Levodopa/Carbidopa (Monograph)
Brand name: Lodosyn
Drug class: Dopamine Precursors
- Antiparkinsonian Agents
VA class: CN500
CAS number: 59-92-7
Levodopa/Carbidopa is also contained as an ingredient in the following combinations:
Carbidopa and Levodopa
Introduction
Antiparkinsonian agent; levodopa is the levorotatory isomer of dihydroxyphenylalanine and the metabolic precursor of dopamine, and carbidopa is a decarboxylase inhibitor that inhibits the peripheral decarboxylation of levodopa to dopamine.
Uses for Levodopa/Carbidopa
Parkinsonian Syndrome
Levodopa is used for symptomatic treatment of parkinsonian syndrome, including parkinson disease, postencephalitic parkinsonism, and symptomatic parkinsonian syndrome resulting from carbon monoxide intoxication or manganese intoxication. Available in various fixed-combination preparations with carbidopa for this use.
Carbidopa is used to inhibit decarboxylation of peripheral levodopa and increase the amount of levodopa available for transport to the brain. Available in fixed combination with levodopa and also as a single-entity preparation for use in patients receiving levodopa-carbidopa who require additional carbidopa to reduce nausea and vomiting and/or facilitate more rapid dosage titration.
Levodopa (in combination with carbidopa) is currently the most effective drug for relieving motor symptoms of parkinson disease. However, effectiveness decreases over time and most patients develop motor fluctuations and dyskinesias (drug-induced involuntary movements) with long-term use.
Strategies to reduce risk of motor complications include adjusting dosage of levodopa, adding other antiparkinsonian agents (e.g., dopamine receptor agonist [e.g., pramipexole, ropinirole, rotigotine], selective monoamine oxidase [MAO]-B inhibitor [e.g., rasagiline, safinamide, selegiline], catechol-O-methyltransferase [COMT] inhibitor [e.g., entacapone, tolcapone], amantadine), or initiating other agents first to delay use of levodopa.
Motor complications associated with long-term use of standard oral levodopa formulations are thought to result from fluctuating plasma concentrations due to short half-life, delayed gastric emptying, and erratic absorption. Several non-oral preparations of levodopa and carbidopa (e.g., levodopa oral inhalation powder, carbidopa-levodopa enteral suspension) are available for use in patients with advanced parkinson disease whose motor symptoms are not effectively controlled with oral therapies.
Levodopa oral inhalation powder is used for intermittent treatment of “off” episodes in patients receiving levodopa-carbidopa. Intended for use on an intermittent basis only in patients who are already receiving carbidopa-levodopa therapy. May be particularly useful in patients with severely delayed gastric emptying.
Carbidopa-levodopa enteral suspension is used for treatment of motor fluctuations in patients with advanced parkinson disease. Administered by continuous enteral infusion through a percutaneous endoscopic gastrojejunostomy (PEG-J) tube.
Levodopa/Carbidopa Dosage and Administration
Administration
Levodopa and carbidopa are administered orally as fixed-combination or single-entity (carbidopa only) conventional tablets, orally disintegrating tablets, extended-release tablets, or extended-release capsules. Levodopa also is available as a powder for oral inhalation. Carbidopa-levodopa enteral suspension is administered through a nasojejunal (NJ) tube or a PEG-J tube.
May continue therapy with other antiparkinsonian agents while carbidopa-levodopa is administered; however, dosage adjustments may be necessary.
If general anesthesia required, continue therapy as long as patient permitted to take oral medications. If therapy interrupted, observe patient for symptoms of neuroleptic malignant syndrome (NMS); resume as soon as patient is able to take oral medications. (See Hyperpyrexia and Confusion under Cautions.)
Oral Administration
Administer orally as fixed-combination or single-entity (carbidopa only) conventional (immediate-release) tablets, extended-release tablets, orally disintegrating tablets, or extended-release capsules.
Carbidopa-levodopa conventional tablets and orally disintegrating tablets contain a 1:4 or 1:10 ratio of carbidopa to levodopa. Carbidopa-levodopa extended-release tablets and capsules contain a 1:4 ratio of carbidopa to levodopa. Carbidopa and levodopa also are commercially available as fixed-combination tablets with entacapone (Stalevo) containing a 1:4 ratio of carbidopa to levodopa combined with 200 mg of entacapone.
Extended-release carbidopa-levodopa tablets: Administer as whole or half tablets; do not chew or crush.
Extended-release carbidopa-levodopa capsules: Swallow whole without regard to food; do not chew, divide, or crush. In patients with difficulty swallowing, may open capsules and sprinkle entire contents on a small amount (e.g., 1–2 tablespoons) of applesauce; administer mixture immediately and do not store for later use.
Orally disintegrating carbidopa-levodopa tablets: Just prior to administration, gently remove tablet from the bottle with dry hands. Place tablet on tongue to dissolve (usually within seconds) and swallow with saliva. Administration with water is not necessary.
Fixed-combination carbidopa, levodopa, and entacapone tablets (Stalevo): Do not divide tablets; administer only one tablet per dosing interval.
Oral Inhalation
Administer levodopa powder with a special oral inhalation device (Inbrija inhaler) that delivers powdered drug from capsules. A total of 2 capsules (each containing 42 mg of levodopa) is required for the recommended dose. Do not swallow capsules as the intended effect will not be obtained.
To administer a dose, load first capsule into inhaler. Before inhaling the dose, exhale completely as possible. While keeping inhaler level, place mouthpiece of inhaler between the lips and inhale deeply and slowly through the inhaler; the patient should feel or hear a whirling sound, which is an indication that the inhaler is working. After inhaling contents of capsule, hold breath for 5 seconds before exhaling. Repeat these steps with the second capsule to complete full dose.
Use a new inhaler with each new carton of drug.
Consult manufacturer's prescribing information for additional details.
Enteral Administration
Administer carbidopa-levodopa enteral suspension (Duopa) as a 16-hour continuous infusion through a PEG-J tube using a portable infusion device (i.e., CADD Legacy 1400 pump). PEG-J tube placement and removal should be performed by a gastroenterologist or other experienced healthcare provider. May temporarily administer through an NJ tube (e.g., as a trial to determine whether patient responds to therapy and can manage device) until a permanent PEG-J tube can be established.
Enteral suspension is commercially available in single-use cassettes containing 4.63 mg of carbidopa and 20 mg of levodopa per mL.
Store cassettes in freezer prior to use. (See Storage under Stability.) Prior to administration, remove cassette from refrigerator and allow to reach room temperature for 20 minutes. Failure to administer drug at room temperature may result in a subtherapeutic response. Cassettes are for single-use only; do not use for longer than 16 hours and discard cassette after this time period even if some drug remains.
At end of the daily 16-hour administration period, disconnect PEG-J tube from the pump and flush with room temperature potable water.
Consult manufacturer's prescribing information for additional details.
Dosage
Dosage expressed in terms of levodopa and carbidopa.
Adjust dosage carefully according to individual requirements, response, and tolerance.
Daily dosage of carbidopa should be at least 70–100 mg daily; patients receiving <70–100 mg daily are likely to experience nausea and vomiting.
Observe patient closely if dosage is reduced abruptly or drug is discontinued; risk of precipitating a symptom complex resembling neuroleptic malignant syndrome (NMS). Gradually reduce dosage when treatment is discontinued. (See Hyperpyrexia and Confusion under Cautions.)
Adults
Parkinsonian Syndrome
Carbidopa-Levodopa Conventional Tablets or Orally Disintegrating Tablets
OralInitially, carbidopa 25 mg/levodopa 100 mg (as 1 tablet) 3 times daily. May increase dosage by 1 tablet (carbidopa 25 mg/levodopa 100 mg) daily or every other day until a daily dosage of carbidopa 200 mg/levodopa 800 mg is reached.
Alternatively, initiate with carbidopa 10 mg/levodopa 100 mg (as 1 tablet) 3 or 4 times daily; however, this dosage will not provide an adequate dose of carbidopa for most patients. May increase dosage by 1 tablet (carbidopa 10 mg/levodopa 100 mg) daily or every other day until a daily dosage of carbidopa 80 mg/levodopa 800 mg is reached.
Individualize maintenance dosage according to desired therapeutic response. Patients should receive at least 70–100 mg of carbidopa daily during maintenance therapy.
Use of combination preparations containing a 1:10 ratio of carbidopa to levodopa may not provide an adequate amount of carbidopa. If a greater proportion of carbidopa is required, may substitute 1 tablet of carbidopa 25 mg/levodopa 100 mg for 1 tablet of carbidopa 10 mg/levodopa 100 mg. If additional carbidopa is still required, may administer a 25-mg dose of carbidopa (as the single-entity tablet preparation) with each first daily dose of carbidopa-levodopa; may give additional 12.5-mg or 25-mg doses of carbidopa with each subsequent dose of carbidopa-levodopa as needed.
If patients require higher dosages of levodopa while receiving a combination preparation containing 100 mg of levodopa, switch patients to a preparation containing 250 mg of levodopa.
Carbidopa-Levodopa Extended-release Tablets
OralExtended-release tablets are not bioequivalent to immediate-release tablets; adjust dosage appropriately when converting patients between the formulations. (See Bioavailability under Pharmacokinetics.)
Patients currently receiving immediate-release levodopa preparations: Convert to an appropriate dosage of the extended-release tablets that provides approximately 10% more levodopa daily than dosage previously received as the immediate-release preparation; levodopa dosage may need to be increased up to 30% more daily, depending on response.
Levodopa-naive patients: Initially, carbidopa 50 mg/levodopa 200 mg (as 1 extended-release tablet) twice daily; initial dosage should not be given at intervals <6 hours. Adjust dose or dosing frequency based on response and tolerance at intervals ≥3 days. Most patients are treated adequately with dosages that provide 400–1600 mg of levodopa, administered in divided doses at intervals ranging from 4–8 hours while awake. Higher dosages (≥2400 mg of levodopa per day) and shorter intervals (<4 hours) have been used but usually are not recommended. If the dosing interval is <4 hours and/or the divided doses are not equal, it is recommended that the smaller doses be given at the end of the day.
When additional levodopa is needed for symptomatic control, may consider adding doses of a conventional preparation of carbidopa-levodopa during brief periods of the day.
Carbidopa-Levodopa Extended-release Capsules
OralExtended-release capsules are not bioequivalent to immediate-release preparations; adjust dosage appropriately when converting patients between the formulations. (See Bioavailability under Pharmacokinetics.)
Patients currently receiving immediate-release levodopa preparations: Calculate patient's current total daily dosage of levodopa and convert to an appropriate starting dosage of the extended-release capsules (see Table 1). Following conversion, adjust dose and/or dosing interval as necessary based on patient tolerance and clinical response. In patients currently receiving carbidopa-levodopa in combination with a COMT inhibitor (e.g., entacapone), may need to increase total initial daily dose of levodopa in the extended-release capsule.
|
Total Daily Dose of Levodopa in Immediate-release Carbidopa-Levodopa |
Total Daily Dose of Levodopa in Extended-release Capsules |
|---|---|
|
400–549 mg |
855 mg (administered as 3 capsules [carbidopa 23.75 mg and levodopa 95 mg] 3 times daily) |
|
550–749 mg |
1140 mg (administered as 4 capsules [carbidopa 23.75 mg and levodopa 95 mg] 3 times daily) |
|
750–949 mg |
1305 mg (administered as 3 capsules [carbidopa 36.25 mg and levodopa 145 mg] 3 times daily) |
|
950–1249 mg |
1755 mg (administered as 3 capsules [carbidopa 48.75 mg and levodopa 195 mg] 3 times daily) |
|
≥1250 mg |
2340 mg (administered as 4 capsules [carbidopa 48.75 mg and levodopa 195 mg] 3 times daily) or 2205 mg (administered as 3 capsules [carbidopa 61.25 mg and levodopa 245 mg] 3 times daily) |
Levodopa-naive patients: Initially, carbidopa 23.75 mg/levodopa 95 mg (as extended-release capsules) 3 times daily for the first 3 days. May increase to carbidopa 36.25 mg/levodopa 145 mg 3 times daily on the fourth day of treatment. Thereafter, may increase dosage based on patient tolerance and clinical response up to a maximum of carbidopa 97.5 mg/levodopa 390 mg 3 times daily; if needed, dosing frequency may be increased to a maximum of 5 times daily. Maintain patients on the lowest possible dosage necessary to achieve adequate symptom control while minimizing adverse effects.
Carbidopa, Levodopa, and Entacapone Fixed-combination Tablets
OralPatients currently receiving carbidopa-levodopa conventional tablets with entacapone: May substitute with corresponding strength of the combination tablet containing same amounts of carbidopa and levodopa. No experience transitioning patients receiving carbidopa-levodopa extended-release tablets or carbidopa-levodopa preparations not containing a 1:4 ratio.
Patients not currently receiving entacapone: Initially titrate to a tolerable and effective dose using separate carbidopa-levodopa and entacapone tablets. Once optimum dosage established, may convert patients to a corresponding dosage of the carbidopa-levodopa-entacapone combination tablet.
Carbidopa Tablets
OralCarbidopa: 25 mg with first dose of carbidopa/levodopa each day for patients who need additional carbidopa; additional 12.5- or 25-mg doses may be given during the day with each dose of carbidopa/levodopa.
Levodopa Oral Inhalation Powder (Inbrija)
Oral InhalationInhale contents of 2 capsules (total of 84 mg) as needed for “off” symptoms, up to 5 times daily.
Maximum recommended dose per “off” period is 84 mg and maximum daily dosage is 420 mg.
Carbidopa-Levodopa Enteral Suspension (Duopa)
EnteralDosage of carbidopa-levodopa enteral suspension consists of 3 components: a morning dose (administered usually over 10–30 minutes), a continuous infusion (administered over 16 hours), and additional doses (i.e., extra doses) as needed for breakthrough symptoms.
Prior to initiating treatment, convert patient from all forms of levodopa to oral immediate-release carbidopa-levodopa tablets (1:4 ratio). Dosage of enteral suspension is based on amount of oral levodopa taken the previous day.
Determine initial morning dose of enteral suspension (in mL) as follows: calculate the total amount of levodopa (in mg) in the first dose of immediate-release carbidopa-levodopa taken the previous day. Convert this dose (in mg) to mL by multiplying by 0.8 and dividing by 20 mg/mL; add an additional 3 mL to account for priming volume.
Determine initial continuous dose of enteral suspension (in mL) as follows: calculate the total amount of levodopa from oral immediate-release carbidopa-levodopa doses taken throughout the previous day (over 16 waking hours); do not use doses taken at night in the calculation. Subtract the first oral levodopa dose taken the previous day (determined in morning dose calculation) from the total oral levodopa dose taken over 16 hours; divide this value by 20 mg/mL to obtain the continuous dose that should be administered over 16 hours. Calculate hourly infusion rate (in mL/hour) by dividing continuous dose by 16 hours.
After the first day of treatment, titrate daily morning dose and continuous dose based on individual response and tolerability until a stable dosage is obtained. (See Prescribing Limits.) If patient experiences persistent or numerous “off” periods during the 16-hour infusion period, may increase continuous dose or administer extra doses. In patients who require overnight treatment, an extended-release formulation of oral levodopa-carbidopa may be taken at bedtime after stopping the enteral infusion. If dyskinesias or other adverse effects occur, may decrease continuous dose or temporarily interrupt therapy until adverse effects subside. Consult manufacturer's prescribing information for recommendations on dosage adjustments.
Avoid sudden discontinuance of therapy or rapid dose reduction; when discontinuing therapy, taper dosage or switch patients to oral immediate-release carbidopa-levodopa therapy.
Prescribing Limits
Adults
Parkinsonian Syndrome
Oral
Carbidopa: Experience with dosages >200 mg daily limited.
Carbidopa-levodopa extended-release capsules: Manufacturer recommends a maximum daily dose of carbidopa 612.5 mg and levodopa 2450 mg.
Carbidopa-levodopa-entacapone fixed-combination tablets: If preparations containing carbidopa 12.5–37.5 mg, levodopa 50–150 mg, and entacapone 200 mg (Stalevo 50, 75, 100, 125, and 150) are used, maximum of 8 tablets daily. If preparation containing carbidopa 50 mg, levodopa 200 mg, and entacapone 200 mg (Stalevo 200) is used, maximum of 6 tablets daily.
Levodopa oral inhalation: Maximum recommended dose per “off” period is 84 mg and maximum daily dosage is 420 mg.
Carbidopa-levodopa enteral suspension: Maximum recommended daily dose is 2000 mg of the levodopa component (i.e., one cassette per day).
Cautions for Levodopa/Carbidopa
Contraindications
-
Concomitant use with a nonselective MAO inhibitor. (See Specific Drugs and Foods under Interactions.)
-
Angle-closure glaucoma.
-
Known hypersensitivity to levodopa, carbidopa, or any ingredient in the formulation.
Warnings/Precautions
Warnings
Motor Complications
Therapy associated with dyskinesias; dosage reduction of levodopa-carbidopa or other antiparkinsonian agents may be needed.
Motor fluctuations also may occur with long-term use. May manifest as “end-of-dose” effect, sudden loss of effectiveness with abrupt onset of akinesia followed by sudden return of effectiveness (“on-off” phenomenon), or sudden hypotonic freezing (patient falls frequently while attempting to walk).
Neuropsychiatric Effects
Psychiatric disturbances reported. Observe patients carefully for depression with concomitant suicidal tendencies. Depression reported with increased frequency in patients receiving enteral carbidopa-levodopa suspension compared with oral immediate-release preparation.
Hallucinations and abnormal thoughts or behavior (e.g., paranoia, confusion, psychotic disorder, agitation, delusions, delirium, psychotic-like behavior, disorientation, aggressive behavior) reported with dopaminergic drugs. Hallucinations generally occur soon after initiation of levodopa therapy and may be alleviated by reducing dosage.
Generally avoid use in patients with major psychotic disorders.
Generalized neuropathy, most often characterized as sensory or sensorimotor, reported in patients receiving carbidopa-levodopa enteral suspension. Electrodiagnostic findings most consistent with axonal polyneuropathy. Evaluate patients for neuropathy prior to and during treatment, particularly in those with preexisting neuropathy or risk of neuropathy. Vitamin B supplementation reported to decrease incidence of neuropathy.
Cardiovascular Effects
Risk of orthostatic hypotension; usually asymptomatic and tolerance usually develops within a few months.
Cardiac ischemic events reported with use of some preparations.
Use with caution in patients with a history of MI who have residual atrial, nodal, or ventricular arrhythmias; monitor cardiac function in a facility with intensive cardiac care during initial dosage adjustment.
Use with caution in patients with severe cardiovascular disease.
Respiratory Effects
Use with caution in patients with severe pulmonary disease (e.g., bronchial asthma).
Coughing is a frequent adverse effect of levodopa oral inhalation therapy. Clinically important changes in pulmonary function not observed; however, this dosage form is not recommended in patients with COPD, asthma, or other chronic lung diseases.
GI Effects
Use with caution in patients with a history of peptic ulcers; possibility of upper GI hemorrhage in these patients.
Complications associated with the PEG-J procedure or device (e.g., bezoar; ileus; implant site erosion/ulcer; intestinal hemorrhage, ischemia, obstruction, or perforation; intussusception; pancreatitis; peritonitis; pneumoperitoneum; postoperative wound infection) may occur in patients receiving carbidopa-levodopa enteral suspension; may result in serious outcomes such as death or need for surgery. Instruct patients to notify a clinician immediately if they experience abdominal pain, prolonged constipation, nausea, vomiting, fever, or melanotic stool.
Falling Asleep During Activities of Daily Living and Somnolence
Episodes of falling asleep while engaged in activities of daily living (e.g., driving) reported, sometimes resulting in accidents.
Some patients perceived no warning signs (e.g., excessive drowsiness) and believed they were alert immediately prior to the event.
Monitor patients for drowsiness or sleepiness. Patients may not acknowledge drowsiness or sleepiness until directly questioned about such adverse effects during specific activities. Ask patients about any factors that may increase the risk of somnolence (e.g., concomitant sedating drugs, presence of sleep disorders).
Consider discontinuing therapy if a patient develops daytime sleepiness or episodes of falling asleep during activities that require active participation (e.g., conversations, eating). If the drug is continued, advise patients not to drive and to avoid other potentially dangerous activities. (See Advice to Patients.) Insufficient information to establish whether dosage reduction will eliminate this adverse event.
Hyperpyrexia and Confusion
Symptom complex resembling neuroleptic malignant syndrome (NMS; e.g., elevated temperature, muscular rigidity, altered consciousness, autonomic instability) reported following dosage reduction or abrupt withdrawal of levodopa.
Observe patient closely when dosage is reduced or drug discontinued; especially important in patients receiving concomitant therapy with an antipsychotic agent.
General Precautions
Evaluate hepatic, hematopoietic, cardiovascular, and renal function periodically.
Use of Fixed Combinations
When the fixed-combination preparation containing levodopa, carbidopa, and entacapone (Stalevo) is used, observe the usual precautions and contraindications associated with all drugs in the preparation.
Glaucoma
May increase IOP in patients with glaucoma; use with caution in patients with well-controlled open-angle glaucoma and monitor IOP. (See Contraindications under Cautions.)
Endocrine Disorders
Use with caution.
Closely monitor diabetic patients; levodopa may affect glycemic control.
Melanoma
Epidemiologic studies indicate patients with parkinsonian syndrome have a twofold to approximately sixfold higher risk of developing melanoma than the general population. Unclear whether increased risk is due to parkinsonian syndrome or other factors (e.g., drugs used to treat the disease).
Monitor for melanoma on a frequent and regular basis. Manufacturer recommends periodic skin examinations performed by appropriately qualified individuals (e.g., dermatologists).
Intense Urges
Intense urges (e.g., urge to gamble, increased sexual urges, other intense urges) and inability to control these urges reported in some patients receiving antiparkinsonian agents that increase central dopaminergic tone (including levodopa-carbidopa). Urges stopped in some cases when dosage was reduced or drug was discontinued.
Consider reducing dosage or discontinuing therapy if a patient develops such urges.
Phenylketonuria with Orally Disintegrating Tablets
Levodopa-carbidopa orally disintegrating tablets contain aspartame (NutraSweet), which is metabolized in the GI tract to phenylalanine.
Specific Populations
Pregnancy
No adequate and well-controlled studies in pregnant women; in animal reproductive studies, decreased pup viability and teratogenic effects (e.g., visceral and skeletal malformations) observed.
Weigh risks versus benefits in women of childbearing potential.
Lactation
Levodopa is distributed into human milk; caution advised. Carbidopa is distributed into milk in rats; not known whether carbidopa is distributed into human milk.
Use caution in nursing women. Consider known benefits of breast-feeding along with mother's clinical need for the drug and any potential adverse effects on the infant from drug or underlying maternal condition.
Pediatric Use
Safety and efficacy not established in children <18 years of age.
Geriatric Use
Oral preparations: No overall differences in safety or efficacy relative to younger adults.
Levodopa oral inhalation: Cough, upper respiratory tract infection, nausea, vomiting, extremity pain, and discolored nasal discharge were reported with higher frequency in geriatric patients ≥65 years of age than younger adults.
Hepatic Impairment
Use with caution.
Renal Impairment
Use with caution.
Common Adverse Effects
Dyskinesias, nausea, vomiting, headache, insomnia, abnormal dreams, dry mouth, anxiety, constipation, orthostatic hypotension.
Levodopa oral inhalation: Cough, nausea, upper respiratory tract infection, discolored sputum.
Carbidopa-levodopa enteral suspension: Complications from device insertion, nausea, depression, peripheral edema, hypertension, upper respiratory tract infection, oropharyngeal pain, atelectasis, incision site erythema.
Drug Interactions
Specific Drugs and Foods
|
Drug or Food |
Interaction |
Comments |
|---|---|---|
|
Anticholinergic agents |
Potential for decreased tremor and/or exacerbation of abnormal involuntary movements Possible delay in levodopa absorption and increase in gastric metabolism of levodopa |
|
|
Antidepressants, tricyclic |
Potential for hypertension and dyskinesia |
Use concomitantly with caution |
|
Antipsychotic agents (phenothiazines, butyrophenones, risperidone) |
Possible reduction in the therapeutic effects of levodopa Possible increased risk of NMS (see Hyperpyrexia and Confusion under Cautions) |
Observe patient for loss of therapeutic effect |
|
Benzodiazepines |
Possible reduction in the therapeutic effects of levodopa with chlordiazepoxide or diazepam |
Use concomitantly with caution |
|
Dopamine-depleting agents (e.g., reserpine, tetrabenazine) |
Concomitant use not recommended |
|
|
Hypotensive agents |
Potential for symptomatic postural hypotension Potential for toxic CNS effects such as psychosis with methyldopa |
Dosage adjustment of the hypotensive agent may be needed |
|
Iron preparations |
Possible decreased absorption of levodopa and carbidopa |
Administer concomitantly with caution and monitor patients for worsening parkinsonian symptoms; some clinicians recommend that iron supplements be taken at least 2 hours before or after levodopa |
|
Isoniazid |
Possible reduction in the therapeutic effects of levodopa |
Observe patient for loss of therapeutic effect |
|
MAO inhibitors |
Potential for hypertension, headache, hyperexcitability with nonselective MAO inhibitors Possible severe orthostatic hypotension with selegiline |
Contraindicated with nonselective MAO inhibitors; discontinue nonselective MAO inhibitor at least 2 weeks prior to initiation of levodopa May be administered concomitantly with a selective MAO inhibitor (e.g., selegiline) with caution |
|
Metoclopramide |
Possible increase in bioavailability of levodopa Possible reduction in the therapeutic effects of levodopa |
|
|
Papaverine |
Possible reduction in the therapeutic effects of levodopa |
Use concomitantly with caution and observe patient for loss of therapeutic effect |
|
Phenytoin |
Possible reduction in the therapeutic effects of levodopa |
Use concomitantly with caution and observe patient for loss of therapeutic effect |
|
Protein |
High protein foods may impair absorption of levodopa |
Levodopa/Carbidopa Pharmacokinetics
Absorption
Bioavailability
Levodopa is absorbed from the GI tract; peak plasma concentrations achieved within 0.5 or 2 hours following administration of conventional tablets or extended-release tablets, respectively.
Carbidopa-levodopa immediate-release preparations: Conventional tablets and orally disintegrating tablets begin to release the drugs within 30 minutes of administration. Pharmacokinetic values for orally disintegrating tablet and immediate-release tablet are similar.
Carbidopa-levodopa extended-release tablets: Bioavailability of levodopa from extended-release tablets 70–75% of that from conventional tablets. Extended-release tablets result in less fluctuation in plasma concentrations between doses than conventional tablets.
Carbidopa-levodopa extended-release capsules: Formulated with both immediate-release and extended-release components. Following oral administration, plasma levodopa concentrations initially increase rapidly, followed by sustained plasma concentrations for about 4–5 hours; minimal peak to trough fluctuation. Bioavailability of levodopa from extended-release capsules approximately 70% relative to immediate-release preparations. Peak levodopa concentration is 30% of that achieved with immediate-release preparations at comparable doses.
Levodopa oral inhalation: Following oral inhalation of a single dose, peak plasma concentrations obtained in approximately 0.5 hours. Bioavailability of levodopa from oral inhalation powder approximately 70% relative to immediate-release oral levodopa tablets. Time to peak plasma concentration is approximately 15 minutes faster, but peak plasma concentrations and systemic exposure are substantially lower, compared with orally administered immediate-release levodopa-carbidopa tablets.
Carbidopa-levodopa enteral suspension: Following initiation of the 16-hour infusion, peak plasma concentrations of levodopa obtained in 2.5 hours. Bioavailability of enteral suspension comparable to conventional tablets. However, enteral suspension associated with less variability in plasma concentrations than conventional tablets. Absorption not influenced by gastric emptying rate.
Food
Effects of food on levodopa pharmacokinetics are variable due to differences in formulations, dosages, and study designs.
High protein diet may interfere with absorption of levodopa from conventional preparations.
Extended-release tablets: Food increases bioavailability and peak plasma concentrations of levodopa.
Extended-release capsules: Food decreased peak plasma concentration by 21% and increased AUC of levodopa by 13%; absorption delayed by approximately 2 hours.
Distribution
Extent
Widely distributed.
<1% of levodopa penetrates the CNS; carbidopa does not cross the blood-brain barrier.
Plasma Protein Binding
Levodopa: 10–30%.
Carbidopa: About 36%.
Elimination
Metabolism
Levodopa is metabolized in the stomach and intestine and on first pass through the liver; absorbed levodopa decarboxylated to dopamine.
Carbidopa inhibits peripheral decarboxylation of levodopa, thus increasing availability of levodopa for distribution into the CNS.
Elimination Route
Levodopa is excreted in urine as metabolites.
Half-life
Levodopa: 1.5 hours when administered with carbidopa.
Stability
Storage
Oral
Conventional Carbidopa-Levodopa Tablets
Tightly closed container at 25°C (may be exposed to 15–30°C). Protect from light and moisture.
Extended-release Carbidopa-Levodopa Tablets
Tightly closed container at 25°C (may be exposed to 15–30°C); protect from light and moisture.
Orally Disintegrating Carbidopa-Levodopa Tablets
Tightly closed container at 20–25°C; protect from light and moisture.
Extended-release Carbidopa-Levodopa Capsules
Tightly closed container at 25°C (may be exposed to 15–30°C); protect from light and moisture.
Levodopa Powder for Oral Inhalation
Store inhaler and capsules in a dry place at 20–25°C (may be exposed to 15–30°C).
Keep capsules in blister pack until ready to use.
Do not store capsules in inhalers.
Carbidopa-Levodopa Enteral Suspension
Store cassettes in freezer at -20°C. Thaw in refrigerator at 2–8°C prior to dispensing. Protect cassettes from light and keep in carton prior to use.
Levodopa/Carbidopa Mechanism of Action
-
Manifestations of parkinsonian syndrome are related to depletion of dopamine in the corpus striatum.
-
Levodopa relieves symptoms of parkinsonism presumably by increasing dopamine concentrations in the brain.
-
Carbidopa inhibits the peripheral decarboxylation of levodopa by aromatic l-amino acid decarboxylase without affecting metabolism of the drug within CNS.
Advice to Patients
-
Importance of taking levodopa/carbidopa as directed. Importance of not altering the prescribed dosage regimen or adding other antiparkinsonian drugs without consulting a clinician.
-
Importance of informing patients with phenylketonuria that the orally disintegrating tablets contain aspartame.
-
Advise patient to notify clinician if abnormal involuntary movements appear or get worse; dosage adjustment may be needed.
-
Advise patient of expected onset and duration of effect.
-
Possibility that dark color (red, brown, black) may appear in saliva, urine, or sweat; garments may be discolored.
-
Advise patient that a change in diet to food high in protein may delay absorption of levodopa and reduce systemic availability. Excess acidity also may delay absorption.
-
Importance of informing clinician of existing or contemplated concomitant therapy, including prescription and OTC drugs and dietary or herbal products.
-
Risk of somnolence and episodes of sudden sleep onset; importance of exercising caution when driving or operating machinery and of refraining from such activities if somnolence and/or an episode of sudden sleep onset occurs.
-
Importance of instructing patients on proper administration of levodopa powder for oral inhalation using the specific inhaler provided by the manufacturer. Instruct patients to take a dose when the return of their parkinsonian symptoms (“off” periods) first occurs. Importance of reminding patients that the contents of Inbrija capsules are for oral inhalation only and must not be swallowed.
-
Importance of instructing patients on proper administration of carbidopa-levodopa enteral suspension through the PEG-J tube and use of the ambulatory pump. Advise patients that if the pump is disconnected for short periods of time (e.g., <2 hours to swim, shower, or for a short medical procedure), no supplemental oral medication is needed, but an extra dose of the enteral suspension may be given before disconnecting. If the pump is disconnected for periods >2 hours, the patient should contact their clinician and take oral carbidopa-levodopa until the enteral infusion can be resumed.
-
Importance of asking patients whether they have developed any new or increased gambling urges, sexual urges, or other urges while receiving levodopa-carbidopa and of advising them of the importance of reporting such urges.
-
Importance of frequent monitoring for melanoma and periodic dermatologic examinations by a dermatologist.
-
Importance of women informing clinician if they are or plan to become pregnant or plan to breast-feed.
-
Importance of advising patients of other important precautionary information. (See Cautions.)
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Tablets |
25 mg (of anhydrous carbidopa)* |
Carbidopa Tablets |
|
|
Lodosyn (scored) |
Valeant |
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral Inhalation |
Powder for inhalation (contained in capsules) |
42 mg |
Inbrija |
Acorda |
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Capsules, extended-release |
Carbidopa 23.75 mg (of anhydrous carbidopa) and Levodopa 95 mg |
Rytary |
Impax |
|
Carbidopa 36.25 mg (of anhydrous carbidopa) and Levodopa 145 mg |
Rytary |
Impax |
||
|
Carbidopa 48.75 mg (of anhydrous carbidopa) and Levodopa 195 mg |
Rytary |
Impax |
||
|
Carbidopa 61.25 mg (of anhydrous carbidopa) and Levodopa 245 mg |
Rytary |
Impax |
||
|
Suspension, enteral |
4.63 mg (of anhydrous carbidopa) per mL and 20 mg (of levodopa) per mL |
Duopa (available as single-use 100-mL cassettes) |
AbbVie |
|
|
Tablets |
Carbidopa 10 mg (of anhydrous carbidopa) and Levodopa 100 mg* |
Carbidopa and Levodopa Tablets |
||
|
Sinemet (scored) |
Merck |
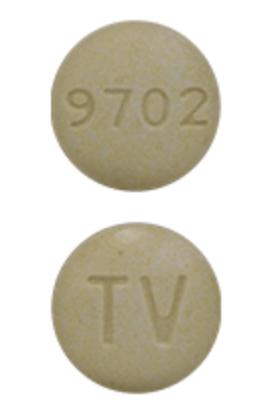
|||
|
Carbidopa 25 mg (of anhydrous carbidopa) and Levodopa 100 mg* |
Carbidopa and Levodopa Tablets |
|||
|
Sinemet (scored) |
Merck |
|||
|
Carbidopa 25 mg (of anhydrous carbidopa) and Levodopa 250 mg* |
Carbidopa and Levodopa Tablets |
|||
|
Sinemet (scored) |
Merck |
|||
|
Tablets, extended-release |
Carbidopa 50 mg (of anhydrous carbidopa) and Levodopa 200 mg* |
Carbidopa and Levodopa Extended-release Tablets |
||
|
Sinemet CR |
Merck |
|||
|
Carbidopa 25 mg (of anhydrous carbidopa) and Levodopa 100 mg* |
Carbidopa and Levodopa Extended-release Tablets |
|||
|
Sinemet CR |
Merck |
|||
|
Tablets, orally disintegrating |
Carbidopa 10 mg (of anhydrous carbidopa) and Levodopa 100 mg* |
Carbidopa and Levodopa Orally-disintegrating Tablets |
||
|
Carbidopa 25 mg (of anhydrous carbidopa) and Levodopa 100 mg* |
Carbidopa and Levodopa Orally-disintegrating Tablets |
|||
|
Carbidopa 25 mg (of anhydrous carbidopa) and Levodopa 250 mg* |
Carbidopa and Levodopa Orally-disintegrating Tablets |
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Tablets, film-coated |
Carbidopa 12.5 mg (of anhydrous carbidopa) with Entacapone 200 mg and Levodopa 50 mg |
Stalevo |
Novartis |
|
Carbidopa 18.75 mg (of anhydrous carbidopa) with Entacapone 200 mg and Levodopa 75 mg |
Stalevo |
Novartis |
||
|
Carbidopa 25 mg (of anhydrous carbidopa) with Entacapone 200 mg and Levodopa 100 mg |
Stalevo |
Novartis |
||
|
Carbidopa 31.25 mg (of anhydrous carbidopa) with Entacapone 200 mg and Levodopa 125 mg |
Stalevo |
Novartis |
||
|
Carbidopa 37.5 mg (of anhydrous carbidopa) with Entacapone 200 mg and Levodopa 150 mg |
Stalevo |
Novartis |
||
|
Carbidopa 50 mg (of anhydrous carbidopa) with Entacapone 200 mg and Levodopa 200 mg |
Stalevo |
Novartis |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions November 1, 2021. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
Reload page with references included
Related/similar drugs
Frequently asked questions
- How long does it take carbidopa levodopa to work?
- How often should carbidopa/levodopa be taken?
- Can carbidopa/levodopa cause high blood pressure?
- What foods should be avoided when taking levodopa?
- Is Rytary better than Sinemet?
- What is the difference between carbidopa, levodopa, and Rytary?
- How long does it take for Rytary to start working?
- How long does Rytary stay in your system?
More about carbidopa / levodopa
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (118)
- Drug images
- Side effects
- Dosage information
- Patient tips
- During pregnancy
- Support group
- Drug class: dopaminergic antiparkinsonism agents
Patient resources
Professional resources
- Carbidopa and Levodopa prescribing information
- Carbidopa and Levodopa ER Capsules (FDA)
- Carbidopa and Levodopa ODT (FDA)
- Carbidopa and Levodopa Tablets (FDA)
Other brands
Sinemet, Rytary, Crexont, Sinemet CR, ... +3 more