Laparoscopic Liver Biopsy
Medically reviewed by Drugs.com. Last updated on Aug 4, 2025.
AMBULATORY CARE:
What you need to know about a laparoscopic liver biopsy:
A laparoscopic liver biopsy is surgery to remove a sample of tissue from your liver. The sample can be sent to a lab and tested for liver disease, cancer, or infection.
 |
How to prepare for a laparoscopic liver biopsy:
- Your healthcare provider will talk to you about how to prepare for your surgery. You may need to have your blood tested before surgery. A blood test can check how well your blood clots. Your blood needs to clot correctly to prevent heavy bleeding during surgery.
- The provider may tell you not to eat or drink anything after midnight on the day of your surgery. He or she will tell you what medicines to take or not take on the day of your surgery. You may need to stop taking blood thinners, NSAIDs, or aspirin several days before surgery. You may be given an antibiotic before surgery to help prevent a bacterial infection. Tell your healthcare provider if you have ever had an allergic reaction to an antibiotic.
- Arrange for someone to drive you home and stay with you after surgery. This person can help you around the house and watch you for any problems.
What will happen during a laparoscopic liver biopsy:
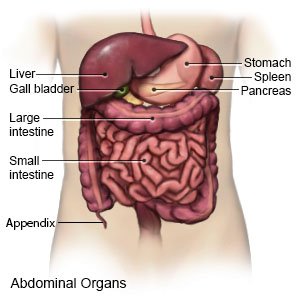
- You will be given general anesthesia to keep you asleep and free from pain during surgery. Your healthcare provider will make an incision in your abdomen and insert a laparoscope. A laparoscope is a long metal tube with a light and camera on the end. Your healthcare provider will also insert other tools through 2 to 3 smaller incisions made at different places on your abdomen.

- Your abdomen will then be inflated with a gas (carbon dioxide). This lifts your abdomen away from your organs and gives your healthcare provider more space to work. He or she will use the tools to remove 1 or more samples of tissue from your liver. Your healthcare provider will close your incisions with glue or steristrips and cover them with a bandage.
What will happen after a laparoscopic liver biopsy:
Healthcare providers will monitor you for problems such as bleeding. Do not get out of bed until your healthcare provider says it is okay. You may be able to go home the same day, or you may need to spend a night in the hospital. You may have pain in your abdomen or right shoulder. These symptoms should get better in 48 to 72 hours.
Risks of a laparoscopic liver biopsy:
You may bleed more than expected or get an infection. Biopsy tools may cause a hole in your liver. This may cause blood or bile to leak into your abdomen. You may need other treatments to fix these problems.
Call your local emergency number (911 in the US) if:
- You have trouble breathing.
Related medications
Seek care immediately if:
- Blood soaks through your bandage.
- Your stitches come apart.
- You have severe pain.
- Your abdomen is larger than usual and feels firm.
Call your surgeon or doctor if:
- You have a fever or chills.
- Your pain does not get better after you take pain medicine.
- Your incisions are red, swollen, or draining pus.
- You have nausea or are vomiting.
- Your skin is itchy, swollen, or you have a rash.
- You have questions or concerns about your condition or care.
Medicines:
You may need any of the following:
- Acetaminophen decreases pain and fever. It is available without a doctor's order. Ask how much to give your child and how often to give it. Follow directions. Read the labels of all other medicines your child uses to see if they also contain acetaminophen, or ask your child's doctor or pharmacist. Acetaminophen can cause liver damage if not taken correctly.
- Prescription pain medicine may be given. Ask your healthcare provider how to take this medicine safely. Some prescription pain medicines contain acetaminophen. Do not take other medicines that contain acetaminophen without talking to your healthcare provider. Too much acetaminophen may cause liver damage. Prescription pain medicine may cause constipation. Ask your healthcare provider how to prevent or treat constipation.
- Take your medicine as directed. Contact your healthcare provider if you think your medicine is not helping or if you have side effects. Tell your provider if you are allergic to any medicine. Keep a list of the medicines, vitamins, and herbs you take. Include the amounts, and when and why you take them. Bring the list or the pill bottles to follow-up visits. Carry your medicine list with you in case of an emergency.
Care for your incision site as directed:
Carefully wash around the incision site with soap and water. Let the soap and water run over your incision site. Gently pat the area dry and put on new, clean bandages as directed. Change your bandages when they get wet or dirty. If you have steristrips, let them fall off on their own. If they do not fall off after 10 to 14 days, gently peel them off. Check your incisions every day for redness, swelling, or pus. Do not put powders or lotions on your incision sites until your healthcare provider says it is okay.
Self-care:
- Rest as directed. Do not exercise or lift anything heavier than 5 pounds for as long as directed. Take short walks around the house to prevent blood clots.
- Ask your healthcare provider when to take your blood thinner or antiplatelet medicine. You may need to wait 24 to 72 hours to take your medicine. This will prevent bleeding.
Follow up with your surgeon or doctor as directed:
Write down your questions so you remember to ask them during your visits.
© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
