Deep Vein Thrombosis Prevention
Medically reviewed by Drugs.com. Last updated on Aug 4, 2025.
Some conditions increase your risk for a DVT. These include a family history of blood clots or a blood clotting disorder, such as factor V Leiden. Lack of activity, cigarette smoking, obesity, and birth control pills can also increase the risk. You can lower your risk by following the directions from your doctor or specialist. You can also make lifestyle changes to prevent blood clots.
 |
DISCHARGE INSTRUCTIONS:
Call your local emergency number (911 in the US) or have someone call if:
- You feel lightheaded, short of breath, and have chest pain.
- You cough up blood.
Return to the emergency department if:
- Your arm or leg feels warm, tender, and painful. It may look swollen and red.
Call your doctor or hematologist if:
- You have questions or concerns about your condition or care.
Related medications
Medicines:
- Blood thinners help prevent blood clots. Clots can cause strokes, heart attacks, and death. Many types of blood thinners are available. Your healthcare provider will give you specific instructions for the type you are given. The following are general safety guidelines to follow while you are taking a blood thinner:
- Watch for bleeding and bruising. Watch for bleeding from your gums or nose. Watch for blood in your urine and bowel movements. Use a soft washcloth on your skin, and a soft toothbrush to brush your teeth. This can keep your skin and gums from bleeding. If you shave, use an electric shaver. Do not play contact sports.
- Tell your dentist and other healthcare providers that you take a blood thinner. Wear a bracelet or necklace that says you take this medicine.
- Do not start or stop any other medicines or supplements unless your healthcare provider tells you to. Many medicines and supplements cannot be used with blood thinners.
- Take your blood thinner exactly as prescribed by your healthcare provider. Do not skip a dose or take less than prescribed. Tell your provider right away if you forget to take your blood thinner, or if you take too much.
- Take your medicine as directed. Contact your healthcare provider if you think your medicine is not helping or if you have side effects. Tell your provider if you are allergic to any medicine. Keep a list of the medicines, vitamins, and herbs you take. Include the amounts, and when and why you take them. Bring the list or the pill bottles to follow-up visits. Carry your medicine list with you in case of an emergency.
What you can do to prevent a DVT:
- Do not smoke. Nicotine and other chemicals in cigarettes and cigars can damage blood vessels and increase your risk for a DVT. Ask your healthcare provider for information if you currently smoke and need help to quit. E-cigarettes or smokeless tobacco still contain nicotine. Talk to your healthcare provider before you use these products.
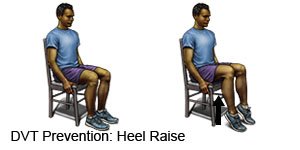
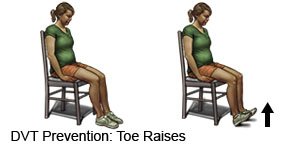
- Change your body position or move around often. Move and stretch in your seat several times each hour if you travel by car or work at a desk. In an airplane, get up and walk every hour. Move your legs by tightening and releasing your leg muscles while sitting. You can also move your legs while sitting by raising and lowering your heels. Keep your toes on the floor while you do this. You can also raise and lower your toes while keeping your heels on the floor.
- Exercise regularly to help increase your blood flow. Walking is a good low-impact exercise. Talk to your healthcare provider about the best exercise plan for you.
- Maintain a healthy weight. Ask your healthcare provider what a healthy weight is for you. Ask your provider to help you create a safe weight loss plan, if needed.
- Ask about birth control if you take the pill. Birth control pills increase the risk for blood clots if you are older than 35, smoke cigarettes, or have a clotting disorder. Talk to your provider about other ways to prevent pregnancy, such as a cervical cap or intrauterine device (IUD).
What you can do to prevent another DVT:
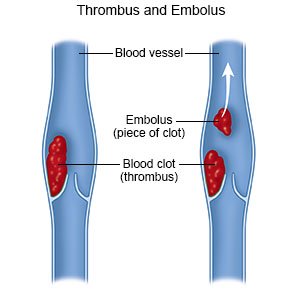
After you have a DVT, your risk for blood clots will always be higher. The following can help lower your risk:
- Take medicines as directed. Your healthcare provider may recommend blood thinners and other medicines to help prevent blood clots. It is important not to skip doses. The medicine may not be able to prevent blood clots if the amount in your blood goes too low.
- Wear a compression device as directed. Examples include pressure stockings, intermittent pneumatic compression, and sequential compression devices. A compression device puts pressure on your lower legs to help keep blood from pooling in your leg veins. Your healthcare provider can prescribe the right device for you. Do not buy over-the-counter devices unless your provider says it is okay. They may not fit correctly or may have elastic that cuts off your circulation. Ask your provider when to start wearing a compression device and how long to wear it.

- Get up and move as directed after surgery or an injury, or during an illness. Early and regular movement can help decrease your risk for a DVT by helping to increase your blood flow. Ask your healthcare provider what type of activity you need and how often you should do it.
Follow up with your doctor or hematologist as directed:
You may need to come in regularly for scans to check for blood clots. Your blood may checked to see how long it takes to clot. Your doctor or hematologist will tell you if you need to have this test and how often to have it. Write down your questions so you remember to ask them during your visits.
© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
