Indapamide
Generic name: indapamide [ in-DAP-a-mide ]
Brand name: Lozol
Dosage form: oral tablet (1.25 mg; 2.5 mg)
Drug class: Thiazide diuretics
What is indapamide?
Indapamide is a thiazide diuretic (water pill) that helps prevent your body from absorbing too much salt, which can cause fluid retention.
Indapamide treats fluid retention (edema) in people with congestive heart failure. indapamide is also used to treat high blood pressure (hypertension).
Indapamide may also be used for purposes not listed in this medication guide.
Indapamide side effects
Get emergency medical help if you have signs of an allergic reaction: hives; difficulty breathing; swelling of your face, lips, tongue, or throat.
Call your doctor at once if you have signs of an electrolyte imbalance, such as:
-
drowsiness, lack of energy, feeling tired;
-
leg cramps, muscle weakness or limp feeling;
-
severe weakness, loss of coordination, feeling unsteady;
-
fast or irregular heartbeats, fluttering in your chest, feeling restless;
-
numbness or tingling;
-
headache, confusion, slurred speech;
-
a light-headed feeling, like you might pass out;
-
dry mouth, increased thirst; or
-
little or no urinating.
Common side effects of indapamide may include:
-
dizziness;
-
weakness, tiredness;
-
back pain, muscle cramps;
-
feeling anxious or agitated;
-
headache; or
-
runny nose.
This is not a complete list of side effects and others may occur. Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
Related/similar drugs
Warnings
You should not use indapamide if you are allergic to sulfa drugs or if you are unable to urinate.
Before taking this medicine
You should not use indapamide if you are allergic to it, or if:
-
you are unable to urinate; or
-
you are allergic to sulfa drugs.
To make sure indapamide is safe for you, tell your doctor if you have:
-
cirrhosis or other liver disease;
-
kidney disease;
-
low levels of potassium or sodium in your blood;
-
gout;
-
diabetes;
-
lupus; or
-
if you are on a low-salt diet.
Indapamide is not expected to be harmful to an unborn baby. Tell your doctor if you are pregnant or plan to become pregnant.
It is not known whether indapamide passes into breast milk or if it could harm a nursing baby. You should not breast-feed while using this medicine.
Indapamide is not approved for use by anyone younger than 18 years old.
How should I take indapamide?
Follow all directions on your prescription label. Your doctor may occasionally change your dose to make sure you get the best results. Do not use indapamide in larger or smaller amounts or for longer than recommended.
Indapamide is usually taken once per day in the morning. Follow your doctor's dosing instructions very carefully.
Call your doctor if you have ongoing vomiting or diarrhea, or if you are sweating more than usual. You can easily become dehydrated while taking this medicine, which can lead to severely low blood pressure or a serious electrolyte imbalance.
While using indapamide, you may need frequent medical tests and blood pressure checks. Your blood and urine may both be tested if you have been vomiting or are dehydrated.
If you are being treated for high blood pressure, keep using this medicine even if you feel well. High blood pressure often has no symptoms. You may need to use blood pressure medicine for the rest of your life.
Store at room temperature away from moisture, heat, and light. Keep the bottle tightly closed when not in use.
Indapamide dosing information
Usual Adult Dose for Edema:
Initial dose: 2.5 mg orally once a day.
Usual Adult Dose for Hypertension:
Initial dose: 1.25 mg orally once a day.
What happens if I miss a dose?
Take the missed dose as soon as you remember. Skip the missed dose if it is almost time for your next scheduled dose. Do not take extra medicine to make up the missed dose.
What happens if I overdose?
Seek emergency medical attention or call the Poison Help line at 1-800-222-1222.
Overdose symptoms may include vomiting, weakness, dizziness, dry mouth, thirst, and muscle pain or weakness.
What should I avoid while taking indapamide?
Avoid becoming overheated or dehydrated during exercise, in hot weather, or by not drinking enough fluids. Follow your doctor's instructions about the type and amount of liquids you should drink. In some cases, drinking too much liquid can be as unsafe as not drinking enough.
What other drugs will affect indapamide?
Tell your doctor about all your current medicines and any you start or stop using, especially:
-
digoxin, digitalis;
-
lithium;
-
blood pressure medication; or
-
steroids (prednisone and others).
This list is not complete. Other drugs may interact with indapamide, including prescription and over-the-counter medicines, vitamins, and herbal products. Not all possible interactions are listed in this medication guide.
More about indapamide
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (29)
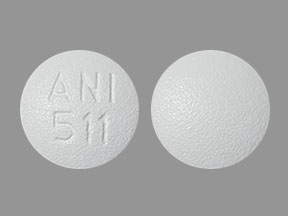
- Drug images
- Side effects
- Dosage information
- During pregnancy
- Drug class: thiazide diuretics
- Breastfeeding
- En español
Patient resources
Other brands
Professional resources
Other brands
Related treatment guides
Further information
Remember, keep this and all other medicines out of the reach of children, never share your medicines with others, and use this medication only for the indication prescribed.
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
Copyright 1996-2025 Cerner Multum, Inc. Version: 8.01.