Oxaprozin (Monograph)
Brand name: Daypro
Drug class: Reversible COX-1/COX-2 Inhibitors
Warning
- Cardiovascular Risk
-
Increased risk of serious (sometimes fatal) cardiovascular thrombotic events (e.g., MI, stroke). Risk may occur early in treatment and may increase with duration of use. (See Cardiovascular Thrombotic Effects under Cautions.)
-
Contraindicated in the setting of CABG surgery.
- GI Risk
-
Increased risk of serious (sometimes fatal) GI events (e.g., bleeding, ulceration, perforation of the stomach or intestine). Serious GI events can occur at any time and may not be preceded by warning signs and symptoms. Geriatric individuals are at greater risk for serious GI events. (See GI Effects under Cautions.)
Introduction
Prototypical NSAIA; propionic acid derivative.
Uses for Oxaprozin
Consider potential benefits and risks of oxaprozin therapy as well as alternative therapies before initiating therapy with the drug. Use lowest effective dosage and shortest duration of therapy consistent with the patient’s treatment goals.
Inflammatory Diseases
Symptomatic treatment of osteoarthritis and rheumatoid arthritis.
Management of juvenile rheumatoid arthritis in children 6-16 years of age.
Oxaprozin Dosage and Administration
General
-
Consider potential benefits and risks of oxaprozin therapy as well as alternative therapies before initiating therapy with the drug.
Administration
Oral Administration
Administer orally once daily; divided doses may improve tolerance in some patients.
Dosage
To minimize the potential risk of adverse cardiovascular and/or GI events, use lowest effective dosage and shortest duration of therapy consistent with the patient’s treatment goals. Adjust dosage based on individual requirements and response; attempt to titrate to lowest effective dosage.
Pediatric Patients
Inflammatory Disease
Juvenile Rheumatoid Arthritis
Oral|
Weight (kg) |
Dosage |
|---|---|
|
22–31 |
600 mg once daily |
|
32–54 |
900 mg once daily |
|
≥55 |
1.2 g once daily |
Adults
Inflammatory Diseases
Osteoarthritis or Rheumatoid Arthritis
OralInitially, 1.2 g once daily. Reserve long-term use of dosages >1.2 g daily for adults with severe disease who weigh >50 kg, have normal renal and hepatic function, and low risk for GI toxicity.
If rapid onset of action needed, administer one-time loading dose of 1.2–1.8 g (up to 26 mg/kg).
Patients with low body weight: Initially, 600 mg once daily. May increase to 1.2 g daily if needed.
Prescribing Limits
Pediatric Patients
Juvenile Rheumatoid Arthritis
Oral
Doses >1.2 g daily not studied.
Adults
Inflammatory Diseases
Osteoarthritis or Rheumatoid Arthritis
OralMaximum 1.8 g or 26 mg/kg daily (whichever is lower). Maximum loading dose is 26 mg/kg.
Special Populations
Renal Impairment
Severe renal impairment and in those undergoing hemodialysis: Initially, 600 mg once daily. May increase to 1.2 g daily if needed. Supplemental doses after hemodialysis not needed.
Hepatic Impairment
Dosage adjustment not needed in patients with well-compensated cirrhosis.
Geriatric Patients
Dosage adjustment may be necessary in patients with low body weight, decreased renal function, or age-related concomitant disease.
Cautions for Oxaprozin
Contraindications
-
Known hypersensitivity to oxaprozin or any ingredient in the formulation.
-
History of asthma, urticaria, or other sensitivity reaction precipitated by aspirin or other NSAIAs.
-
In the setting of CABG surgery.
Warnings/Precautions
Warnings
Cardiovascular Thrombotic Effects
NSAIAs (selective COX-2 inhibitors, prototypical NSAIAs) increase the risk of serious adverse cardiovascular thrombotic events (e.g., MI, stroke) in patients with or without cardiovascular disease or risk factors for cardiovascular disease.
Findings of FDA review of observational studies, meta-analysis of randomized controlled trials, and other published information indicate that NSAIAs may increase the risk of such events by 10–50% or more, depending on the drugs and dosages studied.
Relative increase in risk appears to be similar in patients with or without known underlying cardiovascular disease or risk factors for cardiovascular disease, but the absolute incidence of serious NSAIA-associated cardiovascular thrombotic events is higher in those with cardiovascular disease or risk factors for cardiovascular disease because of their elevated baseline risk.
Increased risk may occur early (within the first weeks) following initiation of therapy and may increase with higher dosages and longer durations of use.
In controlled studies, increased risk of MI and stroke observed in patients receiving a selective COX-2 inhibitor for analgesia in first 10–14 days following CABG surgery.
In patients receiving NSAIAs following MI, increased risk of reinfarction and death observed beginning in the first week of treatment.
Increased 1-year mortality rate observed in patients receiving NSAIAs following MI; absolute mortality rate declined somewhat after the first post-MI year, but the increased relative risk of death persisted over at least the next 4 years.
Some systematic reviews of controlled observational studies and meta-analyses of randomized studies suggest naproxen may be associated with lower risk of cardiovascular thrombotic events compared with other NSAIAs. FDA states that limitations of these studies and indirect comparisons preclude definitive conclusions regarding relative risks of NSAIAs.
Use NSAIAs with caution and careful monitoring (e.g., monitor for development of cardiovascular events throughout therapy, even in those without prior cardiovascular symptoms) and at the lowest effective dosage for the shortest duration necessary.
Some clinicians suggest that it may be prudent to avoid NSAIA use, whenever possible, in patients with cardiovascular disease. Avoid use in patients with recent MI unless benefits of therapy are expected to outweigh risk of recurrent cardiovascular thrombotic events; if used, monitor for cardiac ischemia. Contraindicated in the setting of CABG surgery.
No consistent evidence that concomitant use of low-dose aspirin mitigates the increased risk of serious adverse cardiovascular events. (See Specific Drugs under Interactions.)
GI Effects
Serious GI toxicity (e.g., bleeding, ulceration, perforation) can occur with or without warning symptoms; increased risk in those with a history of GI bleeding or ulceration, geriatric patients, smokers, those with alcohol dependence, and those in poor general health.
For patients at high risk for complications from NSAIA-induced GI ulceration (e.g., bleeding, perforation), consider concomitant use of misoprostol; alternatively, consider concomitant use of proton pump inhibitor (e.g., omeprazole) or use of an NSAIA that is a selective inhibitor of COX-2 (e.g., celecoxib).
Hypertension
Hypertension and worsening of preexisting hypertension reported; either event may contribute to the increased incidence of cardiovascular events. Use with caution in patients with hypertension; monitor BP.
Impaired response to ACE inhibitors, angiotensin II receptor antagonists, β-blockers, and certain diuretics may occur. (See Specific Drugs under Interactions.)
Heart Failure and Edema
Fluid retention and edema reported.
NSAIAs (selective COX-2 inhibitors, prototypical NSAIAs) may increase morbidity and mortality in patients with heart failure.
NSAIAs may diminish cardiovascular effects of diuretics, ACE inhibitors, or angiotensin II receptor antagonists used to treat heart failure or edema. (See Specific Drugs under Interactions.)
Manufacturer recommends avoiding use in patients with severe heart failure unless benefits of therapy are expected to outweigh risk of worsening heart failure; if used, monitor for worsening heart failure.
Some experts recommend avoiding use, whenever possible, in patients with reduced left ventricular ejection fraction and current or prior symptoms of heart failure.
Renal Effects
Direct renal injury, including renal papillary necrosis, reported in patients receiving long-term NSAIA therapy.
Potential for overt renal decompensation. Increased risk of renal toxicity in patients with renal or hepatic impairment or heart failure, in geriatric patients, in patients with volume depletion, and in those receiving a diuretic, ACE inhibitor, or angiotensin II receptor antagonist.
Sensitivity Reactions
Hypersensitivity
Anaphylactoid reactions (e.g., anaphylaxis, angioedema) reported. Immediate medical intervention and discontinuance for anaphylaxis.
Avoid in patients with aspirin triad (aspirin sensitivity, asthma, nasal polyps); caution in patients with asthma.
Potentially fatal or life-threatening syndrome of multi-organ hypersensitivity (i.e., drug reaction with eosinophilia and systemic symptoms [DRESS]) reported in patients receiving NSAIAs. Clinical presentation is variable, but typically includes eosinophilia, fever, rash, lymphadenopathy, and/or facial swelling, possibly associated with other organ system involvement (e.g., hepatitis, nephritis, hematologic abnormalities, myocarditis, myositis). Symptoms may resemble those of acute viral infection. Early manifestations of hypersensitivity (e.g., fever, lymphadenopathy) may be present in the absence of rash. If signs or symptoms of DRESS develop, discontinue the NSAIA and immediately evaluate the patient.
Dermatologic Reactions
Serious skin reactions (e.g., exfoliative dermatitis, Stevens-Johnson syndrome, toxic epidermal necrolysis) reported; can occur without warning. Discontinue at first appearance of rash or any other signs of hypersensitivity (e.g., blisters, fever, pruritus).
Photosensitivity
Rash on sun-exposed areas of the body reported.
General Precautions
Hepatic Effects
Severe reactions including jaundice, fatal fulminant hepatitis, liver necrosis, and hepatic failure (sometimes fatal) reported rarely with NSAIAs.
Elevations of serum ALT or AST reported.
Monitor for symptoms and/or signs suggesting liver dysfunction; monitor abnormal liver function test results. Discontinue if signs or symptoms of liver disease or systemic manifestation (e.g., eosinophilia, rash) occur or if liver function test abnormalities persist or worsen.
Hematologic Effects
Anemia reported rarely. Determine hemoglobin concentration or hematocrit in patients receiving long-term therapy if signs or symptoms of anemia occur.
May inhibit platelet aggregation and prolong bleeding time.
Other Precautions
Not a substitute for corticosteroid therapy; not effective in the management of adrenal insufficiency.
May mask certain signs of infection.
Obtain CBC and chemistry profile periodically during long-term use.
Specific Populations
Pregnancy
Use of NSAIAs during pregnancy at about ≥30 weeks’ gestation can cause premature closure of the fetal ductus arteriosus; use at about ≥20 weeks’ gestation associated with fetal renal dysfunction resulting in oligohydramnios and, in some cases, neonatal renal impairment.
Effects of NSAIAs on the human fetus during third trimester of pregnancy include prenatal constriction of the ductus arteriosus, tricuspid incompetence, and pulmonary hypertension; nonclosure of the ductus arteriosus during the postnatal period (which may be resistant to medical management); and myocardial degenerative changes, platelet dysfunction with resultant bleeding, intracranial bleeding, renal dysfunction or renal failure, renal injury or dysgenesis potentially resulting in prolonged or permanent renal failure, oligohydramnios, GI bleeding or perforation, and increased risk of necrotizing enterocolitis.
Avoid use of NSAIAs in pregnant women at about ≥30 weeks’ gestation; if use required between about 20 and 30 weeks’ gestation, use lowest effective dosage and shortest possible duration of treatment, and consider monitoring amniotic fluid volume via ultrasound examination if treatment duration >48 hours; if oligohydramnios occurs, discontinue drug and follow up according to clinical practice. (See Advice to Patients.)
Fetal renal dysfunction resulting in oligohydramnios and, in some cases, neonatal renal impairment observed, on average, following days to weeks of maternal NSAIA use; infrequently, oligohydramnios observed as early as 48 hours after initiation of NSAIAs. Oligohydramnios is often, but not always, reversible (generally within 3–6 days) following NSAIA discontinuance. Complications of prolonged oligohydramnios may include limb contracture and delayed lung maturation. In limited number of cases, neonatal renal dysfunction (sometimes irreversible) occurred without oligohydramnios. Some neonates have required invasive procedures (e.g., exchange transfusion, dialysis). Deaths associated with neonatal renal failure also reported. Limitations of available data (lack of control group; limited information regarding dosage, duration, and timing of drug exposure; concomitant use of other drugs) preclude a reliable estimate of the risk of adverse fetal and neonatal outcomes with maternal NSAIA use. Available data on neonatal outcomes generally involved preterm infants; extent to which risks can be generalized to full-term infants is uncertain.
Animal data indicate important roles for prostaglandins in kidney development and endometrial vascular permeability, blastocyst implantation, and decidualization. In animal studies, inhibitors of prostaglandin synthesis increased pre- and post-implantation losses; also impaired kidney development at clinically relevant doses.
No adequate and well-controlled studies of oxaprozin in pregnant women. In animal studies, teratogenicity observed in rabbits, but no evidence of teratogenicity or embryotoxicity observed in mice or rats. Failure to deliver and a reduction in live birth index observed in rats.
Effects of oxaprozin on labor and delivery not known. In animal studies, NSAIAs delayed parturition and increased stillbirths.
Lactation
Distributed into milk in rats; not known whether distributed into human milk. Discontinue nursing or the drug.
Fertility
NSAIAs may be associated with reversible infertility in some women. Reversible delays in ovulation observed in limited studies in women receiving NSAIAs; animal studies indicate that inhibitors of prostaglandin synthesis can disrupt prostaglandin-mediated follicular rupture required for ovulation.
Consider withdrawal of NSAIAs in women experiencing difficulty conceiving or undergoing evaluation of infertility.
Testicular degeneration with oxaprozin administration observed in dogs, but not confirmed in other species; clinical relevance not known.
Pediatric Use
Safety and efficacy not established in children <6 years of age.
Safety and efficacy in pediatric patients 6–16 years of age with juvenile rheumatoid arthritis supported by studies in adults with rheumatoid arthritis and by safety and pharmacokinetic data from trials in children with juvenile rheumatoid arthritis.
Geriatric Use
No overall differences in efficacy or safety were observed between geriatric and younger adults. Possibility exists of greater sensitivity in some geriatric individuals.
Caution advised. Geriatric adults appear to tolerate NSAIA-induced adverse effects less well than younger individuals.
Select dosage with caution because of age-related decreases in renal function. May be useful to monitor renal function.
Hepatic Impairment
Use with caution in patients with severe hepatic impairment.
Renal Impairment
Use not recommended in patients with advanced renal disease; close monitoring of renal function advised if used. Dosage adjustment needed. (See Renal Impairment under Dosage and Administration.)
Common Adverse Effects
Abdominal pain, anorexia, constipation, diarrhea, flatulence, GI ulcers, GI bleeding/perforation, dyspepsia, heartburn, nausea, vomiting, renal function abnormalities, anemia, confusion, depression, sleep disturbance, dizziness, dysuria or increased frequency, edema, liver function test abnormalities, headache, prolonged bleeding time, pruritus, rash, sedation, somnolence, tinnitus.
Drug Interactions
Specific Drugs
|
Drug |
Interaction |
Comments |
|---|---|---|
|
ACE inhibitors |
Reduced BP response to ACE inhibitor |
Monitor BP |
|
Acetaminophen |
Pharmacokinetic interaction unlikely |
|
|
Angiotensin II receptor antagonists |
Reduced BP response to angiotensin II receptor antagonist |
Monitor BP |
|
Antacids |
Change in oxaprozin bioavailability unlikely |
|
|
Aspirin |
Increased risk of GI ulceration and other complications No consistent evidence that low-dose aspirin mitigates the increased risk of serious cardiovascular events associated with NSAIAs Possible pharmacokinetic interaction (altered plasma protein binding) |
Manufacturer states that concomitant use not recommended |
|
β-Adrenergic blocking agents |
Reduced BP response to metoprolol reported |
Monitor BP |
|
Diuretics (furosemide, thiazides) |
Reduced natriuretic effects possible |
Monitor for diuretic efficacy and renal failure |
|
Estrogens, conjugated |
Pharmacokinetic interaction unlikely |
|
|
Glyburide |
Pharmacokinetic interaction; no effect on hypoglycemic effects |
Monitor blood glucose if concomitant therapy initiated |
|
Histamine H2-receptor antagonists (cimetidine, ranitidine) |
Decreased clearance of oxaprozin |
|
|
Lithium |
Increased plasma lithium concentrations |
Monitor for lithium toxicity |
|
Methotrexate |
Possible toxicity associated with increased plasma methotrexate concentration |
Caution advised |
|
Pemetrexed |
Possible increased risk of pemetrexed-associated myelosuppression, renal toxicity, and GI toxicity |
Short half-life NSAIAs (e. g., diclofenac, indomethacin): Avoid administration beginning 2 days before and continuing through 2 days after pemetrexed administration Longer half-life NSAIAs (e.g., meloxicam, nabumetone): In the absence of data, avoid administration beginning at least 5 days before and continuing through 2 days after pemetrexed administration Patients with Clcr 45–79 mL/minute: Monitor for myelosuppression, renal toxicity, and GI toxicity |
|
Warfarin |
Possibility of bleeding complications |
Caution advised |
Oxaprozin Pharmacokinetics
Absorption
Bioavailability
Well absorbed following oral administration.
Food
Food may reduce the rate of absorption, but does not affect extent of absorption.
Distribution
Extent
Distributed into synovial tissues in patients with rheumatoid arthritis.
Plasma Protein Binding
99% (mainly albumin).
Elimination
Metabolism
Metabolized, principally in the liver, to inactive metabolites.
Elimination Route
Excreted in urine (65%) and in feces (35%) as metabolites; approximately 5% is excreted in urine as unchanged drug.
Half-life
Approximately 38–44 hours.
Special Populations
Renal clearance decreased in patients with renal impairment; renal clearance contributes minimally to excretion of oxaprozin. Not removed by hemodialysis or continuous ambulatory peritoneal dialysis (CAPD).
Stability
Storage
Oral
Tablets
Tight, light resistant containers at 25°C (may be exposed to 15–30°C).
Actions
-
Inhibits cyclooxygenase-1 (COX-1) and COX-2.
-
Pharmacologic actions similar to those of other prototypical NSAIAs; exhibits anti-inflammatory, analgesic, and antipyretic activity.
Advice to Patients
-
Importance of reading the medication guide for NSAIAs that is provided each time the drug is dispensed.
-
Risk of serious cardiovascular events (e.g., MI, stroke).
-
Risk of GI toxicity and ulceration.
-
Risk of serious skin reactions, DRESS, and anaphylactoid and other sensitivity reactions.
-
Risk of hepatotoxicity.
-
Importance of seeking immediate medical attention if signs and symptoms of a cardiovascular event (chest pain, dyspnea, weakness, slurred speech) occur.
-
Importance of notifying clinician if signs and symptoms of GI ulceration or bleeding, unexplained weight gain, or edema develops.
-
Advise patients to stop taking the drug immediately if they develop any type of rash or fever and to promptly contact their clinician. Importance of seeking immediate medical attention if an anaphylactic reaction occurs.
-
Importance of discontinuing therapy and contacting clinician immediately if signs and symptoms of hepatotoxicity (nausea, fatigue, lethargy, pruritus, jaundice, upper right quadrant tenderness, flu-like symptoms) occur.
-
Risk of heart failure or edema; importance of reporting dyspnea, unexplained weight gain, or edema.
-
Importance of women informing clinicians if they are or plan to become pregnant or plan to breast-feed.
-
Importance of avoiding NSAIA use beginning at 20 weeks’ gestation unless otherwise advised by a clinician; importance of avoiding NSAIAs beginning at 30 weeks’ gestation because of risk of premature closure of the fetal ductus arteriosus; monitoring for oligohydramnios may be necessary if NSAIA therapy required for >48 hours’ duration between about 20 and 30 weeks’ gestation.
-
Advise women who are trying to conceive that NSAIAs may be associated with a reversible delay in ovulation.
-
Importance of informing clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs, as well as any concomitant diseases.
-
Importance of informing patients of other important precautionary information. (See Cautions.)
Additional Information
The American Society of Health-System Pharmacists, Inc. represents that the information provided in the accompanying monograph was formulated with a reasonable standard of care, and in conformity with professional standards in the field. Readers are advised that decisions regarding use of drugs are complex medical decisions requiring the independent, informed decision of an appropriate health care professional, and that the information contained in the monograph is provided for informational purposes only. The manufacturer’s labeling should be consulted for more detailed information. The American Society of Health-System Pharmacists, Inc. does not endorse or recommend the use of any drug. The information contained in the monograph is not a substitute for medical care.
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
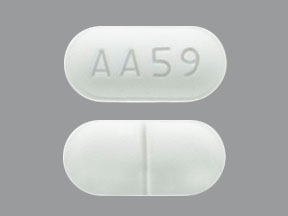
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Tablets, film-coated |
600 mg* |
Daypro (scored) |
Searle |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions June 10, 2024. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
Reload page with references included
Related/similar drugs
More about oxaprozin
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (8)
- Drug images
- Latest FDA alerts (4)
- Side effects
- Dosage information
- During pregnancy
- Drug class: Nonsteroidal anti-inflammatory drugs
- Breastfeeding