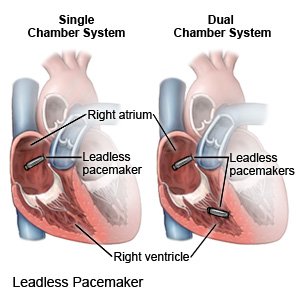
Leadless Pacemaker
Medically reviewed by Drugs.com. Last updated on Aug 4, 2025.
A leadless pacemaker is a small device that helps control a slow or irregular heartbeat. The device sends electrical impulses are sent to your heart when needed. A leadless pacemaker uses battery power instead of a generator. This means it is not attached to wires. You may need a single-chamber or dual-chamber pacemaker. Single chamber means 1 device is placed in your right ventricle. Dual chamber means a second device is placed in your right atrium. The 2 devices of the dual-chamber system work together to regulate your heartbeat.
 |
DISCHARGE INSTRUCTIONS:
Call your local emergency number (911 in the US), or have someone call if:
- You have any of the following signs of a heart attack:
- Squeezing, pressure, or pain in your chest
- You may also have any of the following:
- Discomfort or pain in your back, neck, jaw, stomach, or arm
- Shortness of breath
- Nausea or vomiting
- Lightheadedness or a sudden cold sweat
- You feel lightheaded, short of breath, or have chest pain.
- You cough up blood.
Seek care immediately if:
- Your arm or leg feels warm, tender, and painful. It may look swollen and red.
- You feel weak, dizzy, or faint.
- Your pulse is lower or higher than your healthcare provider said it should be.
- The catheter site is painful, red, swollen, or draining pus.
Call your doctor or cardiologist if:
- You have a fever or chills.
- You have questions or concerns about your condition or care.
Related medications
Care for the catheter site as directed:
You may have a bruise or swelling where the catheter went into your skin. The site may be sore or tender. These symptoms are normal and should go away in a few days. Your healthcare provider may give you specific instructions to follow while you heal. Ask your provider when you can remove your bandage. The following are general guidelines to follow after you remove the bandage:
- Wash around the site with soap and water starting 2 days after the procedure. It is okay to let soap and water run over the site, but do not scrub it . Gently pat the site dry. Then apply new, clean bandages as directed.
- Check the site every day. Look for signs of infection, such as redness, swelling, or pus.
- Apply pressure to stop bleeding from the site. Use a clean gauze or towel to apply pressure for 5 to 10 minutes. Call your local emergency number (911 in the US) if bleeding becomes heavy or does not stop.
Activity:
Ask your healthcare provider how long to follow these and other safety precautions given to you:
- Ask when you can return to your regular daily activities. Your provider will tell you when you can go back to work, drive, or do other activities.
- Ask when you can play sports or be physically active. Your provider may tell you not to play contact sports or do vigorous exercises. Do not lift anything heavier than your provider says is okay.
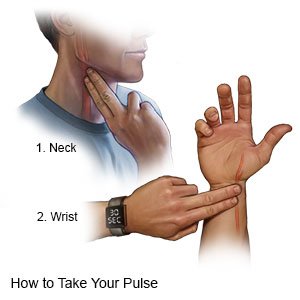
- Check your pulse as directed. Check while you are resting.
- Use a watch with a second hand. Count your pulse for 60 seconds.
- Use your index and middle fingers. Place your fingers on the inside of your wrist. You should feel your pulse beating just below your thumb. You may instead check on one side of your neck. You should feel your pulse beating where your neck meets your jaw.
- Record your information. Include your pulse rate, the date, time, and which side was used to take the pulse. Include anything you notice about your pulse, such as that it is weak, strong, or missing beats. Bring a copy of the information to your follow-up visits.
Pacemaker safety:
Your healthcare provider will give you specific instructions based on your pacemaker. The following are general guidelines:
- Stay away from magnets or machines with electric fields. These can interfere with how your pacemaker works. You will get specific safety information based on the type of pacemaker you have. The following are general safety guidelines:
- Do not lean into a car engine or do welding.
- Do not use an electronic body fat scale or electronic abdominal stimulating exercise machine.
- Check before you have CT, PET, or MRI to make sure it is safe with your pacemaker.
- Check before you have electrolysis for hair removal.
- Check before you use a medical alert system, or let your company know you have a pacemaker. The company will be able to tell you if a pacemaker is safe to use with the system.
- Avoid or limit time around electric fence systems. This also includes electric systems to keep pets in a small area. If you cannot avoid it, make your time near it as short as possible.
- Keep your cell phone away from your pacemaker. Do not place your cell phone in a breast pocket over your pacemaker site. Use your cell phone with the ear on the opposite side from your pacemaker.
- Keep headphones away from your pacemaker. Earbud and clip-on headphones for MP3 players might interfere with your pacemaker. Make sure your headphones are always at least 6 inches away from the pacemaker. Do not put headphones in your shirt pocket over the pacemaker. Do not let the headphones hang from your neck onto your chest. Do not let anyone who is using headphones put his or her head on your chest.
- Tell airport security that you have a pacemaker before you go through the metal detectors. Metal detectors may beep because of the metal in your pacemaker. Step away from the machine if you feel dizzy or your heart rate increases. Ask the security agents not to hold a security wand over your pacemaker for more than a few seconds. Your pacemaker function or programming may be affected by the wand.
- Wear medical alert identification. Wear medical alert jewelry or carry a card that says you have a pacemaker. Ask your provider where to get these items.

Pacemaker care:
- Your healthcare provider will check your pacemaker at least every 3 months. Your provider will tell you how often to have the pacemaker checked. A leadless pacemaker lasts about 10 years.
- The battery will need to be replaced in 5 to 15 years. This depends on how often your pacemaker needs to regulate your heartbeat. Your provider will monitor you and decide when these parts need to be replaced.
Follow up with your doctor or cardiologist as directed:
You will need regular checks to make sure your pacemaker is working correctly. You may also need regular EKGs to check the electrical activity of your heart. Write down your questions so you remember to ask them during your visits.
© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
