Brexucabtagene Autoleucel (Monograph)
Brand name: Tecartus
Drug class: Gene Therapy
Warning
WARNING: CYTOKINE RELEASE SYNDROME AND NEUROLOGIC TOXICITIES, and SECONDARY HEMATOLOGICAL MALIGNANCIES
See full prescribing information for complete boxed warning
-
Cytokine Release Syndrome (CRS), including life-threatening reactions, occurred in patients receiving brexucabtagene autoleucel. Do not administer brexucabtagene autoleucel to patients with active infection or inflammatory disorders. Treat severe or life-threatening CRS with tocilizumab or tocilizumab and corticosteroids.
-
Neurologic toxicities, including life-threatening reactions, occurred in patients receiving brexucabtagene autoleucel, including concurrently with CRS or after CRS resolution. Monitor for neurologic toxicities after treatment with brexucabtagene autoleucel. Provide supportive care and/or corticosteroids, as needed.
-
T cell malignancies have occurred following treatment of hematologic malignancies with BCMA- and CD19- directed genetically modified autologous T cell immunotherapies.
Introduction
Brexucabtagene autoleucel is a CD19-directed genetically modified autologous T cell immunotherapy.
Uses for Brexucabtagene Autoleucel
Brexucabtagene autoleucel has the following uses:
Brexucabtagene autoleucel is a chimeric antigen receptor (CAR) T-cell therapy with the following indications:
Treatment of adult patients with relapsed or refractory mantle cell lymphoma (MCL). This indication is approved under accelerated approval based on overall response rate and durability of response. Continued approval for this indication may be contingent upon verification and description of clinical benefit in a confirmatory trial. Brexucabtagene autoleucel has been designated an orphan drug by FDA for the treatment of MCL. Efficacy and safety of brexucabtagene autoleucel for this use were evaluated in a single-arm, open-label multicenter trial (ZUMA-2) in adults with relapsed or refractory MCL who had previously received anthracycline- or bendamustine-containing chemotherapy, an anti-CD20 antibody, and a Bruton tyrosine kinase inhibitor. A total of 60 patients underwent leukapheresis and received a single infusion of brexucabtagene autoleucel; these patients were followed for at least 6 months after their first objective disease response and comprised the efficacy population. The objective response rate per the Lugano Classification (2014) was 87% in the efficacy population; complete remission rate was 62% and partial remission rate was 25%. The median duration of response was not reached at a median follow-up of 8.6 months.
Treatment of adult patients with relapsed or refractory B-cell precursor acute lymphoblastic leukemia (ALL). Brexucabtagene autoleucel has been designated an orphan drug by FDA for the treatment of ALL. Efficacy of brexucabtagene autoleucel for this use was evaluated in an open-label, single-arm multicenter trial (ZUMA-3) in adults with relapsed or refractory B-cell precursor ALL. Treatment consisted of lymphodepleting chemotherapy (fludarabine and cyclophosphamide) followed by a single IV infusion of brexucabtagene autoleucel. Among 54 patients in the efficacy population, the overall complete remission rate was 64.8%; 51.9% of patients achieved complete remission at a median follow-up of 7.1 months. The median duration of remission was 13.6 months.
Brexucabtagene autoleucel is an individualized cellular product prepared from autologous T cells obtained by leukapheresis. The patient's T-cells are sent to a laboratory where they are genetically modified to express chimeric antigen receptors (CAR), and then infused back into the patient.
CAR T-cell therapies can be associated with severe toxicities; the American Society of Clinical Oncology (ASCO) has published a guideline to provide guidance on the diagnosis, evaluation and management of such toxicities.
Brexucabtagene Autoleucel Dosage and Administration
General
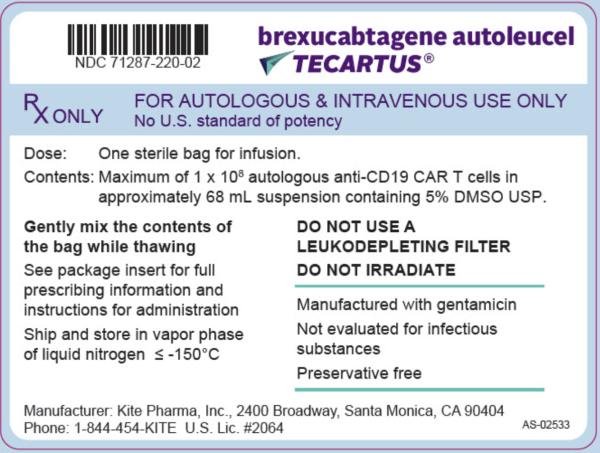
Brexucabtagene autoleucel is available in the following dosage form(s) and strength(s):
-
Cell suspension for IV infusion.
-
Mantle cell lymphoma (MCL): Each infusion bag contains a suspension of 2 × 106 CAR-positive viable T cells per kg of body weight, with a maximum of 2 × 108 CAR-positive viable T cells in approximately 68 mL.
-
Acute lymphoblastic leukemia (ALL): Each infusion bag contains a suspension of 1 × 106 CAR-positive viable T cells per kg of body weight, with a maximum of 1 × 108 CAR-positive viable T cells in approximately 68 mL.
Dosage
It is essential that the manufacturer's labeling be consulted for more detailed information on dosage and administration of this drug. Dosage summary:
Adults
Dosage and Administration
For autologous use only. For IV use only.
-
Administer brexucabtagene autoleucel in a certified healthcare facility.
-
Do NOT use a leukodepleting filter.
-
Administer a lymphodepleting regimen of cyclophosphamide and fludarabine before infusion of brexucabtagene autoleucel.
-
Verify the patient's identity prior to infusion. Check that the patient’s identity matches the patient identifiers on the infusion bag.
-
Premedicate with acetaminophen and diphenhydramine. Avoid prophylactic use of systemic corticosteroids as it may interfere with the activity of brexucabtagene autoleucel.
-
Confirm availability of tocilizumab prior to infusion.
-
Dosing of brexucabtagene autoleucel is based on the number of chimeric antigen receptor (CAR)-positive viable T cells.
-
Recommended dose for patients with MCL: target dose of 2 × 106 CAR-positive viable T cells per kg body weight, with a maximum of 2 × 108 CAR-positive viable T cells.
-
Recommended dose for patients with ALL: target dose of 1 × 106 CAR-positive viable T cells per kg body weight, with a maximum of 1 × 108 CAR-positive viable T cells.
-
See Full Prescribing Information for additional details on preparation and administration.
Cautions for Brexucabtagene Autoleucel
Contraindications
-
None.
Warnings/Precautions
Cytokine Release Syndrome
Cytokine release syndrome (CRS), including fatal or life-threatening reactions, occurred following treatment with brexucabtagene autoleucel. CRS occurred in 91% (75/82) of patients with mantle cell lymphoma (MCL), including ≥ Grade 3 (Lee grading system) CRS in 18% of patients. Among the patients with MCL who died after receiving brexucabtagene autoleucel, one patient had a fatal CRS event. The median time to onset of CRS was three days (range: 1 to 13 days) and the median duration of CRS was ten days (range: 1 to 50 days) for patients with MCL. CRS occurred in 92% (72/78) of patients with acute lymphoblastic leukemia (ALL), including ≥ Grade 3 (Lee grading system) CRS in 26% of patients. Three patients with ALL had ongoing CRS events at the time of death. The median time to onset of CRS was five days (range: 1 to 12 days) and the median duration of CRS was eight days (range: 2 to 63 days) for patients with ALL.
The incidence of CRS (first occurrence) within the first seven days after brexucabtagene autoleucel infusion was 83% (68/82) in patients with MCL and 90% (70/78) in patients with ALL. In all patients combined (MCL/ALL), the incidence of first CRS (first occurrence) within the first seven days after brexucabtagene autoleucel infusion was 86% (138/160).
Among patients with CRS, the key manifestations (>10%) were similar in MCL and ALL and included fever (93%), hypotension (62%), tachycardia (59%), chills (32%), hypoxia (31%), headache (21%), fatigue (20%), and nausea (13%). Serious events associated with CRS in MCL and ALL combined (≥ 2%) included hypotension, fever, hypoxia, tachycardia, and dyspnea.
Ensure that a minimum of two doses of tocilizumab are available for each patient prior to infusion of brexucabtagene autoleucel. Monitor patients daily for at least seven days for patients with MCL and at least 14 days for patients with ALL at the certified healthcare facility following infusion for signs and symptoms of CRS. Monitor patients for signs or symptoms of CRS for four weeks after infusion. Counsel patients to seek immediate medical attention should signs or symptoms of CRS occur at any time. At the first sign of CRS, institute treatment with supportive care, tocilizumab, or tocilizumab and corticosteroids as indicated.
Neurologic Toxicities
Neurologic toxicities (including ICANS) that were fatal or life-threatening, occurred following treatment with brexucabtagene autoleucel. Neurologic events occurred in 81% (66/82) of patients with MCL, including ≥ Grade 3 in 37% of patients. The median time to onset for neurologic events was six days (range: 1 to 32 days) with a median duration of 21 days (range: 2 to 454 days) in patients with MCL. Neurologic events occurred in 87% (68/78) of patients with ALL, including ≥ Grade 3 in 35% of patients. The median time to onset for neurologic events was seven days (range: 1 to 51 days) with a median duration of 15 days (range: 1 to 397 days) in patients with ALL. For patients with MCL, 54 (66%) patients experienced CRS before the onset of neurological events. Five (6%) patients did not experience CRS with neurologic events and eight patients (10%) developed neurological events after the resolution of CRS. Neurologic events resolved for 119 out of 134 (89%) patients treated with brexucabtagene autoleucel. Nine patients (three patients with MCL and six patients with ALL) had ongoing neurologic events at the time of death. For patients with ALL, neurologic events occurred before, during, and after CRS in 4 (5%), 57 (73%), and 8 (10%) of patients, respectively. Three patients (4%) had neurologic events without CRS. The onset of neurologic events can be concurrent with CRS, following resolution of CRS, or in the absence of CRS.
The incidence of neurologic events (first occurrence) within the first seven days after brexucabtagene autoleucel infusion was 56% (46/82) in patients with MCL and 55% (43/78) in patients with ALL. In all patients combined (MCL/ALL), the incidence of neurologic events (first occurrence) within the first seven days after brexucabtagene autoleucel infusion was 56% (89/160). Ninety-one percent of all treated patients experienced the first CRS or neurological event within the first seven days after brexucabtagene autoleucel infusion.
The most common neurologic events (>10%) were similar in MCL and ALL patients and included encephalopathy (57%), headache (37%), tremor (34%), confusional state (26%), aphasia (23%), delirium (17%), dizziness (15%), anxiety (14%), and agitation (12%). Serious events (≥ 2%) including encephalopathy, aphasia, confusional state, and seizures occurred after treatment with brexucabtagene autoleucel.
Monitor patients daily for at least seven days for patients with MCL and at least 14 days for patients with ALL at the certified healthcare facility following infusion for signs and symptoms of neurologic toxicities. Monitor patients for signs or symptoms of neurologic toxicities for four weeks after infusion and treat promptly.
Hemophagocytic Lymphohistiocytosis/Macrophage Activation Syndrome
Hemophagocytic lymphohistiocytosis/macrophage activation syndrome (HLH/MAS), including life-threatening reactions, occurred following treatment with brexucabtagene autoleucel. HLH/MAS occurred in 4% (3/78) of patients with ALL. Two patients experienced Grade 3 events and 1 patient experienced a Grade 4 event. The median time to onset for HLH/MAS was 8 days (range: 6 to 9 days) with a median duration of 5 days (range: 2 to 8 days).
All three patients with HLH/MAS had concurrent CRS symptoms and neurologic events after brexucabtagene autoleucel infusion. Treatment of HLH/MAS should be administered per institutional standards.
Hypersensitivity Reactions
Serious hypersensitivity reactions, including anaphylaxis, may occur due to dimethyl sulfoxide (DMSO) or residual gentamicin in brexucabtagene autoleucel.
Severe Infections
Severe or life-threatening infections occurred in patients after brexucabtagene autoleucel infusion. Infections (all grades) occurred in 56% (46/82) of patients with MCL and 44% (34/78) of patients with ALL. Grade 3 or higher infections, including bacterial, viral, and fungal infections, occurred in 30% of patients with ALL and MCL. Brexucabtagene autoleucel should not be administered to patients with clinically significant active systemic infections. Monitor patients for signs and symptoms of infection before and after brexucabtagene autoleucel infusion and treat appropriately. Administer prophylactic antimicrobials according to local guidelines.
Febrile neutropenia was observed in 6% of patients with MCL and 35% of patients with ALL after brexucabtagene autoleucel infusion and may be concurrent with CRS. The febrile neutropenia in 27 (35%) of patients with ALL includes events of "febrile neutropenia" (11 [14%]) plus the concurrent events of "fever" and "neutropenia" (16 [21%]). In the event of febrile neutropenia, evaluate for infection and manage with broad spectrum antibiotics, fluids, and other supportive care as medically indicated.
In immunosuppressed patients, life-threatening and fatal opportunistic infections have been reported. The possibility of rare infectious etiologies (e.g., fungal and viral infections such as HHV-6 and progressive multifocal leukoencephalopathy) should be considered in patients with neurologic events and appropriate diagnostic evaluations should be performed.
Hepatitis B Reactivation
Hepatitis B virus (HBV) reactivation, in some cases resulting in fulminant hepatitis, hepatic failure, and death, can occur in patients treated with drugs directed against B cells. Perform screening for HBV, hepatitis C virus (HCV), and human immunodeficiency virus (HIV) in accordance with clinical guidelines before collection of cells for manufacturing.
Prolonged Cytopenias
Patients may exhibit cytopenias for several weeks following lymphodepleting chemotherapy and brexucabtagene autoleucel infusion. In patients with MCL, Grade 3 or higher cytopenias not resolved by Day 30 following brexucabtagene autoleucel infusion occurred in 55% (45/82) of patients and included thrombocytopenia (38%), neutropenia (37%), and anemia (17%). In patients with ALL who were responders to brexucabtagene autoleucel treatment, Grade 3 or higher cytopenias not resolved by Day 30 following brexucabtagene autoleucel infusion occurred in 20% (7/35) of the patients and included neutropenia (12%) and thrombocytopenia (12%); Grade 3 or higher cytopenias not resolved by Day 60 following brexucabtagene autoleucel infusion occurred in 11% (4/35) of the patients and included neutropenia (9%) and thrombocytopenia (6%). Monitor blood counts after brexucabtagene autoleucel infusion.
Hypogammaglobulinemia
B cell aplasia and hypogammaglobulinemia can occur in patients receiving treatment with brexucabtagene autoleucel. Hypogammaglobulinemia was reported in 16% (13/82) of patients with MCL and 9% (7/78) of patients with ALL. Monitor immunoglobulin levels after treatment with brexucabtagene autoleucel and manage using infection precautions, antibiotic prophylaxis, and immunoglobulin replacement.
The safety of immunization with live viral vaccines during or following brexucabtagene autoleucel treatment has not been studied. Vaccination with live virus vaccines is not recommended for at least six weeks prior to the start of lymphodepleting chemotherapy, during brexucabtagene autoleucel treatment, and until immune recovery following treatment with brexucabtagene autoleucel.
Secondary Malignancies
Patients treated with TECARTUS may develop secondary malignancies. T cell malignancies have occurred following treatment of hematologic malignancies with BCMA- and CD19-directed genetically modified autologous T cell immunotherapies. Mature T cell malignancies, including CAR-positive tumors, may present as soon as weeks following infusion, and may include fatal outcomes. Monitor life-long for secondary malignancies. In the event that a secondary malignancy occurs, contact Kite at 1-844-454-KITE (5483) to obtain instructions on patient samples to collect for testing.
Effects on Ability to Drive and Use Machines
Due to the potential for neurologic events, including altered mental status or seizures, patients receiving brexucabtagene autoleucel are at risk for altered or decreased consciousness or coordination in the eight weeks following brexucabtagene autoleucel infusion. Advise patients to refrain from driving and engaging in hazardous occupations or activities, such as operating heavy or potentially dangerous machinery, during this initial period.
Specific Populations
Pregnancy
There are no available data with brexucabtagene autoleucel use in pregnant women. No animal reproductive and developmental toxicity studies have been conducted with brexucabtagene autoleucel to assess whether brexucabtagene autoleucel can cause fetal harm when administered to a pregnant woman. It is not known if brexucabtagene autoleucel has the potential to be transferred to the fetus. Based on the mechanism of action of brexucabtagene autoleucel, if the transduced cells cross the placenta, they may cause fetal toxicity, including B cell lymphocytopenia. Therefore, brexucabtagene autoleucel is not recommended for women who are pregnant. Pregnancy after brexucabtagene autoleucel infusion should be discussed with the treating physician.
In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2% – 4% and 15% – 20%, respectively.
Lactation
There is no information regarding the presence of brexucabtagene autoleucel in human milk, the effect on the breastfed infant, and the effects on milk production. The developmental and health benefits of breastfeeding should be considered along with the mother's clinical need for brexucabtagene autoleucel and any potential adverse effects on the breastfed infant from brexucabtagene autoleucel or from the underlying maternal condition.
Females and Males of Reproductive Potential
Pregnancy status of females with reproductive potential should be verified. Sexually active females of reproductive potential should have a negative pregnancy test prior to starting treatment with brexucabtagene autoleucel.
See the Prescribing Information for fludarabine and cyclophosphamide for information on the need for effective contraception in patients who receive the lymphodepleting chemotherapy.
There are insufficient exposure data to provide a recommendation concerning duration of contraception following treatment with brexucabtagene autoleucel.
There are no data on the effect of brexucabtagene autoleucel on fertility.
Pediatric Use
The safety and efficacy of brexucabtagene autoleucel have not been established in pediatric patients.
Geriatric Use
Of the 82 patients treated with brexucabtagene autoleucel for MCL, 42 (51%) were 65 years of age and older. Of the 78 patients treated with brexucabtagene autoleucel for ALL, 12 (15%) were 65 years of age and older. No overall differences in safety or effectiveness were observed between these patients and younger patients.
Common Adverse Effects
-
The most common non-laboratory adverse reactions (incidence ≥20%) in patients with MCL: fever, CRS, hypotension, encephalopathy, fatigue, tachycardia, arrhythmia, infection with pathogen unspecified, chills, hypoxia, cough, tremor, musculoskeletal pain, headache, nausea, edema, motor dysfunction, constipation, diarrhea, decreased appetite, dyspnea, rash, insomnia, pleural effusion, and aphasia.
-
The most common non-laboratory adverse reactions (incidence ≥20%) in patients with ALL: fever, CRS, hypotension, encephalopathy, tachycardia, nausea, chills, headache, fatigue, febrile neutropenia, diarrhea, musculoskeletal pain, hypoxia, rash, edema, tremor, infection with pathogen unspecified, constipation, decreased appetite, and vomiting.
Drug Interactions
Specific Drugs
It is essential that the manufacturer's labeling be consulted for more detailed information on interactions with this drug, including possible dosage adjustments. Interaction highlights:
Please see product labeling for drug interaction information.
Actions
Mechanism of Action
Brexucabtagene autoleucel, a CD19-directed genetically modified autologous T cell immunotherapy, binds to CD19-expressing cancer cells and normal B cells. Studies demonstrated that following anti-CD19 CAR T cell engagement with CD19-expressing target cells, the CD28 and CD3-zeta co-stimulatory domains activate downstream signaling cascades that lead to T cell activation, proliferation, acquisition of effector functions, and secretion of inflammatory cytokines and chemokines. This sequence of events leads to killing of CD19-expressing cells.
Advice to Patients
-
Advise the patient to read the FDA-approved patient labeling (Medication Guide).
-
Ensure that patients understand the risk of manufacturing failure (4% in clinical trial). In case of a manufacturing failure, a second manufacturing of brexucabtagene autoleucel may be attempted. In addition, while the patient awaits the product, additional chemotherapy (not the lymphodepletion) may be necessary and may increase the risk of adverse events during the pre-infusion period.
-
Advise patients to seek immediate attention if cytokine release syndrome (CRS) occurs; signs or symptoms associated with CRS include fever, chills, fatigue, tachycardia, nausea, hypoxia, and hypotension.
-
Advise patients to seek immediate attention if neurologic toxicities occur; signs or symptoms include encephalopathy, seizures, changes in level of consciousness, speech disorders, tremors, and confusion.
-
Advise patients to seek immediate attention if signs or symptoms of severe infections occur.
-
Advise patients to seek immediate attention if signs or symptoms associated with bone marrow suppression, including neutropenia, anemia, thrombocytopenia, or febrile neutropenia, occur.
-
Advise patients that secondary malignancies, including T cell malignancies, have occurred following treatment with BCMA- and CD19-directed genetically modified autologous T cell immunotherapies.
-
Advise patients to refrain from driving or operating heavy or potentially dangerous machinery for at least eight weeks after brexucabtagene autoleucel infusion.
-
Advise patients to have periodic monitoring of blood counts.
-
Advise patients to contact Kite at 1-844-454-KITE (5483) if they are diagnosed with a secondary malignancy.
Additional Information
AHFSfirstRelease™. For additional information until a more detailed monograph is developed and published, the manufacturer's labeling should be consulted. It is essential that the manufacturer's labeling be consulted for more detailed information on usual uses, dosage and administration, cautions, precautions, contraindications, potential drug interactions, laboratory test interferences, and acute toxicity.
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Parenteral |
Suspension, for IV infusion |
2×106 CAR-positive viable T cells per kg of body weight (maximum of 2×108 CAR-positive viable T cells) |
Tecartus (supplied in an infusion bag containing approximately 68 mL of frozen suspension of genetically modified autologous T cells in 5% DMSO and human serum albumin) |
Kite Pharma |
|
1×106 CAR-positive viable T cells per kg of body weight (maximum of 1×108 CAR-positive viable T cells) |
Tecartus (supplied in an infusion bag containing approximately 68 mL of frozen suspension of genetically modified autologous T cells in 5% DMSO and human serum albumin) |
Kite Pharma |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions August 10, 2025. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
Reload page with references included
Related/similar drugs
Frequently asked questions
More about brexucabtagene autoleucel
- Check interactions
- Compare alternatives
- Latest FDA alerts (3)
- Side effects
- Dosage information
- During pregnancy
- Drug class: miscellaneous antineoplastics
- Breastfeeding
- En español