Estradiol / Norgestimate Side Effects
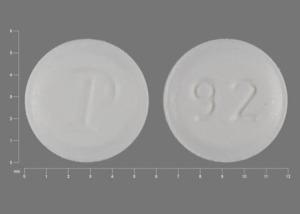
Applies to estradiol / norgestimate: oral tablet.
Important warnings
This medicine can cause some serious health issues
You should not use this medicine if you have had a hysterectomy, or if you have: undiagnosed vaginal bleeding, liver disease, a bleeding disorder, if you will have major surgery, or if you have ever had a heart attack, a stroke, a blood clot, or cancer of the breast, uterus/cervix, or vagina.
Do not use if you are pregnant.
Estradiol and norgestimate may increase your risk of developing a condition that may lead to uterine cancer. Report any unusual vaginal bleeding right away.
Using this medicine can increase your risk of blood clots, stroke, heart attack, or cancer of the breast, uterus, or ovaries. Estradiol and norgestimate should not be used to prevent heart disease, stroke, or dementia.
Get emergency medical help if you have signs of an allergic reaction: hives; difficult breathing; swelling of your face, lips, tongue, or throat.
Call your doctor at once if you have:
-
heart attack symptoms--chest pain or pressure, pain spreading to your jaw or shoulder, nausea, sweating;
-
signs of a stroke--sudden numbness or weakness (especially on one side of the body), sudden severe headache, slurred speech, problems with vision or balance;
-
signs of a blood clot--sudden vision loss, stabbing chest pain, feeling short of breath, coughing up blood, pain or warmth in one or both legs;
-
swelling or tenderness in your stomach;
-
jaundice (yellowing of the skin or eyes);
-
memory problems, confusion, unusual behavior;
-
unusual vaginal bleeding, pelvic pain;
-
a lump in your breast; or
-
high levels of calcium in your blood--nausea, vomiting, constipation, increased thirst or urination, muscle weakness, bone pain, lack of energy.
Common side effects may include:
-
nausea, vomiting, bloating, stomach cramps;
-
fluid retention (swelling, rapid weight gain);
-
headache;
-
breast pain;
-
thinning scalp hair; or
-
vaginal itching or discharge, changes in your menstrual periods, breakthrough bleeding.
This is not a complete list of side effects and others may occur. Call your doctor for medical advice about side effects.
See also:
For healthcare professionals
Applies to estradiol / norgestimate: oral tablet.
Nervous system adverse events
- Very common (10% or more): Headache (23%)
- Common (1% to 10%): Dizziness[Ref]
Immunologic
- Very common (10% or more): Upper respiratory tract infection (21%)
- Common (1% to 10%): Sinusitis, pharyngitis, viral infection[Ref]
Genitourinary
- Very common (10% or more): Breast pain (16%)
- Common (1% to 10%): Vaginal bleeding (all), dysmenorrhea[Ref]
Gastrointestinal
- Very common (10% or more): Abdominal pain (12%)
- Common (1% to 10%): Nausea, flatulence, tooth disorder[Ref]
Musculoskeletal
Other
Psychiatric
- Common (1% to 10%): Depression[Ref]
Respiratory
- Common (1% to 10%): Coughing[Ref]
References
1. Steiger MJ, Quinn NP (1991) "Hormone replacement therapy induced chorea." BMJ, 302, p. 762
2. (2001) "Product Information. Ortho-Prefest (estradiol-norgestimate)." Ortho McNeil Pharmaceutical
3. (2017) "Product Information. Prefest (estradiol-norgestimate)." Barr Pharmaceuticals Inc
4. Auerbach R, Mittal K, Schwartz PE (1988) "Estrogen and progestin receptors in an ovarian ependymoma." Obstet Gynecol, 71, p. 1043-5
5. Julian TM (1987) "Pseudoincontinence secondary to unopposed estrogen replacement in the surgically castrate premenopausal female." Obstet Gynecol, 70, p. 382-3
6. Boston Collaborative Drug Surveilance Program (1974) "Surgically confirmed gallbladder disease, venous thromboembolism, and breast tumors in relation to postmenopausal estrogen therapy." N Engl J Med, 290, p. 15-9
7. (2002) "Risks and benefits of estrogen plus progestin in healthy postmenopausal women: principal results From the Women's Health Initiative randomized controlled trial." JAMA, 288, p. 321-33
8. (2002) "Hormone replacement therapy." Med Lett Drugs Ther, 44, p. 78
More about estradiol / norgestimate
- Check interactions
- Compare alternatives
- Reviews (1)
- Dosage information
- During pregnancy
- Drug class: sex hormone combinations
Professional resources
Other brands
Related treatment guides
Further information
Estradiol/norgestimate side effects can vary depending on the individual. Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
Note: Medication side effects may be underreported. If you are experiencing side effects that are not listed, submit a report to the FDA by following this guide.