects |
|
Histamine H2-receptor antagonists (e.g., cimetidine, famotidine, ranitidine) |
Possible decreased gefitinib concentrations Ranitidine and sodium bicarbonate (to achieve gastric pH ≥5) decreased gefitinib AUC by 47% |
Administer H2-receptor antagonist 6 hours before or after gefitinib |
|
Metoprolol |
Increased systemic exposure of metoprolol by 30% |
|
|
Phenytoin |
Increased metabolism and decreased plasma concentrations of gefitinib |
Increase gefitinib dosage to 500 mg daily in the absence of severe adverse effects When phenytoin is discontinued, resume gefitinib at 250 mg once daily after 7 days |
|
Proton-pump inhibitors |
Possible decreased gefitinib concentrations |
Avoid concomitant use, if possible; if concomitant use cannot be avoided, administer proton-pump inhibitor 12 hours before or after gefitinib Consider substituting H2-receptor antagonist or antacid (administered 6 hours before or after gefitinib) for proton-pump inhibitor |
|
Rifampin |
Rifampin (potent CYP3A4 inducer) decreased AUC and peak concentrations of gefitinib by 83 and 65%, respectively |
Increase gefitinib dosage to 500 mg daily in the absence of severe adverse effects When rifampin is discontinued, resume gefitinib at 250 mg once daily after 7 days |
|
Warfarin |
INR elevations and/or bleeding reported |
Monitor regularly for changes in PT or INR |
Gefitinib Pharmacokinetics
Absorption
Bioavailability
Slowly absorbed following oral administration, with peak plasma concentrations attained within 3–7 hours. Mean bioavailability is 60%.
Food
Food does not substantially affect bioavailability.
Special Populations
In healthy poor metabolizers of CYP2D6, mean exposure is twofold higher compared with extensive metabolizers of CYP2D6; however, plasma concentrations of O-desmethyl gefitinib are undetectable.
In patients with mild (Child-Pugh class A), moderate (Child-Pugh class B), or severe (Child-Pugh class C) hepatic impairment due to cirrhosis, mean systemic exposure is increased by 40, 263, or 166%, respectively, compared with healthy individuals with normal hepatic function. In patients with liver metastases and moderate hepatic impairment, systemic exposure was similar to that in patients with liver metastases and normal hepatic function.
Population pharmacokinetic analyses suggest that Clcr (>20 mL/minute) does not have a clinically important effect on steady-state trough concentrations. Not studied in patients with severe renal impairment.
Age, body weight, and ethnicity do not substantially affect pharmacokinetics.
In population pharmacokinetic analyses of one clinical study, women had 27% higher exposure than men; gender-related differences in exposure not identified in such analyses from other clinical studies.
Distribution
Extent
Extensively distributed throughout the body.
Crosses the placenta. Gefitinib and its metabolites distribute into milk in rats; not known whether distributed into human milk.
Plasma Protein Binding
90% in vitro (to albumin and α1-acid glycoprotein).
Elimination
Metabolism
Extensively metabolized in liver, principally by CYP3A4 and, to a lesser extent, by CYP2D6. Eight metabolites identified; only O-desmethyl gefitinib has exposure comparable to that of gefitinib, but potency is only 1/14 that of gefitinib.
Elimination Route
Excreted in feces (86%) and urine (<4%).
Half-life
48 hours.
Stability
Storage
Oral
Tablets
20–25°C.
Actions
-
Antineoplastic agent; EGFR tyrosine kinase inhibitor.
-
EGFR (HER1, c-ERbB-1) is expressed on the cell surface of both normal and cancer cells and plays a role in cell growth and proliferation. Some EGFR-activating mutations (del19 or L858R substitution mutations) within NSCLC cells can promote tumor cell growth, block apoptosis, increase production of angiogenic factors, and facilitate metastasis.
-
Reversibly inhibits phosphorylation and proliferation of cell lines expressing wild-type EGFR and cell lines expressing del19 or L858R mutations.
-
Exhibits greater binding affinity for EGFR del19 or L858R substitution mutations than for wild-type EGFR.
-
Inhibits insulin-like growth factor (IGF) and platelet-derived growth factor (PDGF) at clinically relevant concentrations.
Advice to Patients
-
Importance of reading the manufacturer's patient information.
-
If a dose of gefitinib is missed, instruct patients to take the missed dose as soon as it is remembered unless it is within 12 hours of the next scheduled dose, in which case they should not take the missed dose.
-
Risk of interstitial lung disease. Importance of immediately informing clinician if new or worsening respiratory symptoms occur (e.g., dyspnea, cough, fever).
-
Risk of hepatotoxicity and importance of periodic liver function test monitoring. Importance of reporting any manifestations of hepatotoxicity (e.g., jaundice, dark or “tea-colored” urine, right upper quadrant pain, light-colored stool, decreased appetite).
-
Risk of GI perforation. Importance of advising patients to seek immediate medical attention if they experience symptoms of GI perforation (e.g., severe abdominal pain).
-
Risk of severe or persistent diarrhea. Importance of informing clinician if severe or persistent diarrhea occurs.
-
Risk of ocular disorders, including keratitis. Importance of promptly informing clinician if ocular problems (e.g., lacrimation, sensitivity to light, eye pain, redness, blurred vision, other vision changes) occur.
-
Risk of bullous and exfoliative skin disorders. Importance of advising patients to seek immediate medical attention if they develop severe dermatologic reactions (e.g., peeling, blistering).
-
Risk of fetal harm and loss of pregnancy. Necessity of advising women of childbearing potential that they should use an effective method of contraception while receiving gefitinib and for ≥2 weeks after discontinuance of therapy. Importance of women informing clinicians if they are or plan to become pregnant. If pregnancy occurs, advise pregnant women of potential risk to the fetus.
-
Importance of women informing clinicians if they plan to breast-feed. Importance of advising women to avoid breast-feeding while receiving gefitinib.
-
Importance of informing clinician of existing or contemplated concomitant therapy, including prescription and OTC drugs (e.g., antacids, histamine H2-receptor antagonists, proton-pump inhibitors, warfarin) and herbal supplements, as well as any concomitant illnesses.
-
Importance of informing patients of other important precautionary information. (See Cautions.)
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
Gefitinib can only be obtained through select specialty pharmacies and distributors. Consult the manufacturer's website for specific ordering and availability information.
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Tablets, film-coated |
250 mg |
Iressa |
AstraZeneca |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions August 12, 2022. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
Reload page with references included
Related/similar drugs
More about gefitinib
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (8)
- Drug images
- Side effects
- Dosage information
- During pregnancy
- Drug class: EGFR inhibitors
- Breastfeeding
- En español