Biaxin Side Effects
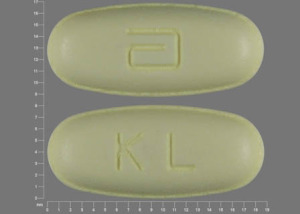
Generic name: clarithromycin
Medically reviewed by Drugs.com. Last updated on Sep 16, 2024.
Note: This document provides detailed information about Biaxin Side Effects associated with clarithromycin. Some dosage forms listed on this page may not apply specifically to the brand name Biaxin.
Applies to clarithromycin: oral powder for suspension, oral tablet, oral tablet extended release.
Precautions
It is very important that your doctor check your or your child's progress at regular visits to make sure this medicine is working properly. Blood and urine tests may be needed to check for unwanted effects.
Do not use this medicine if you or your child are also using astemizole (Hismanal®), cisapride (Propulsid®), lomitapide (Juxtapid®), lovastatin (Mevacor®), pimozide (Orap®), simvastatin (Zocor®), terfenadine (Seldane®), or certain ergot medicines (eg, dihydroergotamine, ergotamine, D.H.E. 45®, Ergomar®, Ergostat®, or Migranal®). If you have kidney or liver disease, do not take this medicine together with colchicine (Colcrys®). Using these medicines together may increase the risk for more serious side effects.
If your or your child's symptoms do not improve within a few days, or if they become worse, check with your doctor.
Make sure your doctor knows if you are pregnant or planning to become pregnant. If you become pregnant while using this medicine, tell your doctor right away.
This medicine may cause serious allergic reactions, including anaphylaxis, which can be life-threatening and require immediate medical attention. Call your doctor right away if you or your child have a rash, itching, hoarseness, trouble breathing or swallowing, or any swelling of your hands, face, mouth, or throat while you or your child are using this medicine.
Serious skin reactions can occur with this medicine. Check with your doctor right away if you or your child have blistering, peeling, or loosening of the skin, red skin lesions, severe acne or skin rash, sores or ulcers on the skin, or fever or chills while you or your child are using this medicine.
Check with your doctor right away if you or your child have pain or tenderness in the upper stomach, pale stools, dark urine, loss of appetite, nausea, unusual tiredness or weakness, or yellow eyes or skin. These could be symptoms of a serious liver problem.
Contact your doctor right away if you have any changes to your heart rhythm. You might feel dizzy or faint, or you might have a fast, pounding, or uneven heartbeat. Make sure your doctor knows if you or anyone in your family has ever had a heart rhythm problem, such as QT prolongation.
Clarithromycin may increase the risk for heart and blood vessel problems in patients with these conditions. It may occur a year or 10 years after the use of this medicine. Talk to your doctor if you have concerns about this risk.
This medicine may cause diarrhea, and in some cases it can be severe. It may occur 2 months or more after you or your child Stop taking clarithromycin (the active ingredient contained in Biaxin). Do not take any medicine to treat diarrhea without first checking with your doctor. Diarrhea medicines may make the diarrhea worse or make it last longer. If you have any questions or if mild diarrhea continues or gets worse, check with your doctor.
This medicine may make you dizzy or confused. Do not drive or do anything else that could be dangerous until you know how this medicine affects you.
Do not take other medicines unless they have been discussed with your doctor. This includes prescription or nonprescription (over-the-counter [OTC]) medicines and herbal or vitamin supplements.
Serious side effects of Biaxin
Along with its needed effects, clarithromycin may cause some unwanted effects. Although not all of these side effects may occur, if they do occur they may need medical attention.
Check with your doctor immediately if any of the following side effects occur while taking clarithromycin:
Less common side effects
- chills
- cough
- fever
- hoarseness
- lower back or side pain
- painful or difficult urination
Rare side effects
- fever with or without chills
- itching, skin rash
- nausea
- severe stomach cramps and pain
- stomach tenderness
- unusual bleeding or bruising
- vomiting
- watery and severe diarrhea, which may also be bloody
- yellow eyes or skin
Incidence not known
- anxiety
- black, tarry stools
- blistering, peeling, or loosening of the skin
- blurred vision
- chest pain or discomfort
- clay-colored stools
- confusion about identity, place, and time
- cool, pale skin
- dark urine
- depression
- difficulty with swallowing
- dizziness
- fainting
- fast, slow, pounding, or irregular heartbeat or pulse
- feeling of unreality
- feeling that others are watching you or controlling your behavior
- feeling that others can hear your thoughts
- feeling, seeing, or hearing things that are not there
- hives
- increased hunger
- joint or muscle pain
- light-colored stools
- loss of appetite
- nightmares
- puffiness or swelling of the eyelids or around the eyes, face, lips, or tongue
- recurrent fainting
- red skin lesions, often with a purple center
- red, irritated eyes
- redness, swelling, or soreness of the tongue
- seizures
- sense of detachment from self or body
- severe mood or mental changes
- shakiness
- skin eruptions
- slurred speech
- sore throat
- sores, ulcers, or white spots in the mouth or on the lips
- stomach pain
- swollen glands
- tightness in the chest
- unpleasant breath odor
- unusual behavior
- unusual tiredness or weakness
- vomiting of blood
Other side effects of Biaxin
Some side effects of clarithromycin may occur that usually do not need medical attention. These side effects may go away during treatment as your body adjusts to the medicine. Also, your health care professional may be able to tell you about ways to prevent or reduce some of these side effects.
Check with your health care professional if any of the following side effects continue or are bothersome or if you have any questions about them:
Less common side effects
- belching
- bloated or full feeling
- change in sensation of taste
- excess air or gas in the stomach or bowels
- headache
- heartburn
- indigestion
- mild diarrhea
- passing gas
Incidence not known
- change in sense of smell
- continuing ringing or buzzing or other unexplained noise in the ears
- feeling of constant movement of self or surroundings
- hearing loss
- lightheadedness
- loss of taste
- mood or mental changes
- sensation of spinning
- shakiness in the legs, arms, hands, or feet
- sore mouth or tongue
- swelling or inflammation of the mouth
- tongue discoloration
- tooth discoloration
- trouble sleeping
- weight loss
See also:
For healthcare professionals
Applies to clarithromycin: oral powder for reconstitution, oral tablet, oral tablet extended release.
General adverse events
The most common side effects were abdominal pain/discomfort, diarrhea, nausea, vomiting, and dysgeusia/taste perversion.
In immunocompromised patients treated with higher doses of this drug (1 to 2 g/day), the most common side effects were nausea, vomiting, taste perversion, abdominal pain, diarrhea, rash, flatulence, headache, constipation, hearing disturbance, increased AST, and increased ALT.[Ref]
Nervous system
- Very common (10% or more): Dysgeusia/taste perversion (up to 16%)
- Common (1% to 10%): Headache, dizziness
- Uncommon (0.1% to 1%): Loss of consciousness, dyskinesia, somnolence, hearing impaired, tinnitus, tremor, vertigo
- Frequency not reported: New onset of symptoms of myasthenic syndrome, exacerbation of symptoms of myasthenia gravis, hearing disturbance, muzziness
- Postmarketing reports: Convulsions, ageusia, parosmia/smell perversion, anosmia, paresthesia, deafness, hyperkinesia[Ref]
Deafness was reported mainly in elderly women and was usually reversible.[Ref]
Gastrointestinal
- Very common (10% or more): Nausea (up to 12.3%)
- Common (1% to 10%): Diarrhea, vomiting, abdominal pain/discomfort, dyspepsia/heartburn, flatulence, oral candidiasis/moniliasis, constipation
- Uncommon (0.1% to 1%): Glossitis, stomatitis, esophagitis, gastroesophageal reflux disease, gastritis, proctalgia, abdominal distension, dry mouth, eructation, gastroenteritis, gastrointestinal hemorrhage, bleeding gums, bloodstained stools
- Frequency not reported: Clostridium difficile-associated diarrhea (ranging from mild diarrhea to fatal colitis), pancreatitis
- Postmarketing reports: Acute pancreatitis, tongue discoloration, tooth discoloration, pseudomembranous colitis, enteritis[Ref]
The incidence of dry mouth was similar for patients treated with 1 to 2 g/day, but was generally about 3 to 4 times as frequent for those treated with 4 g/day.
Severity of pseudomembranous colitis has ranged from mild to life-threatening.
Tooth discoloration was usually reversible with professional dental cleaning after the drug was stopped.[Ref]
Local
- Very common (10% or more): Injection site phlebitis
- Common (1% to 10%): Injection site pain, injection site inflammation, tenderness at site of administration
- Frequency not reported: Vessel puncture site pain
These side effects are specific to the IV formulation.
Hepatic
- Common (1% to 10%): Elevated AST, elevated ALT, abnormal liver function test
- Uncommon (0.1% to 1%): Cholestasis, hepatitis (symptoms included anorexia, jaundice, dark urine, pruritus, tender abdomen), increased blood bilirubin, elevated GGT, elevated direct bilirubin, hepatic dysfunction (including increased liver enzymes), hepatitis and cholestasis with or without jaundice
- Frequency not reported: Hepatocellular and/or cholestatic hepatitis (with or without jaundice), drug-induced hepatotoxicity, fulminant hepatic failure
- Postmarketing reports: Hepatic failure, hepatocellular jaundice, adverse reactions related to hepatic dysfunction, abnormal hepatic function, liver abnormalities[Ref]
Elevated AST (greater than 5 times the upper limit of normal [5 x ULN]) and ALT (greater than 5 x ULN) were reported in up to 4% and up to 3% of patients, respectively.
Hepatic dysfunction (sometimes severe and usually reversible), including increased liver enzymes, and hepatocellular and/or cholestatic hepatitis, with or without jaundice have been reported. In some instances, hepatic failure with fatal outcome has been reported and generally has been associated with serious underlying diseases (e.g., preexisting liver disease) and/or concomitant medications (e.g., hepatotoxic agents).
Drug-induced hepatotoxicity was rare and typically associated with higher doses (1 to 2 g/day) and high serum drug levels. The enzyme elevation pattern was usually cholestatic with minimal elevations of AST and ALT.[Ref]
Hypersensitivity
- Common (1% to 10%): Anaphylactoid reaction
- Uncommon (0.1% to 1%): Hypersensitivity, allergic reactions
- Postmarketing reports: Anaphylactic reaction, angioedema[Ref]
Allergic reactions have ranged from urticaria and mild skin eruptions to rare cases of anaphylaxis.
A 92-year-old female admitted for heart failure and a right upper lobe infiltrate was started on clarithromycin 500 mg. The following day, this drug was discontinued and IV antibiotics were initiated due to persisting fever. She received only 1 dose of this drug. On day 6 of the hospitalization, the patient was afebrile, IV antibiotics were stopped, and this drug was again started. Two hours after the dose, the patient developed swelling in her lips, jaw, tongue, mouth, and face. The patient was given diphenhydramine and the clarithromycin was discontinued. She was discharged the following day.[Ref]
Cardiovascular
- Common (1% to 10%): Vasodilation, phlebitis
- Uncommon (0.1% to 1%): ECG QT prolonged, cardiac arrest, atrial fibrillation, extrasystoles, palpitations
- Rare (0.01% to 0.1%): Arrhythmia
- Frequency not reported: QT interval prolongation
- Postmarketing reports: Ventricular arrhythmia, ventricular tachycardia, torsades de pointes, hemorrhage[Ref]
Hematologic
- Common (1% to 10%): Decreased WBC, decreased platelet count, decreased hemoglobin
- Uncommon (0.1% to 1%): Leukopenia, neutropenia, thrombocythemia, eosinophilia, increased prothrombin time
- Frequency not reported: Granulocytopenia, reduction in prothrombin time
- Postmarketing reports: Thrombocytopenia, agranulocytosis, prolonged prothrombin time, decreased WBC count, increased INR[Ref]
Decreased WBC (less than 1 x 10[9]/L), platelet count (less than 50 x 10[9]/L), and hemoglobin (less than 8 g/dL) were reported in up to 4%, up to 4%, and 3% of patients, respectively.[Ref]
Dermatologic
- Common (1% to 10%): Rash, hyperhidrosis, pruritus
- Uncommon (0.1% to 1%): Urticaria, dermatitis bullous, maculopapular rash, cellulitis, pustular rash (non-urticarial), stained fingernails
- Postmarketing reports: Stevens-Johnson syndrome, toxic epidermal necrolysis, drug rash with eosinophilia and systemic symptoms (DRESS), Henoch-Schonlein purpura, acne, erysipelas, erythrasma[Ref]
Other
- Common (1% to 10%): Infection, candidiasis, pyrexia/fever, asthenia
- Uncommon (0.1% to 1%): Malaise, chest pain, chills, fatigue, thirst, abnormal albumin globulin ratio, body aches and pains, flushing, accidental injury, flu syndrome
- Postmarketing reports: Otitis media, extended-release tablets in the stool, colchicine toxicity[Ref]
Many reports of extended-release tablets in the stool occurred in patients with anatomic (including ileostomy or colostomy) or functional gastrointestinal disorders with shortened gastrointestinal transit times. In several reports, tablet residues occurred in the context of diarrhea.
Colchicine toxicity has been reported with concomitant use of this drug and colchicine, especially in the elderly; some occurred in patients with renal dysfunction. Death occurred in some such patients.[Ref]
Psychiatric
- Common (1% to 10%): Insomnia
- Uncommon (0.1% to 1%): Anxiety, nervousness, screaming, depression, sleep disturbance
- Frequency not reported: Behavioral changes, nightmares, psychosis
- Postmarketing reports: Psychotic disorder, confusional state, depersonalization, disorientation, hallucination, depression, manic behavior, abnormal behavior, abnormal dreams[Ref]
The incidence of insomnia was similar for patients treated with 1 to 2 g/day, but was generally about 3 to 4 times as frequent for those treated with 4 g/day.
Psychotic disorder, confusional state, depersonalization, depression, disorientation, manic behavior, hallucination, abnormal behavior, and/or abnormal dreams usually resolved after the drug was stopped.[Ref]
Metabolic
- Common (1% to 10%): Increased alkaline phosphatase
- Uncommon (0.1% to 1%): Anorexia, decreased appetite, increased blood LDH
- Postmarketing reports: Hypoglycemia[Ref]
Increased alkaline phosphatase (greater than 5 x ULN) was reported in up to 2% of patients.
Hypoglycemia has been reported in patients receiving oral hypoglycemic agents or insulin.[Ref]
Respiratory
- Common (1% to 10%): Dyspnea, rhinitis, increased cough, pharyngitis, asthma
- Uncommon (0.1% to 1%): Epistaxis, pulmonary embolism
- Frequency not reported: Laryngismus[Ref]
The incidence of dyspnea was similar for patients treated with 1 to 2 g/day, but was generally about 3 to 4 times as frequent for those treated with 4 g/day.[Ref]
Ocular
- Common (1% to 10%): Conjunctivitis
- Uncommon (0.1% to 1%): Photophobia
- Very rare (less than 0.01%): Uveitis
- Frequency not reported: Corneal opacities[Ref]
Uveitis was reported primarily in patients treated with concomitant rifabutin; most cases were reversible.
A case of corneal opacities was reported in a patient with AIDS and Mycobacterium avium complex bacteremia. The patient's ocular signs and symptoms resolved upon substitution with azithromycin.[Ref]
Renal
- Uncommon (0.1% to 1%): Elevated BUN, elevated serum creatinine, increased blood urea, increased blood creatinine
- Frequency not reported: Acute renal failure
- Postmarketing reports: Interstitial nephritis, renal failure[Ref]
Elevated BUN (greater than 50 mg/dL) was reported in less than 1% of patients.[Ref]
Musculoskeletal
- Uncommon (0.1% to 1%): Myalgia, muscle spasms, nuchal rigidity, musculoskeletal stiffness, arthralgia, back pain
- Postmarketing reports: Myopathy, rhabdomyolysis
In some cases of rhabdomyolysis, this drug was coadministered with statins, fibrates, colchicine, or allopurinol.
Genitourinary
- Uncommon (0.1% to 1%): Vaginal infection
- Postmarketing reports: Abnormal urine color (associated with hepatic failure), dysuria[Ref]
Immunologic
- Rare (0.01% to 0.1%): Leukocytoclastic vasculitis[Ref]
References
1. "Multum Information Services, Inc. Expert Review Panel"
2. Cerner Multum, Inc. "UK Summary of Product Characteristics."
3. Cerner Multum, Inc. "Australian Product Information."
4. Straneo G, Scarpazza G (1990) "Efficacy and safety of clarithromycin versus josamycin in the treatment of hospitalized patients with bacterial pneumonia." J Int Med Res, 18, p. 164-70
5. Wood M (1991) "The tolerance and toxicity of clarithromycin." J Hosp Infect, 19, p. 39-46
6. Anderson G, Esmonde T, Coles S, et al. (1991) "A comparative safety and efficacy study of clarithromycin and erythromycin stearate in community-acquired pneumonia." J Antimicrob Chemother, 27, p. 117-24
7. Karma P, Pukander J, Penttila M, et al. (1991) "The comparative efficacy and safety of clarithromycin and amoxycillin in the treatment of outpatients with acute maxillary sinusitis." J Antimicrob Chemother, 27, p. 83-90
8. Hamedani P, Ali J, Hafeez S, et al. (1991) "The safety and efficacy of clarithromycin in patients with legionella pneumonia." Chest, 100, p. 1503-6
9. Peters D, Clissold S (1992) "Clarithromycin: a review of its antimicrobial activity, pharmacokinetic properties and therapeutic potential." Drugs, 44, p. 117-64
10. Guay D, Craft J (1992) "Comparative safety and efficacy of clarithromycin and ampicillin in the treatment of out-patients with acute bacterial exacerbation of chronic bronchitis." J Intern Med, 231, p. 295-301
11. Hardy D, Guay D, Jones R (1992) "Clarithromycin, a unique macrolide." Diagn Microbiol Infect Dis, 15, p. 39-53
12. Dorrell L, Ellerton C, Cottrell DG, Snow MH (1994) "Toxicity of clarithromycin in the treatment of mycobacterium avium complex infection in a patient with AIDS." J Antimicrob Chemother, 34, p. 605-6
13. Dautzenberg B, Piperno D, Diot P, Truffotpernot C, Chauvin JP (1995) "Clarithromycin in the treatment of mycobacterium avium lung infections in patients without AIDS." Chest, 107, p. 1035-40
14. Fong IW, Laforge J, Dubois J, Small D, Grossman R, Zakhari R, Thomas PT, Hoffstein V, Bourbeau J, Macdonald GF, Mclellan PA, (1995) "Clarithromycin versus cefaclor in lower respiratory tract infections." Clin Invest Med, 18, p. 131-8
15. (2001) "Product Information. Biaxin (clarithromycin)." Abbott Pharmaceutical
16. Nightingale SD, Koster FT, Mertz GJ, Loss SD (1995) "Clarithromycin-induced mania in two patients with AIDS." Clin Infect Dis, 20, p. 1563-4
17. Zuckerman JM, Kaye KM (1995) "The newer macrolides: azithromycin and clarithromycin." Infect Dis Clin North Am, 9, p. 731-45
18. Pijpers E, Vanrijswijk REN, Takxkohlen B, Schrey G (1996) "A clarithromycin-induced myasthenic syndrome." Clin Infect Dis, 22, p. 175-6
19. Macfarlane JT, Prewitt J, Gard P, Guion A (1996) "Comparison of amoxycillin and clarithromycin as initial treatment of community-acquired lower respiratory tract infections." Br J Gen Pract, 46, p. 357-60
20. Fraschini F (1990) "Clinical efficacy and tolerance of two new macrolides, clarithromycin and josamycin, in the treatment of patients with acute exacerbations of chronic bronchitis." J Int Med Res, 18, p. 171-76
21. Marchi E (1990) "Comparative efficacy and tolerability of clarithromycin and amoxycillin in the treatment of out-patients with acute maxillary sinusitis." Curr Med Res Opin, 12, p. 19-24
22. de Campora E, Camaioni A, Leonardi M, et al. (1992) "Comparative efficacy and safety of roxithromycin and clarithromycin in upper respiratory tract infections." Diagn Microbiol Infect Dis, 15, s119-22
23. Liviu L, Yair L, Yehuda S (1996) "Pancreatitis induced by clarithromycin." Ann Intern Med, 125, p. 701
24. Brown BA, Wallace RJ, Griffith DE, Girard W (1995) "Clarithromycin-induced hepatotoxicity." Clin Infect Dis, 20, p. 1073-4
25. Shaheen N, Grimm IS (1996) "Fulminant hepatic failure associated with clarithromycin." Am J Gastroenterol, 91, p. 394-5
26. Liviu L, Yair L (1996) "Pancreatitis induced by clarithromycin." Ann Intern Med, 125, p. 701
27. Baylor P, Williams K (1999) "Interstitial nephritis, thrombocytopenia, hepatitis, and elevated serum amylase levels in a patient receiving clarithromycin therapy." Clin Infect Dis, 29, p. 1350-1
28. Vangala R, Cernek PK (1996) "Hypersensitivity reaction to clarithromycin." Ann Pharmacother, 30, p. 300
29. Kundu S, Williams SR, Nordt SP, Clark RF (1997) "Clarithromycin-induced ventricular tachycardia." Ann Emerg Med, 30, p. 542-4
30. Lee KL, Jim MH, Tang SC, Tai YT (1998) "QT prolongation and Torsades de pointes associated with clarithromycin." Am J Med, 104, p. 395-6
31. Cone LA, Sneider RA, Nazemi R, Dietrich EJ (1996) "Mania due to clarithromycin therapy in a patient who was not infected with human immunodeficiency virus." Clin Infect Dis, 22, p. 595-6
32. Abouesh A, Hobbs WR (1998) "Clarithromycin-induced mania." Am J Psychiatry, 155, p. 1626
33. Mermelstein HT (1998) "Clarithromycin-induced delirium in a general hospital." Psychosomatics, 39, p. 540-2
34. GomezGil E, Garcia F, Pintor L, Martinez JA, Mensa J, dePablo J (1999) "Clarithromycin-induced acute psychoses in peptic ulcer disease." Eur J Clin Microbiol Infect D, 18, p. 70-1
35. Geiderman JM (1999) "Central nervous system disturbances following clarithromycin ingestion." Clin Infect Dis, 29, p. 464-5
36. (1998) "WHO system finds 13 drugs with AEs not in PDR, Martindale." F-D-C Reports -- "The Pink Sheet", 60, p. 16
37. Gavura SR, Nusinowitz S (1998) "Leukocytoclastic vasculitis associated with clarithromycin." Ann Pharmacother, 32, p. 543-5
Frequently asked questions
- Is Biaxin good for a tooth infection or abscess?
- Can you take Biaxin if you’re allergic to penicillin?
- Is Biaxin a sulfa-based drug?
- Can Biaxin cause yeast infections?
- Can Biaxin cause headaches?
- How long does it take for Biaxin to work?
- What is the Best Antibiotic for Strep Throat?
- What are the best antibiotics for pneumonia?
- Do statins cause rhabdomyolysis, and how is it treated?
More about Biaxin (clarithromycin)
- Check interactions
- Compare alternatives
- Reviews (91)
- Drug images
- Dosage information
- During pregnancy
- Drug class: macrolides
- Breastfeeding
Patient resources
Other brands
Professional resources
Related treatment guides
Further information
Biaxin side effects can vary depending on the individual. Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
Note: Medication side effects may be underreported. If you are experiencing side effects that are not listed, submit a report to the FDA by following this guide.