Sepsis in Children
Medically reviewed by Drugs.com. Last updated on Aug 4, 2025.
Sepsis is a condition that develops when your child's immune system reacts too strongly to an infection. The immune system normally fights germs causing an infection. Sepsis develops when the immune system stops attacking germs and starts attacking healthy cells throughout your child's body. This causes a low blood pressure (BP) and inflammation. Sepsis is considered severe if the inflammation affects how one or more of your child's organs work. Sepsis must be treated immediately to prevent septic shock. Septic shock is life-threatening low BP that leads to organ failure.
WHILE YOU ARE HERE:
Informed consent
is a legal document that explains the tests, treatments, or procedures that your child may need. Informed consent means you understand what will be done and can make decisions about what you want. You give your permission when you sign the consent form. You can have someone sign this form for you if you are not able to sign it. You have the right to understand your child's medical care in words you know. Before you sign the consent form, understand the risks and benefits of what will be done to your child. Make sure all of your questions are answered.
Stay with your child for comfort and support
as often as possible while he or she is in the hospital. Ask another family member or someone close to the family to stay with your child when you cannot be there. Bring items from home that will comfort your child, such as a favorite blanket or toy.
Monitoring:
Healthcare providers will closely monitor your child's blood pressure, heart rate, breathing rate, temperature, and pain. An IV line will be used to give medicines or liquid, or to draw blood samples. Providers will also check your child's kidney function by measuring how much he or she is urinating.
Related medications
Tests:
- Blood and urine tests may be done to check your child's blood cell levels, electrolyte levels, and blood sugar levels. These tests will also check for infection, and measure your child's liver and kidney function. A blood gas will show how much oxygen and carbon dioxide is in your child's blood. The results will tell healthcare providers how well your child's lungs, heart, and kidneys are working.
- An x-ray, ultrasound, CT, or MRI may show where in your child's body the infection came from. Your child may be given contrast liquid to help the organs show up better in the pictures. Tell the healthcare provider if your child has ever had an allergic reaction to contrast liquid. Do not let your child enter the MRI room with anything metal. Metal can cause serious injury. Tell the provider if your child has any metal in or on his or her body.
- An echocardiogram is a type of ultrasound. Sound waves are used to show the structure and function of your child's heart. The test will also check for damage to your child's heart valves that may be caused by infection.
- A lumbar puncture (spinal tap) may be done to test your child's cerebrospinal fluid (CSF) for germs. It can also check for signs of infection in or around his or her brain. CSF is the fluid that surrounds your child's spinal column and brain.
Medicines:
Your child may be given medicine to do any of the following:
- Increase his or her blood pressure and blood flow to organs
- Treat the infection causing sepsis
- Control or lower his or her heart rate
- Prevent blood clots
Treatment:
- Removal or change of a catheter or drain may be needed to get rid of the infection.
- IV fluids may be given to treat or prevent dehydration. IV fluids also help increase blood flow to your child's organs, and increase his or her blood pressure.
- Oxygen may be needed if your child's blood oxygen level is lower than it should be. Your child may get oxygen through a mask placed over his or her nose and mouth or through small tubes placed in the nostrils. Ask your child's healthcare provider before you take off the mask or oxygen tubing.
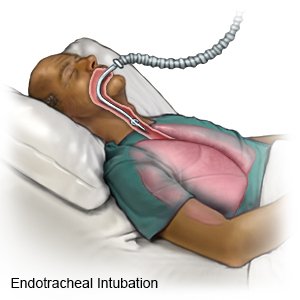
- A ventilator is a machine that gives your child oxygen and breathes for him or her when he or she cannot breathe well. An endotracheal (ET) tube is put into your child's mouth or nose and attached to the ventilator.
- Nutrition support may be needed if your child cannot eat normally. Your child may not be awake, or he or she may have an ET tube that prevents him or her from eating. A feeding tube may be inserted. A feeding tube is a thin tube inserted through your child's nose or mouth into the stomach or small intestine. Formula can be injected through the feeding tube. Instead your child may need nutrition through an IV.
- Pneumatic boots may be applied to your child's legs. The boots have an air pump that tightens and loosens different areas of the boots. This improves blood flow and helps prevent clots.
- A blood transfusion may be needed if bleeding occurs or platelet levels drop. This can happen in severe sepsis.
- Dialysis may be needed if your child's kidneys stop working correctly or are damaged during sepsis. Dialysis is a procedure to remove chemicals, wastes, and extra fluid from your child's blood.
- Surgery may be needed to treat problems causing sepsis. This may include removing an abscess or infected tissue.
Treatment options
The following list of medications are related to or used in the treatment of this condition.
RISKS:
Without treatment, sepsis may develop into septic shock (sepsis with low blood pressure). Multiple organs may shut down. These problems can be life-threatening. Your child's organs may be permanently damaged by septic shock.
CARE AGREEMENT:
You have the right to help plan your child's care. Learn about your child's health condition and how it may be treated. Discuss treatment options with your child's healthcare providers to decide what care you want for your child.© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.
Learn more about Sepsis
Treatment options
- Medications for Infection
- Medications for Sepsis
- Medications for Septicemia
- Medications for Streptococcemia
Care guides
Medicine.com guides (external)
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
