Pancreatic Stent Placement
Medically reviewed by Drugs.com. Last updated on Aug 4, 2025.
AMBULATORY CARE:
What you need to know about pancreatic stent placement:
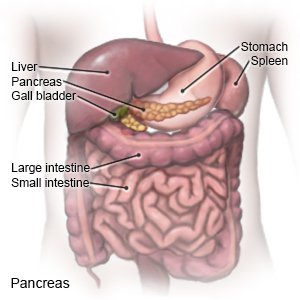
A stent is a small tube used to widen a pancreatic duct and keep it open. Pancreatic fluid normally flows through the ducts. Smaller ducts empty fluid into the main duct. A stent can help treat a narrow, blocked, or leaking duct, or drain extra fluid. One or more stents may be placed before certain procedures to prevent pancreatitis (inflammation of the pancreas). Pancreatic stent placement may be done during endoscopic retrograde cholangiopancreatography (ERCP).
 |
How to prepare for stent placement:
- Your healthcare provider will talk to you about how to prepare for your procedure. He or she may tell you not to eat or drink anything after midnight on the day of your procedure. Tell your provider about all medicines you currently take. He or she will tell you if you need to stop any medicine before your procedure, and when to stop. He or she will tell you which medicines to take or not take on the day of your procedure.
- Tell your provider about all allergies you have. Tell him or her if you had an allergic reaction to a medicine, contrast liquid, anesthesia, or antibiotics.
- Arrange to have someone drive you home from your procedure.
What will happen during stent placement:
- You will be given medicines to help you relax, make you drowsy, and prevent coughing or gagging. Your healthcare provider will insert the endoscope into your mouth. An endoscope is a long tube with a camera and a light. The provider will move the endoscope until it reaches your small intestines. He or she will use the camera to find the opening to the duct.
- Your provider may use a balloon to widen the duct. He or she will guide a wire into the duct. The stent will be put into the duct over the wire. Fluid may be removed. Contrast liquid will be injected to make the duct and stent easier to see in pictures. The pictures will help make sure the stent is in the correct position.
What to expect after stent placement:
- You may have a sore throat for a day or two.
- You may have abdominal pain or feel bloated. You may also feel nauseated. These symptoms should go away in a few hours.
- You will need to have x-rays 3 to 4 weeks after the procedure to make sure the stent it still in place.
Risks of pancreatic stent placement:
The endoscope or tools may damage your pancreas or the duct. The stent may move out of place or block the duct. The stent may become stuck in your small bowel. The procedure may not work and you may need to have another stent placed.
Related medications
Call your local emergency number (911 in the US) if:
- You have chest pain.
- You have sudden or severe trouble breathing.
Call your doctor if:
- You have severe pain in your throat 2 days after the procedure.
- You have trouble swallowing.
- You have severe abdominal pain or your abdomen is larger than usual.
- You faint.
- You vomit blood or something that looks like coffee grounds.
- You have blood in your bowel movements, or your bowel movements look like tar.
- You have a fever or chills.
- You have nausea or are vomiting.
- You have questions or concerns about your condition or care.
Medicines:
- Prescription pain medicine may be given. Ask your healthcare provider how to take this medicine safely. Some prescription pain medicines contain acetaminophen. Do not take other medicines that contain acetaminophen without talking to your healthcare provider. Too much acetaminophen may cause liver damage. Prescription pain medicine may cause constipation. Ask your healthcare provider how to prevent or treat constipation.
- Take your medicine as directed. Contact your healthcare provider if you think your medicine is not helping or if you have side effects. Tell your provider if you are allergic to any medicine. Keep a list of the medicines, vitamins, and herbs you take. Include the amounts, and when and why you take them. Bring the list or the pill bottles to follow-up visits. Carry your medicine list with you in case of an emergency.
Self-care:
- Rest when you feel it is needed. You may be drowsy for up to 24 hours after your procedure. Return to your daily activities as directed.
- Drink liquids as directed. Liquids will help flush the contrast liquid from your body. Ask how much liquid to drink each day and which liquids are best for you.
- Ask when you can eat regular foods. Healthy foods include fruits, vegetables, whole-grain breads, low-fat dairy products, beans, lean meats, and fish. Eat small meals more often. This may help prevent nausea.
- Relieve a sore throat with ice chips, liquids, or lozenges as directed.
- Do not take aspirin after your procedure unless your healthcare provider says it is okay. Aspirin may increase your risk for bleeding.
Follow up with your healthcare provider as directed:
You will need to return in 3 to 4 weeks to make sure the stent is still in the right place. Write down your questions so you remember to ask them during your visits.
© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
