Mebendazole (Monograph)
Brand names: Emverm, Vermox
Drug class: Anthelmintics
VA class: AP200
CAS number: 31431-39-7
Introduction
Anthelmintic agent; benzimidazole derivative.
Uses for Mebendazole
Ascariasis
Treatment of ascariasis caused by Ascaris lumbricoides (roundworm). Albendazole, mebendazole and ivermectin are drugs of choice.
Enterobiasis
Treatment of enterobiasis caused by Enterobius vermicularis (pinworm). Albendazole, mebendazole, and pyrantel pamoate are drugs of choice.
Hookworm Infections
Treatment of intestinal hookworm infections caused by Ancylostoma duodenale or Necator americanus in single or mixed infections. Drugs of choice are albendazole, mebendazole, and pyrantel pamoate.
Treatment of eosinophilic enterocolitis† [off-label] caused by Ancylostoma caninum (dog hookworm). Treatment of choice is albendazole, mebendazole, or endoscopic removal of worms.
Trichuriasis
Treatment of trichuriasis caused by Trichuris trichiura (whipworm). Albendazole is drug of choice; mebendazole and ivermectin are alternatives.
Angiostrongyliasis
Has been used in conjunction with corticosteroids for treatment of eosinophilic meningitis caused by Angiostrongylus cantonensis† [off-label]. May shorten course of infection, but not number of relapses. Infection usually self-limited. No drug proven effective; some patients have worsened when treated.
Baylisascariasis
Possible alternative for treatment of baylisascariasis† [off-label] caused by Baylisascaris procyonis (raccoon roundworm).
Albendazole is drug of choice; some clinicians suggest that mebendazole, levamisole (not commercially available in US), and ivermectin may be alternatives if albendazole unavailable.
Capillariasis
Treatment of capillariasis† [off-label] caused by Capillaria philippinensis (Philippine threadworm). Mebendazole is drug of choice; albendazole is an alternative.
Toxocariasis (Visceral Larva Migrans)
Treatment of toxocariasis† [off-label] (visceral larva migrans) caused by Toxocara canis or T. cati (dog or cat roundworm). Albendazole and mebendazole are drugs of choice. Concomitant corticosteroids may be indicated in severe cases with cardiac, ocular, or CNS involvement. Antiparasitic treatment may not be effective for ocular larva migrans; inflammation may be reduced by corticosteroid injections; surgery may be necessary for secondary damage.
Trichinellosis
Treatment of trichinellosis† (trichinosis) caused by Trichinella spiralis (pork worm). Drug of choice is albendazole; mebendazole is an alternative. Concomitant corticosteroids usually recommended, especially for severe disease. Corticosteroids alleviate symptoms of the inflammatory reaction and can be lifesaving when cardiac or CNS systems are involved.
Trichostrongyliasis
Treatment of trichostrongyliasis† caused by Trichostrongylus. Pyrantel pamoate is drug of choice; albendazole and mebendazole are alternatives.
Mebendazole Dosage and Administration
Administration
Oral Administration
Administer orally without regard to meals.
Mebendazole 100-mg chewable tablets: May be chewed, swallowed whole, or crushed and mixed with food.
Mebendazole 500-mg chewable tablets: Must be chewed completely before swallowing and should not be swallowed whole. In individuals who have difficulty chewing, place tablet on a spoon and add 2–3 mL of drinking water onto the tablet using a dosing syringe. Within 2 minutes, tablet should absorb the water and change into a soft, semi-solid mass that can be swallowed.
Dosage
Pediatric Patients
Ascariasis (Roundworm)
Oral
Children ≥2 years of age (100-mg chewable tablets): 100 mg twice daily (morning and evening) for 3 consecutive days. Manufacturer recommends a second course of treatment if patient not cured 3 weeks after mebendazole treatment.
Children ≥1 year of age (500-mg chewable tablets): Single 500-mg dose.
Enterobiasis (Pinworm)
Oral
Children ≥2 years of age (100-mg chewable tablets): Single 100-mg dose. Some clinicians recommend a second 100-mg dose 2 weeks later. Manufacturer recommends a second course of treatment if patient not cured 3 weeks after mebendazole treatment.
Some clinicians state consider treating all household contacts, especially when multiple or repeated symptomatic infections are occurring in the household.
Hookworm Infections
Intestinal Hookworm Infections
OralChildren ≥2 years of age (100-mg chewable tablets): 100 mg twice daily (morning and evening) for 3 consecutive days. Manufacturer recommends a second course of treatment if patient not cured 3 weeks after mebendazole treatment.
Alternatively, single 500-mg dose has been recommended.
Eosinophilic Enterocolitis Caused by Ancylostoma caninum (Dog Hookworm)†
Oral100 mg twice daily for 3 consecutive days has been recommended.
Trichuriasis (Whipworm)
Oral
Children ≥2 years of age (100-mg chewable tablets): 100 mg twice daily (morning and evening) for 3 consecutive days. Manufacturer recommends a second course of treatment if patient not cured 3 weeks after mebendazole treatment.
Children ≥1 year of age (500-mg chewable tablets): Single 500-mg dose.
Capillariasis (Philippine Threadworm)†
Oral
200 mg twice daily for 20 days has been recommended.
Toxocariasis (Visceral Larva Migrans Caused by Dog or Cat Roundworm)†
Oral
100–200 mg twice daily for 5 days has been recommended. Optimum duration of treatment not known; some clinicians recommend up to 20 days of treatment. For severe symptoms or eye involvement, some clinicians state treatment may be extended to 2–4 weeks.
Trichinellosis (Pork Worm)†
Oral
200–400 mg 3 times daily for 3 days followed by 400–500 mg 3 times daily for 10 days has been recommended.
Trichostrongyliasis†
Oral
100 mg twice daily for 3 consecutive days has been recommended.
Adults
Ascariasis (Roundworm)
Oral
100-mg chewable tablets: 100 mg twice daily (morning and evening) for 3 consecutive days. Manufacturer recommends a second course of treatment if patient not cured 3 weeks after mebendazole treatment.
500-mg chewable tablets: Single 500-mg dose.
Enterobiasis (Pinworm)
Oral
100-mg chewable tablets: Single 100-mg dose. Some clinicians recommend a second 100-mg dose 2 weeks later. Manufacturer recommends a second course of treatment if patient not cured 3 weeks after mebendazole treatment.
Some clinicians state consider treating all household contacts, especially when multiple or repeated symptomatic infections are occurring in the household.
Hookworm Infections
Intestinal Hookworm Infections
Oral100-mg chewable tablets: 100 mg twice daily (morning and evening) for 3 consecutive days. Manufacturer recommends a second course of treatment if patient not cured 3 weeks after mebendazole treatment.
500-mg chewable tablets: Single 500-mg dose.
Eosinophilic Enterocolitis Caused by Ancylostoma caninum (Dog Hookworm)†
Oral100 mg twice daily for 3 consecutive days has been recommended.
Trichuriasis (Whipworm)
Oral
100-mg chewable tablets: 100 mg twice daily (morning and evening) for 3 consecutive days. Manufacturer recommends a second course of treatment if patient not cured 3 weeks after mebendazole treatment.
500-mg chewable tablets: Single 500-mg dose.
Capillariasis (Philippine Threadworm)†
Oral
200 mg twice daily for 20 days has been recommended.
Toxocariasis (Visceral Larva Migrans Caused by Dog or Cat Roundworm)†
Oral
100–200 mg twice daily for 5 days has been recommended. Optimum duration of treatment not known; some clinicians recommend up to 20 days of treatment. For severe symptoms or eye involvement, some clinicians state treatment may be extended to 2–4 weeks.
Trichinellosis (Pork Worm)†
Oral
200–400 mg 3 times daily for 3 days followed by 400–500 mg 3 times daily for 10 days has been recommended.
Trichostrongyliasis†
Oral
100 mg twice daily for 3 consecutive days has been recommended.
Special Populations
No special population dosage recommendations.
Cautions for Mebendazole
Contraindications
-
Hypersensitivity to the drug or any ingredient in the formulation.
Warnings/Precautions
Sensitivity Reactions
Hypersensitivity Reactions
Hypersensitivity reactions, including anaphylactic reactions, reported rarely.
Rash, pruritus, exanthema, urticaria, angioedema, toxic epidermal necrolysis, and Stevens-Johnson syndrome also reported rarely.
Hematologic Effects
Neutropenia (including agranulocytosis) and/or thrombocytopenia reported, especially in patients receiving higher dosages or more prolonged treatment than usually recommended. Myelosuppression usually reversible following discontinuance of the drug, but death has occurred rarely.
Decreased hemoglobin concentration and/or hematocrit, leukopenia, and eosinophilia also reported rarely.
Monitor blood counts if mebendazole given using higher dosage or more prolonged duration of treatment than usually recommended.
Specific Populations
Pregnancy
In rats, adverse developmental effects (i.e., skeletal malformations, soft tissue malformations, decreased pup weight, embryolethality) observed when single oral dose as low as 10 mg/kg (about 0.2 times total maximum daily human dosage) was administered during period of organogenesis.
Published data to date regarding use in pregnant women have not indicated a clear association between mebendazole and a potential risk of major birth defects or miscarriage. However, these studies cannot definitely establish the absence of any mebendazole-associated risk because of methodological limitations, including recall bias, confounding factors, and, in some cases, small sample size or exclusion of first-trimester mebendazole exposures.
Consider that untreated soil-transmitted helminth infections in pregnancy can be associated with adverse outcomes, including maternal iron deficiency anemia, low birthweight, and neonatal and maternal death.
Lactation
Limited data indicate small amounts of mebendazole distributed into human milk following oral administration. Effects on milk production and on breast-fed infant unknown.
Consider benefits of breast-feeding and importance of mebendazole to the woman; also consider potential adverse effects on breast-fed child from the drug or underlying maternal condition.
Pediatric Use
100-mg chewable tablets: Safety and efficacy not established in children <2 years of age.
500-mg chewable tablets: Safety and efficacy not established in children <1 year of age. Safety profile of single 500-mg chewable tablet in pediatric patients 1–16 years of age is similar to that in adults.
Seizures reported when mebendazole used in children <1 year of age.
Geriatric Use
Data insufficient to determine whether patients ≥65 years of age respond differently to mebendazole than younger patients.
Common Adverse Effects
Nausea, vomiting, abdominal pain, anorexia, diarrhea, flatulence, headache, rash, tinnitus, numbness, dizziness, fever, abnormal liver function tests.
Drug Interactions
Specific Drugs
|
Drug |
Interaction |
Comments |
|---|---|---|
|
Anticonvulsants (carbamazepine, phenytoin) |
Decreased plasma mebendazole concentrations |
Unlikely to be clinically important when treating intestinal infections |
|
Metronidazole |
Stevens-Johnson syndrome/toxic epidermal necrolysis reported with concomitant use |
Avoid concomitant use |
Mebendazole Pharmacokinetics
Absorption
Bioavailability
Minimally absorbed from GI tract. Following oral administration, majority of dose remains in the GI tract where it exerts an anthelmintic effect locally.
Mebendazole 100-mg chewable tablets: Oral dosage of 100 mg twice daily for 3 consecutive days results in plasma concentrations of mebendazole or the 2-amino metabolite (the major metabolite) that are ≤30 or ≤90 ng/mL, respectively.
Mebendazole 500-mg chewable tablets: Single oral dose of 500 mg in healthy adults under fasted conditions results in peak plasma mebendazole concentration of 14 ng/mL attained within 1.5 hours.
Food
Mebendazole 100-mg chewable tablets: Administration with high-fat meal increases bioavailability of mebendazole, but effect on amount of drug remaining in GI tract not expected to be substantial.
Mebendazole 500-mg chewable tablets: Administration with high-fat meal increases bioavailability, increasing peak plasma mebendazole concentration following single oral dose of 500 mg in healthy adults to 56 ng/mL, and prolongs time to peak plasma concentration by approximately 2.5 hours.
Special Populations
Children 1–16 years of age with single or mixed infections of Trichuris trichiura and/or Ascaris lumbricoides: Following a single 500-mg chewable tablet, limited data indicate that systemic exposures in those 1–3 years of age is higher than exposures reported in adults.
Plasma concentrations of mebendazole may be increased in patients with impaired hepatic function, impaired metabolism, or impaired biliary elimination.
Distribution
Extent
Limited data indicate small amounts distributed into human milk following oral administration.
Plasma Protein Binding
90–95%.
Elimination
Metabolism
Extensively metabolized principally in the liver. Metabolized via decarboxylation to 2-amino-5(6)-benzimidazolyl phenylketone.
Metabolites do not have anthelmintic activity.
Elimination Route
<2% of an oral dose of mebendazole is excreted in urine; the remainder is excreted in feces as unchanged drug and metabolites.
Mebendazole and its metabolites likely undergo some degree of enterohepatic recirculation.
Half-life
3–6 hours.
Stability
Storage
Oral
Chewable Tablets
Mebendazole 100-mg chewable tablets: 20–25°C.
Mebendazole 500-mg chewable tablets: <30°C in tightly closed container. Discard unused tablets 1 month after opening the container.
Actions and Spectrum
-
Benzimidazole derivative anthelmintic agent structurally related to albendazole and thiabendazole (not commercially available in US).
-
Interferes with cellular tubulin formation and causes ultrastructural degenerative changes in intestine of susceptible helminths. Disrupts glucose uptake and digestive and reproductive functions, leading to immobilization, inhibition of egg production, and death of the helminth.
-
Active against certain nematodes (roundworms) pathogenic to humans, including Ancylostoma duodenale (hookworm), Angiostrongylus cantonensis, Ascaris lumbricoides, Capillaria philippinensis (Philippine threadworm), Enterobius vermicularis (pinworm), Gnathostoma spinigerum, Necator americanus (hookworm), Trichinella spiralis (pork worm), and Trichuris trichiura (whipworm).
-
Resistance to mebendazole may occur. Although clinical importance unknown, mechanism of resistance may involve changes in parasite β-tubulin protein resulting in reduced binding of the drug to β-tubulin.
Advice to Patients
-
Advise patients that mebendazole may be taken with or without food.
-
Inform patients taking mebendazole 100-mg chewable tablets that the tablets may be chewed, swallowed whole, or crushed and mixed with food.
-
Inform patients taking mebendazole 500-mg chewable tablets that the tablet must be chewed completely before swallowing and should not be swallowed whole. Advise those who have difficulty chewing to place tablet on a spoon and add 2–3 mL of drinking water onto tablet using a dosing syringe. Within 2 minutes, tablet should change into a soft, semi-solid mass that can be swallowed.
-
Advise patients that metronidazole and mebendazole should not be used concomitantly since serious skin reactions have been reported.
-
Importance of informing clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs, as well as any concomitant illnesses.
-
Importance of women informing clinicians if they are or plan to become pregnant or plan to breast-feed.
-
Importance of informing patients of other important precautionary information. (See Cautions.)
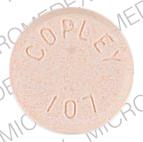
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Tablets, chewable |
100 mg |
Emverm |
Impax |
|
500 mg |
Vermox |
Janssen |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions June 11, 2018. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
† Off-label: Use is not currently included in the labeling approved by the US Food and Drug Administration.
Reload page with references included
Related/similar drugs
More about mebendazole
- Check interactions
- Compare alternatives
- Reviews (9)
- Drug images
- Side effects
- Dosage information
- During pregnancy
- Drug class: anthelmintics
- Breastfeeding
- En español