Amlodipine / Valsartan Dosage
Medically reviewed by Drugs.com. Last updated on May 26, 2025.
Applies to the following strengths: 5 mg-160 mg; 10 mg-160 mg; 5 mg-320 mg; 10 mg-320 mg
Usual Adult Dose for:
Additional dosage information:
Usual Adult Dose for Hypertension
Initial therapy: Amlodipine 5 mg-Valsartan 160 mg orally once a day
Add-on/Replacement therapy: Amlodipine 5 to 10 mg-Valsartan 160 to 320 mg orally once a day
Comments:
- May increase dose after 1 to 2 weeks of therapy.
- A patient who experiences dose-limiting adverse reactions on either component alone may be switched to this drug containing a lower dose of that component in combination with the other. If blood pressure remains uncontrolled after 3 to 4 weeks, may titrate up to a maximum of amlodipine 10 mg-valsartan 320 mg orally once a day.
Renal Dose Adjustments
Mild to moderate renal dysfunction (CrCl 30 to 90 mL/min): No adjustment recommended
Severe renal dysfunction (CrCl less than 30 mL/min): Data not available
Liver Dose Adjustments
Initial therapy not recommended
Precautions
US BOXED WARNING:
- FETAL TOXICITY: If pregnancy is detected, discontinue this drug as soon as possible. Drugs that act directly on the renin-angiotensin system (RAS) can cause injury and death to the developing fetus.
Safety and efficacy have not been established in patients younger than 18 years.
Consult WARNINGS section for additional precautions.
Dialysis
Data not available
Other Comments
Monitoring: Monitor renal function and serum electrolytes periodically.
Patient advice:
- Advise patients to immediately report any signs or symptoms of angioedema (breathing difficulty or swelling of face, eyes, lips, or tongue) and to stop taking this drug until consulting a physician.
- Advise patients that lightheadedness can occur, especially during the first days of treatment, and that it should be reported to their healthcare provider.
- Advise patients to discontinue this drug until a physician has been consulted if syncope occurs.
- Inform patients that inadequate fluid intake, excessive perspiration, diarrhea, or vomiting can lead to an excessive fall in blood pressure.
- Advise patients not to use salt substitutes without first consulting their healthcare provider.
- Females of childbearing age should be informed of the consequences of exposure to this drug during pregnancy; ask these patients to report pregnancies as soon as possible.
- Advice women not to breastfeed during treatment with this drug.
More about amlodipine / valsartan
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (60)
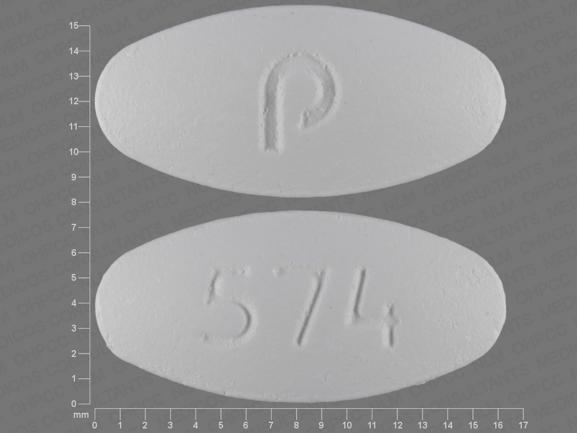
- Drug images
- Side effects
- During pregnancy
- Drug class: angiotensin II inhibitors with calcium channel blockers
- En español
Patient resources
Other brands
Professional resources
Other brands
Related treatment guides
See also:
Lasix
Lasix is a loop diuretic used to treat fluid retention from heart, liver, or kidney conditions, and ...
Enalapril
Enalapril is used to treat high blood pressure, congestive heart failure and to improve survival ...
Botox
Botox is used cosmetically to reduce facial lines and wrinkles and for medical purposes for ...
Valsartan
Valsartan is an angiotensin II receptor blocker (ARB) that may be used to treat high blood pressure ...
Hydrochlorothiazide
HCTZ (hydrochlorothiazide) used to treat high blood pressure (hypertension) and edema. Includes ...
Atenolol
Atenolol is used to treat angina (chest pain) and hypertension (high blood pressure). Learn about ...
Furosemide
Furosemide is a loop diuretic used to treat fluid retention and high blood pressure by increasing ...
Metoprolol
Metoprolol is used to treat angina (chest pain) and hypertension (high blood pressure). Learn about ...
Losartan
Losartan is used to treat high blood pressure (hypertension). It is also used to lower the risk of ...
Lisinopril
Lisinopril is an ACE inhibitor. It is used to treat high blood pressure, congestive heart failure ...
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.