The originating document has been archived. We cannot confirm the completeness, accuracy, or currency of the content.
Atazanavir Sulfate (Monograph)
Brand name: Reyataz
Drug class: HIV Protease Inhibitors
Introduction
Antiretroviral; HIV protease inhibitor (PI).
Uses for Atazanavir Sulfate
Treatment of HIV Infection
Treatment of HIV-1 infection in adults, adolescents, and pediatric patients ≥3 months of age weighing ≥5 kg; used in conjunction with other antiretrovirals. Use of ritonavir-boosted atazanavir in antiretroviral-experienced patients should be guided by the number of baseline primary HIV protease inhibitor (PI) resistance substitutions. Atazanavir is not recommended for use in patients <3 months because of the risk of kernicterus.
Ritonavir-boosted or cobicistat-boosted atazanavir is used with a dual-nucleoside reverse transcriptase inhibitor (NRTI) “backbone” of a fully suppressive antiretroviral regimen; consult guidelines for the most current information on recommended regimens. Selection of an initial antiretroviral regimen should be individualized based on factors such as virologic efficacy, toxicity, pill burden, dosing frequency, drug-drug interaction potential, resistance test results, comorbid conditions, access, and cost.
Commercially available as a single-entity preparation and in a fixed-dose combination preparation that also contains cobicistat; refer to the full prescribing information for administration of the combination product.
Postexposure Prophylaxis following Occupational Exposure to HIV (PEP)
Postexposure prophylaxis of HIV infection following occupational exposure† [off-label] (PEP) in health-care personnel and others exposed via percutaneous injury (e.g., needlestick, cut with sharp object) or mucous membrane or nonintact skin (e.g., chapped, abraded, dermatitis) contact with blood, tissue, or other body fluids that might contain HIV.
USPHS recommends a 3-drug regimen of raltegravir and emtricitabine and tenofovir DF as preferred regimen for PEP following occupational exposure to HIV. Ritonavir-boosted atazanavir and 2 NRTIs is one of several alternative regimens. Preferred dual NRTI option for PEP regimens is emtricitabine and tenofovir DF; alternatives are tenofovir DF and lamivudine, zidovudine and lamivudine, or zidovudine and emtricitabine.
Management of occupational exposures to HIV is complex and evolving; consult infectious disease specialist, clinician with expertise in administration of antiretroviral agents, and/or National Clinicians’ Postexposure Prophylaxis Hotline (PEPline at 888-448-4911) whenever possible. Do not delay initiation of PEP while waiting for expert consultation.
Atazanavir Sulfate Dosage and Administration
General
Pretreatment Screening
-
Perform renal laboratory testing (serum creatinine, estimated creatinine clearance, and urinalysis with microscopic examination) in all patients prior to initiation of atazanavir.
-
Perform hepatic laboratory testing in patients with underlying liver disease prior to initiation of atazanavir.
Patient Monitoring
-
Perform renal laboratory testing (serum creatinine, estimated creatinine clearance, and urinalysis with microscopic examination) during treatment with atazanavir.
-
Perform hepatic laboratory testing in patients with underlying liver disease during treatment with atazanavir.
-
Monitor ECG in patients with preexisting conduction system disease or when atazanavir is administered with other drugs that may prolong the PR interval.
-
Monitor liver enzymes in patients with hepatitis B virus (HBV) or hepatitis C virus (HCV) coinfection.
Dispensing and Administration Precautions
-
Atazanavir is commercially available as a single entity and in a fixed-combination preparation containing atazanavir and cobicistat (atazanavir/cobicistat; Evotaz). Refer to the full prescribing information for specific uses of the combination product. Since the antiretroviral agents contained in the fixed combination preparations also may be available in single-entity or other fixed-combination preparations, exercise care to ensure that therapy is not duplicated if a fixed combination is used in conjunction with other antiretrovirals.
Administration
Oral Administration
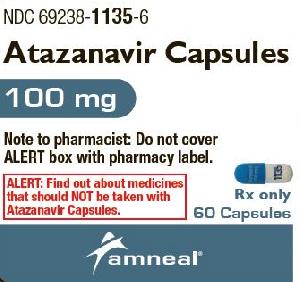
Available as capsules or oral powder.
Administer in combination with other antiretroviral agents for the treatment of human immunodeficiency virus type 1 (HIV-1) infection.
Administer orally in conjunction with low-dose ritonavir (ritonavir-boosted atazanavir) or unboosted (without low-dose ritonavir) once daily with food.
If used concomitantly with certain drugs (e.g., antacids, buffered medications, didanosine, histamine H2-receptor antagonists), dosage adjustments may be needed and/or doses of atazanavir and the other drug may need to be given at separate times.
Capsules
Swallow capsules whole; do not open.
Used in adults, adolescents, and pediatric patients ≥6 years of age.
Usually administered with low-dose ritonavir (ritonavir-boosted atazanavir); may be used without low-dose ritonavir in adults and adolescents ≥13 years of age weighing ≥40 kg who are unable to tolerate ritonavir.
Oral Powder
Provided in single-use packets containing 50 mg of atazanavir as an oral powder; must be mixed with food or beverage prior to administration.
Used in pediatric patients ≥3 months of age weighing ≥5 kg.
Must be administered with low-dose ritonavir (ritonavir-boosted atazanavir). Administer low-dose ritonavir immediately following the atazanavir dose.
Store atazanavir powder in original packet; do not open until ready to use.
Prior to mixing the oral powder, determine the number of packets (3, 4, 5, or 6 packets) needed. Mixing the powder with food (e.g., applesauce, yogurt) is preferred; may mix with beverage (e.g., milk, infant formula, water) for infants able to drink from a cup. For infants <6 months of age not able to eat solid food or drink from a cup, mix with infant formula and administer using oral dosing syringe. Administration with infant bottle not recommended since full dose may not be delivered.
Mixing with food: Tap packet to settle powder; cut packet along dotted line with clean scissors. Using a spoon, mix contents of recommended number of packets with ≥1 tablespoon of food (e.g., applesauce, yogurt) in a small container (e.g., cup, bowl); feed mixture to patient. Add and mix additional 1 tablespoon of food to the small container; feed residual mixture to patient.
Mixing with a beverage: Tap packet to settle powder; cut packet along dotted line with clean scissors. Using a spoon, mix contents of recommended number of packets in a small drinking cup with ≥30 mL of beverage; give mixture to patient to drink. Add and mix additional 15 mL of beverage to drinking cup; give residual mixture to patient to drink. If water is used as the beverage, patient also should eat food at time of administration.
Mixing with liquid infant formula: Tap packet to settle powder; cut packet along dotted line with clean scissors. Using a spoon, mix contents of recommended number of packets in a small medicine cup with 10 mL of prepared liquid infant formula. Draw entire mixture into oral dosing syringe and administer into infant's right or left inner cheek. Pour and mix additional 10 mL of infant formula into medicine cup to rinse off any remaining powder. Draw residual mixture into oral dosing syringe and administer into infant's right or left inner cheek.
Administer entire dose within 1 hour after mixing with food or beverage; may be left at room temperature (20–30°C) for up to 1 hour after mixing. For additional information on mixing and administering the oral powder, refer to the full instructions for use provided by the manufacturer.
Fixed Combinations Containing Atazanavir
Atazanavir also commercially available in a fixed-combination preparation containing atazanavir and cobicistat (atazanavir/cobicistat; Evotaz). Refer to the full prescribing information for administration of the combination product.
Dosage
Available as capsules or oral powder containing atazanavir sulfate; dosage expressed in terms of atazanavir.
Pediatric Patients
Dosage change may be required when transitioning between formulations; refer to the dosage table for the specific formulation.
Treatment of HIV Infection
Antiretroviral-naïve or Antiretroviral-experienced Pediatric Patients
OralPediatric patients ≥3 months of age weighing ≥5 kg (oral powder): Dosage is based on weight. (See Table 1.) Oral powder must be used with low-dose ritonavir (ritonavir-boosted atazanavir); administer ritonavir immediately after atazanavir powder.
Recommendations regarding the timing and maximum doses of concomitant proton pump inhibitors and histamine H2-receptor antagonists in adults also apply to pediatric patients In patients weighing 5 to <10 kg who do not tolerate 200 mg (4 packets) of atazanavir oral powder and have not previously received an HIV PI, atazanavir oral powder in a dosage of 150 mg (3 packets) once daily may be used with close HIV viral load monitoring.
|
Body Weight |
Atazanavir Dosage (Oral Powder) |
Ritonavir Dosage (Oral Solution) |
|---|---|---|
|
5 to <15 kg |
200 mg (4 packets) once daily |
80 mg once daily |
|
15 to <25 kg |
250 mg (5 packets) once daily |
80 mg once daily |
|
≥25 kg and not able to swallow capsules |
300 mg (6 packets) once daily |
100 mg once daily |
Pediatric patients 6 to <18 years of age (capsules): Dosage is based on weight. (See Table 2.) Capsules usually used with low-dose ritonavir (ritonavir-boosted atazanavir); administer atazanavir capsules and ritonavir simultaneously with food.
Recommendations regarding the timing and maximum doses of concomitant proton pump inhibitors and histamine H2-receptor antagonists in adults also apply to pediatric patients.
In antiretroviral-experienced patients, administer atazanavir capsules with ritonavir.
|
Body Weight |
Atazanavir Dosage (Capsules) |
Ritonavir Dosage |
|---|---|---|
|
<15 kg |
Capsules not recommended |
|
|
≥15 to <35 kg |
200 mg once daily |
100 mg once daily |
|
≥35 kg |
300 mg once daily |
100 mg once daily |
Unboosted atazanavir (i.e., without low-dose ritonavir or cobicistat) in antiretroviral-naïve adolescents ≥13 years of age weighing ≥40 kg unable to tolerate ritonavir: 400 mg once daily.
The fixed-combination preparation containing atazanavir and cobicistat (atazanavir/cobicistat; Evotaz) is also used for the treatment of HIV-1 infection in pediatric patients; refer to the full prescribing information for dosage of atazanavir/cobicistat in pediatric patients.
Adults
Treatment of HIV Infection
Antiretroviral-naïve Adults
OralRitonavir-boosted atazanavir: Atazanavir 300 mg once daily in conjunction with ritonavir 100 mg once daily.
Unboosted atazanavir (adults unable to tolerate ritonavir): 400 mg once daily.
Ritonavir-boosted atazanavir in combination with efavirenz: Atazanavir 400 mg once daily in conjunction with ritonavir 100 mg once daily.
Antiretroviral-experienced Adults
OralRitonavir-boosted atazanavir: Atazanavir 300 mg once daily in conjunction with ritonavir 100 mg once daily.
Ritonavir-boosted atazanavir in combination with histamine H2-receptor antagonist and tenofovir disoproxil fumarate (tenofovir DF): Atazanavir 400 mg once daily given in conjunction with ritonavir 100 mg once daily.
Do not use atazanavir without ritonavir in treatment-experienced adults.
The fixed-combination preparation containing atazanavir and cobicistat (atazanavir/cobicistat; Evotaz) is also used for the treatment of HIV-1 infection in adults; refer to the full prescribing information for dosage of atazanavir/cobicistat in adults.
Postexposure Prophylaxis following Occupational Exposure to HIV (PEP)† [off-label]
Oral
Ritonavir-boosted atazanavir: Atazanavir 300 mg once daily in conjunction with ritonavir 100 mg once daily. Alternatively, atazanavir 400 mg once daily can be used without ritonavir, but not in combination with tenofovir DF.
Initiate PEP as soon as possible following occupational exposure to HIV (preferably within hours); continue for 4 weeks, if tolerated.
Special Populations
Hepatic Impairment
Unboosted atazanavir in treatment-naïve adults with mild hepatic impairment (Child-Pugh class A): 400 mg once daily.
Unboosted atazanavir in treatment-naïve adults with moderate hepatic impairment (Child-Pugh class B): 300 mg once daily.
Unboosted atazanavir in patients with severe hepatic impairment (Child-Pugh class C): Do not use.
Ritonavir-boosted atazanavir: Do not use in patients with any degree of hepatic impairment.
Renal Impairment
Ritonavir-boosted or unboosted atazanavir in patients with renal impairment not undergoing hemodialysis: Dosage adjustments not needed.
Ritonavir-boosted atazanavir in antiretroviral-naïve adults with end-stage renal disease undergoing hemodialysis: 300 mg once daily with ritonavir 100 mg once daily.
Antiretroviral-experienced adults with end-stage renal disease undergoing hemodialysis: Do not use ritonavir-boosted or unboosted atazanavir.
Geriatric Use
No specific dosage recommendations at this time. Exercise caution in administration and monitoring because of age-related decrease in hepatic, renal, and/or cardiac function and concomitant disease and drug therapy.
Pregnant and Postpartum Women
Use ritonavir-boosted atazanavir; do not use unboosted atazanavir. No dosage adjustments are necessary for postpartum patients; monitor closely for adverse effects, especially during first 2 months after delivery.
Ritonavir-boosted atazanavir in antiretroviral-naïve or antiretroviral-experienced pregnant patients: recommended dosage is atazanavir 300 mg once daily given in conjunction with ritonavir 100 mg once daily.
Ritonavir-boosted atazanavir in antiretroviral-experienced pregnant women in second or third trimester also receiving either a histamine H2-receptor antagonist or tenofovir DF: Increase atazanavir dosage to 400 mg once daily with ritonavir 100 mg once daily. Not recommended in antiretroviral-experienced pregnant women receiving both a histamine H2-receptor antagonist and tenofovir DF.
Cautions for Atazanavir Sulfate
Contraindications
-
History of clinically important hypersensitivity reaction (e.g., Stevens-Johnson syndrome, erythema multiforme, toxic skin eruptions) to atazanavir sulfate or any ingredient in the formulation.
-
Concomitant use with drugs that are highly dependent on CYP3A or uridine diphosphate-glucuronosyltransferase (UGT) 1A1 for clearance and for which elevated plasma concentrations are associated with serious and/or life-threatening events (see list below).
-
Concomitant use with drugs that are strong inducers of CYP3A when such use may lead to decreased atazanavir exposures resulting in possible loss of virologic response (see list below).
-
The following drugs are contraindicated with atazanavir (with or without ritonavir, unless otherwise noted): alfuzosin, amiodarone (with ritonavir), carbamazepine, phenobarbital, phenytoin, quinidine (with ritonavir), rifampin, apalutamide, encorafenib, irinotecan, ivosidenib, lurasidone (with ritonavir), pimozide, oral triazolam, oral midazolam, dihydroergotamine, ergotamine, ergonovine, methylergonovine, cisapride, elbasvir/grazoprevir, glecaprevir/pibrentasvir, St. John’s wort (Hypericum perforatum), lovastatin, simvastatin, lomitapide, sildenafil for the treatment of pulmonary arterial hypertension (Revatio), indinavir, and nevirapine.
Warnings/Precautions
Severe Dermatologic Reactions
Rash (all grades, regardless of causality) reported frequently. Median time to onset 7.3 weeks; median duration 1.4 weeks. Generally mild-to-moderate maculopapular skin eruptions. Stevens-Johnson syndrome, erythema multiforme, and toxic skin eruptions, including drug rash with eosinophilia and systemic symptoms (DRESS) syndrome, reported.
Discontinue in patients who develop severe rash.
Cardiac Conduction Abnormalities
Abnormalities in AV conduction (including prolongation of PR interval) reported. Cardiac conduction abnormalities generally are asymptomatic and limited to first-degree AV block.
Because of limited clinical experience in patients with preexisting cardiac conduction abnormalities (e.g., marked first-degree AV block; second- or third-degree AV block), consider ECG monitoring in such patients.
Chronic Kidney Disease
Chronic kidney disease reported in postmarketing experience in patients with HIV-1 infection treated with atazanavir (with or without ritonavir). Reports included granulomatous interstitial nephritis (proven by biopsy) associated with the deposition of atazanavir drug crystals in the renal parenchyma.
Consider alternatives in patients at high risk for renal disease or with preexisting renal disease. Perform renal laboratory testing (including Scr, estimated Clcr, and urinalysis with microscopic examination) in all patients prior to and during treatment. Expert consultation advised for patients with confirmed renal laboratory abnormalities during therapy. Consider discontinuation in patients with progressive kidney disease.
Hyperbilirubinemia
Reversible, asymptomatic elevations in indirect (unconjugated) bilirubin occur in most patients since atazanavir is a competitive inhibitor of UGT 1A1 (an enzyme that catalyzes glucuronidation of bilirubin).
Assess hepatic transaminase elevations that occur with hyperbilirubinemia for alternative etiologies.
Long-term safety data not available for patients with persistent elevations in total bilirubin >5 times ULN.
If jaundice or scleral icterus resulting from elevated bilirubin causes cosmetic concerns, can consider alternative antiretroviral; reduction of atazanavir dosage not recommended since efficacy data not available.
Phenylketonuria
Advise individuals with phenylketonuria that atazanavir oral powder contains phenylalanine (component of aspartame).
Each packet of oral powder (50 mg of atazanavir) contains 35 mg of phenylalanine. Atazanavir capsules do not contain phenylalanine.
Hepatotoxicity
Risk of further transaminase elevations or hepatic decompensation in HIV-infected patients with HBV or HCV coinfection or elevated hepatic enzymes prior to initiation of atazanavir. Evaluate hepatic function prior to and during atazanavir treatment in these patients.
Nephrolithiasis and Cholelithiasis
Postmarketing reports of nephrolithiasis and cholelithiasis; some patients required hospitalization for additional management or experienced complications.
If nephrolithiasis or cholelithiasis occurs, consider temporary interruption or discontinuation of atazanavir.
Drug Interactions
When ritonavir-boosted atazanavir is used, consider the cautions, precautions, contraindications, and drug interactions associated with atazanavir and ritonavir.
Ritonavir is a CYP3A inhibitor; initiation of ritonavir-boosted atazanavir in patients receiving drugs metabolized by CYP3A or initiation of drugs metabolized by CYP3A in patients already receiving ritonavir-boosted atazanavir, may increase plasma concentrations of the drugs metabolized by CYP3A. Initiation of drugs that inhibit or induce CYP3A may increase or decrease concentrations of ritonavir-boosted atazanavir, respectively.
Interactions with ritonavir-boosted atazanavir resulting in greater exposures of concomitant medications may lead to clinically important adverse effects (including severe, life-threatening, or fatal events). Some interactions may result in clinically important adverse effects due to greater exposures to ritonavir-boosted atazanavir or loss of therapeutic effect of ritonavir-boosted atazanavir and development of resistance.
Consider potential drug interactions prior to and during use of ritonavir-boosted atazanavir. Monitor for adverse effects associated with drugs used concomitantly with ritonavir-boosted atazanavir.
Additional drug interactions may exist for the fixed-dose combination of atazanavir and cobicistat (Evotaz). See the full prescribing information for drug interactions of this combination product.
Hyperglycemic and Diabetogenic Effects
Hyperglycemia (potentially persistent), new-onset diabetes mellitus, or exacerbation of preexisting diabetes mellitus reported with HIV PIs; diabetic ketoacidosis has also occurred.
Initiate or adjust antidiabetic therapy (e.g., insulin, oral hypoglycemic agents) as needed. Causal relationship not established.
Immune Reconstitution Syndrome
During initial treatment, patients who respond to antiretroviral therapy may develop an inflammatory response to indolent or residual opportunistic infections (e.g., Mycobacterium avium complex, M. tuberculosis, cytomegalovirus, Pneumocystis jirovecii); this may necessitate further evaluation and treatment.
Autoimmune disorders (e.g., Graves' disease, polymyositis, Guillain-Barré syndrome) also reported to occur in the setting of immune reconstitution; time to onset is more variable and can occur many months after initiation of antiretroviral therapy.
Fat Redistribution
Possible redistribution or accumulation of body fat, including central obesity, dorsocervical fat enlargement (“buffalo hump”), peripheral wasting, facial wasting, breast enlargement, and general cushingoid appearance.
Mechanisms and long-term consequences of adipogenic effects unknown; causal relationship not established.
Hemophilia A and B
Increased bleeding, including spontaneous hematomas and hemarthrosis, reported with HIV PIs; causal relationship not established.
Increased hemostatic (e.g., antihemophilic factor) therapy may be needed in some cases; causal relationship not established.
HIV Resistance
Possibility of HIV-1 resistant to atazanavir.
Varying degrees of cross-resistance occur among the various HIV PIs. Resistance to atazanavir may not preclude subsequent use of other HIV PIs.
Specific Populations
Pregnancy
Antiretroviral Pregnancy Registry (APR) at 800-258-4263 or [Web].
Available animal and human data to date indicate that atazanavir does not increase risk of major birth defects overall compared to background rate. No treatment-related malformations observed in rats and rabbits at atazanavir exposures 0.7–1.2 times those reported with usual human dosage of ritonavir-boosted atazanavir (300 mg of atazanavir once daily with ritonavir 100 mg once daily). Based on prospective reports from the APR of approximately 1600 live births following exposure to atazanavir, no difference observed in rate of overall birth defects in those exposed to atazanavir compared with the estimated background risk of major birth defects.
Lactic acidosis, sometimes fatal, and symptomatic hyperlactatemia reported in pregnant women patients receiving atazanavir in conjunction with NRTIs. Hyperbilirubinemia reported in pregnant women receiving atazanavir. Advise pregnant patients of potential risks of lactic acidosis syndrome and hyperbilirubinemia.
Monitor postpartum women closely for adverse effects during first 2 months after delivery; atazanavir concentrations and AUC may be increased during postpartum period.
Lactation
Distributed into human milk. Unknown whether atazanavir affects human milk production.
Distributed into milk in rats; associated with neonatal growth retardation that reversed after weaning.
The HHS perinatal HIV transmission guideline provides updated recommendations on infant feeding. The guideline states that patients with HIV should receive evidence-based, patient-centered counseling to support shared decision making about infant feeding. During counseling, patients should be informed that feeding with appropriate formula or pasteurized donor human milk from a milk bank eliminates the risk of postnatal HIV transmission to the infant. Additionally, achieving and maintaining viral suppression with antiretroviral therapy during pregnancy and postpartum reduces the risk of breastfeeding HIV transmission to <1%, but does not completely eliminate the risk. Replacement feeding with formula or banked pasteurized donor milk is recommended when patients with HIV are not on antiretroviral therapy and/or do not have a suppressed viral load during pregnancy (at a minimum throughout the third trimester), as well as at delivery.
Pediatric Use
Ritonavir-boosted or unboosted atazanavir: Do not use in neonates and infants <3 months of age because of risk of kernicterus. Safety, efficacy, and pharmacokinetic profile not established in infants <3 months of age. All contraindications, warnings, and precautions of atazanavir apply to pediatric patients.
Ritonavir-boosted or unboosted atazanavir: Safety, efficacy, and pharmacokinetic profile evaluated in pediatric patients ≥3 months of age weighing ≥5 kg. Adverse effects in children 6 years to <18 years of age receiving the capsules generally similar to those reported in adults; adverse effects in pediatric patients weighing ≥5 kg receiving the oral powder generally similar to those reported in pediatric patients receiving capsules.
Geriatric Use
Insufficient experience in patients ≥65 years of age to determine whether they respond differently than younger adults. Use with caution and monitor because of age-related decreases in hepatic, renal, and/or cardiac function and concomitant disease and drug therapy.
Hepatic Impairment
Atazanavir principally metabolized and eliminated by the liver; increased plasma atazanavir concentrations expected in patients with moderate to severe hepatic impairment.
Unboosted atazanavir: Dosage adjustments recommended in those with mild or moderate hepatic impairment (Child-Pugh class A or B). Do not use in those with severe hepatic impairment (Child-Pugh class C).
Ritonavir-boosted atazanavir: Do not use in those with any degree of hepatic impairment.
HIV-infected patients with HBV or HCV coinfection and those with marked increases in AST or ALT prior to atazanavir therapy may be at increased risk for further elevations in hepatic enzymes or for hepatic decompensation.
Renal Impairment
Plasma concentrations of atazanavir in individuals with severe renal impairment not undergoing dialysis generally are similar to those in individuals with normal renal function. Dosage adjustments not needed.
Ritonavir-boosted atazanavir can be used in antiretroviral-naïve patients with end-stage renal disease who are undergoing hemodialysis.
Use of ritonavir-boosted or unboosted atazanavir is not recommended in antiretroviral-experienced patients with end-stage renal disease undergoing hemodialysis.
Pharmacogenomic Considerations
Atazanavir is a competitive inhibitor of UGT1A1; atazanavir prescribing is guided by UGT1A1 genotype testing and interpretation. In patients who are poor metabolizers of UGT1A1, consider an alternative agent to ritonavir-boosted atazanavir particularly if there are concerns of jaundice.
Refer to the Clinical Pharmacogenetics Implementation Consortium (CPIC) guideline for additional information.
Common Adverse Effects
Most common adverse effects (≥2%): headache, nausea, jaundice/scleral icterus, abdominal pain, rash, vomiting, diarrhea, insomnia, peripheral neurologic symptoms, dizziness, myalgia, depression, fever.
Drug Interactions
When atazanavir is used with ritonavir, consider drug interactions associated with both atazanavir and ritonavir. The following drug interactions are based on studies using ritonavir-boosted or unboosted atazanavir.
Additional drug interactions may exist for the fixed-dose combination of atazanavir and cobicistat (Evotaz); see the full prescribing information for drug interactions of this combination product.
Drugs Affecting or Metabolized by Hepatic Microsomal Enzymes
CYP3A inducers: Potential pharmacokinetic interactions with ritonavir-boosted and unboosted atazanavir (increased clearance of atazanavir and ritonavir; possible loss of antiretroviral efficacy and development of resistance to atazanavir).
CYP3A inhibitors: Potential pharmacokinetic interactions with ritonavir-boosted and unboosted atazanavir (increased plasma concentrations of atazanavir or ritonavir).
CYP3A or 2C8 substrates: Potential pharmacokinetic interactions with ritonavir-boosted and unboosted atazanavir (altered metabolism of these substrates). Use of atazanavir without ritonavir is not recommended when coadministered with drugs that are highly dependent on CYP2C8 metabolism and have narrow therapeutic indices (e.g., paclitaxel, repaglinide). When ritonavir-boosted atazanavir is coadministered with substrates of CYP2C8, clinically significant interactions are not expected.
Atazanavir not expected to interact with CYP2C19, 2C9, 2D6, 2B6, 2A6, 1A2, or 2E1 substrates.
Drugs Metabolized by Uridine Diphosphate-glucoronosyltransferase 1A1
UGT1A1 substrates: Potential pharmacokinetic interactions with ritonavir-boosted and unboosted atazanavir.
Specific Drugs
|
Drug |
Interaction |
Comments |
|---|---|---|
|
Abacavir |
No in vitro evidence of antagonistic antiretroviral effects |
|
|
Acetaminophen |
Pharmacokinetic interactions unlikely |
|
|
Alfuzosin |
Possible increased alfuzosin concentrations; may result in hypotension |
Concomitant use with atazanavir contraindicated |
|
Amprenavir |
No in vitro evidence of antagonistic antiretroviral effects |
|
|
Antacids or buffered medications |
Possible decreased atazanavir concentrations |
Administer atazanavir 2 hours before or 1 hour after antacids or buffered medications |
|
Antiarrhythmic agents (amiodarone, bepridil, systemic lidocaine, quinidine) |
Possible increased antiarrhythmic agent concentrations Potential for serious or life-threatening effects (e.g., cardiac arrhythmias) |
Amiodarone, quinidine: Concomitant use with ritonavir-boosted atazanavir contraindicated Bepridil, systemic lidocaine; exercise caution; monitor concentrations of the antiarrhythmic drug if used concomitantly with atazanavir |
|
Anticoagulants (apixaban, dabigatran, edoxaban, rivaroxaban, warfarin) |
Apixaban, dabigatran, edoxaban, rivaroxaban: Increased exposure of the anticoagulant and increased risk of bleeding Warfarin: Increased plasma concentrations of warfarin and potential for serious and/or life-threatening bleeding |
Apixaban: Refer to the full prescribing information of apixaban for specific dosing recommendations if used concomitantly with ritonavir-boosted atazanavir; monitor closely when apixaban is used concomitantly with atazanavir without ritonavir Dabigatran, edoxaban, rivaroxaban: Refer to the full prescribing information of the anticoagulant for specific dosing recommendations Rivaroxaban: Concomitant use of ritonavir-boostedatazanavir and rivaroxaban not recommended; monitor patients closely when rivaroxaban is used concomitantly with atazanavir (without ritonavir) Warfarin: Monitor INR |
|
Anticonvulsants (carbamazepine, lamotrigine, phenobarbital, phenytoin) |
Carbamazepine: Possible decreased atazanavir concentrations and increased carbamazepine concentrations if used with ritonavir-boosted atazanavir; decreased atazanavir concentrations if used with unboosted atazanavir Lamotrigine: Concomitant use of ritonavir-boosted atazanavir and lamotrigine decreases lamotrigine plasma concentrations Phenobarbital, phenytoin: Concomitant use of unboosted atazanavir and phenobarbital or phenytoin may decrease plasma concentrations of atazanavir; concomitant use of ritonavir-boosted atazanavir and phenobarbital or phenytoin may decrease plasma concentrations or atazanavir and the anticonvulsant |
Carbamazepine: Concomitant use of unboosted atazanavir and carbamazepine not recommended; if ritonavir-boosted atazanavir is initiated in a patient already receiving a stable carbamazepine dosage, carbamazepine dosage reduction may be needed Lamotrigine: Dosage adjustments not needed if lamotrigine is used concomitantly with unboosted atazanavir; concomitant use of ritonavir-boosted atazanavir and lamotrigine may require lamotrigine dosage adjustment Phenobarbital, phenytoin: Concomitant use of unboosted atazanavir and phenobarbital or phenytoin not recommended; if ritonavir-boosted atazanavir is used concomitantly with phenobarbital or phenytoin, adjustment of the anticonvulsant dosage may be needed |
|
Antifungals, azoles (fluconazole, itraconazole, ketoconazole, voriconazole) |
Fluconazole: No clinically important pharmacokinetic interactions Itraconazole, ketoconazole: Possible increased antifungal concentrations if concomitantly used with ritonavir-boosted atazanavir Voriconazole: Use with ritonavir-boosted atazanavir results in decreased atazanavir and voriconazole plasma concentrations in patients with a functional CYP2C19 allele; decreased atazanavir concentrations and increased voriconazole concentrations in patients without a functional CYP2C19 allele. Coadministration of voriconazole and atazanavir without ritonavir may affect atazanavir concentrations; however, no data are available. |
Itraconazole, ketoconazole: Caution advised if ketoconazole or itraconazole dosage >200 mg daily used with ritonavir-boosted atazanavir Voriconazole: Do not use with ritonavir-boosted atazanavir unless potential benefits outweigh risks; monitor for voriconazole-associated adverse effects and loss of voriconazole or atazanavir efficacy |
|
Antimycobacterials (rifabutin, rifampin) |
Rifabutin: Increased concentrations of rifabutin if used with ritonavir-boosted or unboosted atazanavir Rifampin: Substantially decreased atazanavir concentrations; possible decreased antiretroviral efficacy and increased risk of antiretroviral resistance |
Rifabutin: May reduce rifabutin dosage up to 75% (e.g., 150 mg once every other day or 3 times weekly); increased monitoring for rifabutin-associated adverse effects (e.g., neutropenia) warranted Rifampin: Concomitant use contraindicated |
|
Antineoplastic agents (apalutamide, irinotecan, ivosidenib, paclitaxel) |
Apalutamide: Potential for subsequent loss of virologic response and possible resistance to the class of protease inhibitors Irinotecan: Atazanavir may interfere with metabolism of irinotecan leading to increased irinotecan toxicity Ivosidenib: Potential loss of virologic response and serious adverse events such as QT prolongation Paclitaxel: Possible increased paclitaxel concentrations if used with unboosted atazanavir; clinically important interactions not expected if used with ritonavir-boosted atazanavir |
Apalutamide: Concomitant use contraindicated Irinotecan: Concomitant use contraindicated Ivosidenib: Concomitant use contraindicated Paclitaxel: Concomitant use with unboosted atazanavir not recommended |
|
Antiplatelet agents (clopidogrel, ticagrelor) |
Clopidogrel: Potential reduction of antiplatelet activity of clopidogrel Ticagrelor: Potential increase in risk of dyspnea, bleeding, and other adverse events associated with ticagrelor |
Clopidogrel: Concomitant use not recommended Ticagrelor: Concomitant use not recommended |
|
Antipsychotics (lurasidone, pimozide, quetiapine) |
Lurasidone: Possible increased lurasidone concentrations; potential for serious and/or life-threatening adverse effects if used concomitantly with ritonavir-boosted atazanavir Pimozide: Increased pimozide concentrations; potential for serious and/or life-threatening effects (e.g., cardiac arrhythmias) Quetiapine: Increased quetiapine concentrations expected |
Lurasidone: Concomitant use with ritonavir-boosted atazanavir contraindicated; if concomitant use with unboosted atazanavir necessary, reduce lurasidone dosage Pimozide: Concomitant use contraindicated Quetiapine: If possible, consider alternative antiretroviral therapy to avoid increases in quetiapine exposures; if initiating ritonavir-boosted atazanavir in patient receiving quetiapine, reduce quetiapine to one-sixth of original dosage and monitor for adverse effects of quetiapine; if quetiapine is initiated in a patient receiving ritonavir-boosted atazanavir, refer to quetiapine prescribing information for initial dosage and titration |
|
Atenolol |
No clinically important pharmacokinetic interactions |
|
|
Azithromycin |
Clinically important interactions unlikely |
|
|
Benzodiazepines (midazolam, triazolam) |
Midazolam or triazolam: Possible increased concentrations of midazolam or triazolam and potential for serious and/or life- threatening effects (e.g., prolonged or increased sedation or respiratory depression) |
Oral midazolam or triazolam: Concomitant use contraindicated Parenteral midazolam: Use with caution and in a monitored setting where respiratory depression and/or prolonged sedation can be managed; consider reduced dosage of midazolam, especially if more than a single dose of midazolam given |
|
Bosentan |
Ritonavir-boosted or unboosted atazanavir: Possible decreased atazanavir concentrations |
In patients already receiving ritonavir-boosted atazanavir for ≥10 days, initiate bosentan using a dosage of 62.5 mg once daily or every other day based on individual tolerability In patients already receiving bosentan, discontinue bosentan for ≥36 hours prior to initiating ritonavir-boosted atazanavir; after ≥10 days of ritonavir-boosted atazanavir, resume bosentan at a dosage of 62.5 mg once daily or every other day based on individual tolerability Unboosted atazanavir: concomitant use with bosentan is not recommended |
|
Buprenorphine |
Increased buprenorphine and norbuprenorphine concentrations; when used with unboosted atazanavir, decreased atazanavir concentrations also possible |
Unboosted atazanavir: Concomitant use with buprenorphine not recommended Ritonavir-boosted atazanavir: Monitor for sedation and adverse cognitive effects; consider reduced buprenorphine dosage |
|
Calcium-channel blocking agents (diltiazem, felodipine, nifedipine, nicardipine, verapamil) |
Possible increased concentrations of calcium-channel blocking agent |
Felodipine, nifedipine, nicardipine, verapamil: Use with caution; consider dose titration of calcium-channel blocking agent; ECG monitoring recommended Diltiazem: Consider 50% reduction in diltiazem dosage; use concomitantly with caution; ECG monitoring recommended |
|
Cisapride |
Possible increased cisapride concentrations; potential for serious and/or life-threatening effects (e.g., cardiac arrhythmias) |
Concomitant use contraindicated |
|
Clarithromycin |
Increased concentrations of atazanavir, increased clarithromycin concentrations, decreased 14-hydroxyclarithromycin concentrations; increased clarithromycin concentrations may cause QTc prolongation |
Consider reducing clarithromycin dosage by 50%; consider alternative anti-infective for indications other than infections due to Mycobacterium avium complex |
|
Colchicine |
Increased colchicine concentrations |
Patients with renal or hepatic impairment: Concomitant use of colchicine and atazanavir not recommended Colchicine for treatment of gout flares: Use initial colchicine dose of 0.6 mg followed by 0.3 mg 1 hour later and repeat dose no earlier than 3 days later Colchicine for prophylaxis of gout flares: In those receiving ritonavir-boostedatazanavir, decrease colchicine dosage to 0.3 mg once daily in those originally receiving 0.6 mg twice daily or decrease dosage to 0.3 mg once every other day in those originally receiving 0.6 once daily Colchicine for treatment of familial Mediterranean fever (FMF): Use maximum colchicine dosage of 0.6 mg daily (may be given as 0.3 mg twice daily) |
|
Corticosteroids |
Coadministration with dexamethasone or other corticosteroids that induce CYP3A may result in loss of therapeutic effect of atazanavir and resistance development |
Consider alternative corticosteroids; long-term concomitant use may increase risk of adverse effects including Cushing's syndrome and adrenal suppression |
|
Co-trimoxazole |
Clinically important interactions unlikely |
|
|
Dapsone |
Clinically important interactions unlikely |
|
|
Delavirdine |
No in vitro evidence of antagonistic antiretroviral effects |
|
|
Didanosine |
Buffered didanosine: Decreased atazanavir concentrations and AUC Didanosine delayed-release capsules: Decreased didanosine concentrations and AUC if given with atazanavir and food No in vitro evidence of antagonistic antiretroviral effects |
Buffered didanosine: Administer atazanavir (with food) 2 hours before or 1 hour after buffered didanosine preparations Didanosine delayed-release capsules: Administer didanosine capsules and atazanavir at different times |
|
Efavirenz |
Decreased atazanavir concentrations and AUC No in vitro evidence of antagonistic antiretroviral effects with atazanavir |
Ritonavir-boosted atazanavir in antiretroviral-naïve adults: Use atazanavir 400 mg and ritonavir 100 mg once daily (with food) and efavirenz 600 mg once daily (without food, preferably at bedtime) Ritonavir-boosted atazanavir in antiretroviral-experienced adults: Concomitant use not recommended |
|
Emtricitabine |
No in vitro evidence of antagonistic antiretroviral effects |
|
|
Enfuvirtide |
No in vitro evidence of antagonistic antiretroviral effects |
|
|
Ergot derivatives (dihydroergotamine, ergonovine, ergotamine, methylergonovine) |
Possible increased concentrations of ergot derivatives and potential for serious and/or life-threatening effects such as ergot toxicity (e.g., peripheral vasospasm, ischemia of the extremities and other tissues) |
Concomitant use contraindicated |
|
Erythromycin |
Clinically important interactions unlikely |
|
|
Elbasvir and grazoprevir (elbasvir/grazoprevir) |
Increased grazoprevir concentrations and thus increased risk of ALT elevations |
Concomitant use contraindicated |
|
Estrogens/progestins |
Hormonal contraceptive containing ethinyl estradiol and norgestimate or norethindrone: Increased or decreased plasma concentrations of ethinyl estradiol; increased plasma concentrations of the progestin |
Use with caution Ritonavir-boosted atazanavir: Use an oral contraceptive containing ≥35 mcg of ethinyl estradiol Unboosted atazanavir: Use an oral contraceptive containing no more than 30 mcg of ethinyl estradiol Data not available for other hormonal contraceptives: Alternative methods of contraception recommended |
|
Fluticasone (orally inhaled, intranasal) |
Increased fluticasone concentrations; adrenal insufficiency and Cushing's syndrome reported |
Ritonavir-boosted atazanavir: Do not use concomitantly unless potential benefits outweigh risks of systemic corticosteroid adverse effects; consider alternative especially when long-term corticosteroid use anticipated Unboosted atazanavir: Use with caution; consider alternatives, especially when long-term use of the corticosteroid anticipated |
|
Glecaprevir and pibrentasvir (glecaprevir/pibrentasvir) |
Increased glecaprevir and pibrentasvir concentrations, and thus increased risk of ALT elevations |
Concomitant use contraindicated |
|
GnRH antagonists (elagolix) |
Elagolix: Potential loss of virologic response and risk of adverse events such as bone loss and hepatic transaminase elevations |
Elagolix: If necessary, limit concomitant use of elagolix 200 mg twice daily with atazanavir for up to 1 month or limit concomitant use of elagolix 150 mg once daily with atazanavir for up to 6 months and monitor virologic response |
|
Histamine H2-receptor antagonists |
Famotidine: Decrease in plasma concentrations of atazanavir; possible loss of the therapeutic effect of the antiretroviral agent and development of resistance |
Ritonavir-boosted atazanavir in antiretroviral-naïve adults: Administer atazanavir 300 mg once daily with ritonavir 100 mg once daily with food simultaneously with and/or ≥10 hours after the histamine H2-receptor antagonist; dosage of histamine H2-receptor antagonist should not exceed famotidine 40 mg twice daily (or equivalent) Unboosted atazanavir in antiretroviral-naïve adults: Administer atazanavir 400 mg once daily ≥2 hours before and ≥10 hours after the histamine H2-receptor antagonist; dosage of the histamine H2-receptor antagonist should not exceed famotidine 40 mg daily (or equivalent) and single doses should not exceed famotidine 20 mg (or equivalent) Antiretroviral-experienced patients receiving ritonavir-boosted atazanavir: Administer atazanavir 300 mg once daily with ritonavir 100 mg once daily with food simultaneously with and/or ≥10 hours after the histamine H2-receptor antagonist; dosage of histamine H2-receptor antagonist should not exceed famotidine 20 mg twice daily (or equivalent) Antiretroviral-experienced patients receiving tenofovir disoproxil fumarate (DF) and a histamine H2-receptor antagonist: Regimen of atazanavir 400 mg, tenofovir DF 300 mg, and ritonavir 100 mg once daily with food recommended Antiretroviral-experienced pregnant patients in second or third trimester receiving ritonavir-boosted atazanavir and a histamine H2-receptor antagonist: Adjust dosage of atazanavir to 400 mg once daily with ritonavir 100 mg once daily; dosage recommendations not available for antiretroviral-experienced pregnant patients receiving atazanavir and both tenofovir DF and a histamine H2-receptor antagonist |
|
HMG-CoA reductase inhibitors (statins) |
Atorvastatin, lovastatin, rosuvastatin, simvastatin: Increased concentrations of the statin; increased risk of statin-associated adverse effects, including myopathy and rhabdomyolysis |
Atorvastatin: Carefully titrate atorvastatin dosage; use lowest necessary dosage Lovastatin: Concomitant use contraindicated Rosuvastatin: Rosuvastatin dosage should not exceed 10 mg daily; titrate rosuvastatin dosage carefully and use the lowest necessary dosage Simvastatin: Concomitant use contraindicated |
|
Immunosuppressive agents (cyclosporine, sirolimus, tacrolimus) |
Increased concentrations of immunosuppressive agent |
Monitor immunosuppressive agent concentrations |
|
Indinavir |
Potential for additive hyperbilirubinemia No in vitro evidence of antagonistic antiretroviral effects |
Concomitant use contraindicated |
|
Kinase inhibitors (fostamatinib) |
Fostamatinib: Monitor for R406 exposure resulting in dose-related adverse events such as hepatotoxicity and neutropenia |
Fostamatinib: Dose reduction may be required |
|
Lamivudine |
No clinically important interactions No in vitro evidence of antagonistic antiretroviral effects |
|
|
Lomitapide |
Increased lomitapide concentrations |
Concomitant use contraindicated (potential for hepatotoxicity and significantly increased transaminases) |
|
Lopinavir |
No in vitro evidence of antagonistic antiretroviral effects |
|
|
Methadone |
Clinically significant pharmacokinetic interactions unlikely |
|
|
Nelfinavir |
No in vitro evidence of antagonistic antiretroviral effects |
|
|
Nevirapine |
Substantially decreased atazanavir plasma concentrations and AUC with possible loss of therapeutic effect and development of resistance; increased nevirapine plasma concentrations and AUC and increased risk of nevirapine-associated adverse effects No in vitro evidence of antagonistic antiretroviral effects |
Concomitant use contraindicated |
|
Proton-pump inhibitors (PPIs) |
Omeprazole: Substantially decreased atazanavir concentrations and possible loss of virologic response and development of atazanavir resistance |
Concomitant use with PPIs not recommended in antiretroviral-experienced patients Ritonavir-boosted atazanavir in antiretroviral-naïve adults receiving a PPI: Use regimen of atazanavir 300 mg once daily with ritonavir 100 mg once daily with food; administer the PPI approximately 12 hours before ritonavir-boosted atazanavir; dosage of PPI should not exceed omeprazole 20 mg daily (or equivalent) |
|
Repaglinide |
Possible increased repaglinide concentrations if used with unboosted atazanavir; clinically important interactions not expected if used with ritonavir-boosted atazanavir |
Concomitant use with unboosted atazanavir not recommended |
|
Ritonavir |
Increased atazanavir concentrations and AUC; low-dose ritonavir (100 mg once daily) used as a pharmacokinetic enhancer (pharmacokinetic booster) for therapeutic advantage (ritonavir-boosted atazanavir) No in vitro evidence of antagonistic antiretroviral effects |
Safety and efficacy of concomitant use of ritonavir dosages >100 mg once daily with atazanavir not established; such dosages not recommended Ritonavir-boosted atazanavir: Concomitant use with other HIV PIs not recommended |
|
Salmeterol |
Possible increased salmeterol concentrations and increased risk of salmeterol-associated adverse cardiovascular effects (e.g., QT interval prolongation, palpitations, and sinus tachycardia) |
Concomitant use not recommended |
|
Saquinavir |
Increased plasma concentrations of saquinavir possible No in vitro evidence of antagonistic antiretroviral effects |
Appropriate dosage for concomitant use with respect to safety and efficacy not established |
|
Sildenafil |
Possible increased sildenafil concentrations and increased risk of sildenafil-associated adverse effects (e.g., hypotension, syncope, visual disturbances, prolonged erection) |
Sildenafil (Revatio) for treatment of pulmonary arterial hypertension (PAH): Concomitant use contraindicated; safe and effective dose for concomitant use not established Sildenafil for treatment of erectile dysfunction: Use a reduced sildenafil dosage of 25 mg once every 48 hours and closely monitor for sildenafil-associated adverse effects (e.g., hypotension, syncope, visual disturbances, prolonged erection) |
|
St. John’s wort (Hypericum perforatum) |
Possible decreased atazanavir concentrations; possible decreased antiretroviral efficacy and increased risk of antiretroviral resistance \ |
Concomitant use contraindicated |
|
Tadalafil |
Possible increased tadalafil concentrations and increased risk of tadalafil-associated adverse effects (e.g., hypotension, syncope, visual disturbances, prolonged erection) |
If tadalafil (Adcirca) is indicated for treatment of PAH in patients who have been receiving atazanavir (with or without ritonavir) for ≥1 week, use initial tadalafil dosage of 20 mg once daily and, if tolerated, increase dosage to 40 mg once daily Avoid use of tadalafil (Adcirca) for treatment of PAH when starting atazanavir with or without ritonavir; discontinue tadalafil for ≥24 hours prior to initiating atazanavir; after ≥1 week of the antiretroviral agent, resume tadalafil at dosage of 20 mg once daily and, if tolerated, increase dosage to 40 mg once daily If tadalafil is used for treatment of erectile dysfunction in patients already receiving atazanavir, do not exceed tadalafil dosage of 10 mg once every 72 hours and closely monitor for tadalafil-related adverse effects (e.g., hypotension, syncope, visual disturbances, prolonged erection, syncope) |
|
Tenofovir DF |
Decreased atazanavir concentrations and AUC; increased tenofovir concentrations and AUC and possible increased risk of tenofovir-associated adverse effects, including renal disorders No in vitro evidence of antagonistic antiretroviral effects |
Unboosted atazanavir: Do not use concomitantly with tenofovir DF Ritonavir-boosted atazanavir: Use atazanavir 300 mg, ritonavir 100 mg, and tenofovir DF 300 mg once daily with food; monitor for tenofovir toxicity Ritonavir-boosted atazanavir used concomitantly with tenofovir and a histamine H2- receptor antagonist in antiretroviral-experienced adults: Use atazanavir 400 mg and ritonavir 100 mg, and tenofovir DF 300 mg once daily with food Antiretroviral-experienced pregnant women in second or third trimester receiving ritonavir-boosted atazanavir and either a histamine H2-receptor antagonist or tenofovir: Use atazanavir 400 mg and ritonavir 100 mg once daily with food Dosage recommendations not available for antiretroviral- experienced pregnant women receiving ritonavir-boosted atazanavir and both tenofovir DF and a histamine H2-receptor antagonist |
|
Trazodone |
Possible increased trazodone concentrations; adverse effects (nausea, dizziness, hypotension, syncope) reported when trazodone and ritonavir used concomitantly |
Use concomitantly with caution; consider using decreased trazodone dosage |
|
Tricyclic antidepressants |
Possible increased concentrations of the tricyclic antidepressant and potential for serious and/or life-threatening effects |
Monitor plasma concentrations of the tricyclic antidepressant |
|
Vardenafil |
Possible increased vardenafil concentrations and increased risk of vardenafil-associated adverse effects (e.g., hypotension, syncope, visual disturbances, prolonged erection) |
If ritonavir-boosted atazanavir is used in patients receiving vardenafil for treatment of erectile dysfunction, do not exceed vardenafil dosage of 2.5 mg once every 72 hours; if unboosted atazanavir is used in patients receiving vardenafil for treatment of erectile dysfunction, do not exceed vardenafil dosage of 2.5 mg once every 24 hours Use with caution; closely monitor for vardenafil-related adverse effects (e.g., hypotension, syncope, visual disturbances, prolonged erection, syncope) |
|
Voxilaprevir, sofosbuvir, and velpatasvir (voxilaprevir/sofosbuvir/velpatasvir) |
Increased voxilaprevir concentrations |
Concomitant use contraindicated |
|
Zidovudine |
No clinically important interactions |
No in vitro evidence of antagonistic antiretroviral effects |
Atazanavir Sulfate Pharmacokinetics
Absorption
Bioavailability
Unboosted atazanavir: Rapidly absorbed following oral administration; peak plasma concentrations attained approximately 2–2.5 hours after a dose.
Ritonavir-boosted atazanavir: Peak plasma concentrations attained approximately 2.7–3 hours after a dose.
Food
Food increases bioavailability and reduces pharmacokinetic variability.
Administration of unboosted atazanavir with a light meal increases peak plasma concentration by 57% and AUC by 70% compared with fasting. A high-fat meal increases AUC by 35% with no increase in peak plasma concentration.
Administration of ritonavir-boosted atazanavir with a light meal increases atazanavir peak plasma concentrations by 40% and AUC by 33% compared with fasting. A high-fat meal does not affect AUC compared with fasting.
Plasma Concentrations
Nonlinear pharmacokinetics with greater than dose-proportional increases in plasma concentrations and AUC.
Unboosted atazanavir: Steady-state concentrations attained between days 4–8 with an accumulation of approximately 2.3-fold.
Special Populations
Unboosted atazanavir in hepatic impairment: Following a single 400-mg dose of atazanavir, AUC increased 42% in adults with moderate to severe hepatic impairment (Child-Pugh class B and C) compared with healthy adults.
Unboosted atazanavir in renal impairment: Plasma concentrations in adults with severe renal impairment not undergoing dialysis generally are similar to those in adults with normal renal function. When administered before or after dialysis, plasma concentrations are lower than those in adults with normal renal function (mechanism of this change unknown).
Ritonavir-boosted atazanavir in postpartum women: Atazanavir steady-state peak plasma concentrations and AUC are approximately 28–43% higher during postpartum period (4–12 weeks) compared with historical data in HIV-infected, nonpregnant patients.
Distribution
Extent
Low concentrations of atazanavir attained in CSF and semen after oral administration.
Atazanavir distributed into fetal umbilical cord blood in low concentrations. When ritonavir-boosted atazanavir used in pregnant women, atazanavir concentrations in cord blood approximately 12–19% of maternal plasma concentrations at delivery.
Distributed into human milk.
Plasma Protein Binding
86% bound to serum proteins; binding independent of concentration.
Binds to both α-1-acid glycoprotein (89%) and albumin (86%).
Elimination
Metabolism
Extensively metabolized and eliminated in liver. CYP3A involved in metabolism of the drug.
Elimination Route
Approximately 79% of a dose eliminated in feces and 13% eliminated in urine as metabolites and unchanged drug.
In patients with severe renal impairment on hemodialysis, 2.1% of the administered dose of atazanavir was removed in a 4-hour dialysis session.
Half-life
Unboosted atazanavir: 6.5–7.9 hours.
Ritonavir-boosted atazanavir: 8.6–18.1 hours.
Special Populations
No clinically important differences in pharmacokinetics in those >65 years of age compared with younger adults.
Atazanavir: Half-life is 12.1 hours in those with moderate to severe hepatic impairment.
Stability
Storage
Oral
Capsules
25°C (excursions permitted between 15–30°C) in tightly closed container.
Powder
20-30°C in original packet. After mixing with food or beverage, may store for up to 1 hour at room temperature (20–30°C).
Actions and Spectrum
-
Active against HIV-1; has some in vitro activity against HIV-2.
-
Inhibits replication of HIV-1 by interfering with HIV protease.
-
Atazanavir may be administered with low-dose ritonavir (ritonavir-boosted atazanavir) or with cobicistat (cobicistat-boosted atazanavir) resulting in increased exposures to atazanavir.
-
Antiretroviral activity of ritonavir-boosted atazanavir or cobicistat-boosted atazanavir due to atazanavir.
-
HIV-1 with reduced susceptibility to atazanavir have been selected in vitro and have emerged during therapy with the drug.
-
Varying degrees of cross-resistance occur among HIV protease inhibitors.
Advice to Patients
-
Inform patients of the importance of compliance with human immunodeficiency virus (HIV) therapy and remaining under the care of a clinician. Advise patients to take the antiretroviral regimen as prescribed and not alter or discontinue the regimen without consulting a clinician.
-
Inform patients that atazanavir is used in conjunction with other antiretrovirals for the treatment of HIV infection.
-
Advise patients to take atazanavir with food daily and take other concomitant antiretroviral therapy as prescribed.
-
If a dose of atazanavir is missed, advise patients to take the dose as soon as it is remembered and take the next dose at the regularly scheduled time; if a dose is skipped, advise patients to not double the next dose.
-
If atazanavir oral powder is used, advise caregivers to carefully follow mixing and administration instructions provided by the manufacturer.
-
If atazanavir oral powder is used, advise caregivers of patients with phenylketonuria that atazanavir oral powder contains phenylalanine.
-
Advise patients that ECG changes (PR prolongation) have occurred during atazanavir therapy and to consult a clinician if dizziness or lightheadedness occurs.
-
Inform patients that asymptomatic increases in indirect bilirubin that may be accompanied by yellowing of the skin or whites of the eyes have occurred in patients receiving atazanavir; inform patients that alternative antiretroviral therapy can be considered after discussion with a clinician.
-
Inform patients that atazanavir therapy may lead to the development of chronic kidney disease, and to maintain adequate hydration during treatment.
-
Advise patients to inform their clinician immediately of any signs or symptoms of infection, because in some patients with advanced HIV infection, signs and symptoms of inflammation may occur soon after starting antiretroviral therapy.
-
Inform patients that redistribution/accumulation of body fat may occur with antiretroviral therapy, although, long-term health effects are unknown.
-
Advise patients that mild rash and severe skin reactions, including Stevens-Johnson syndrome, erythema multiforme, and toxic skin eruptions, have occurred during atazanavir therapy. Inform patients to immediately discontinue atazanavir and contact a clinician if manifestations of severe skin reactions or hypersensitivity occur (e.g., severe rash or rash accompanied by shortness of breath, fever, general malaise, muscle or joint aches, blisters, oral lesions, conjunctivitis, facial edema).
-
Advise patients that kidney stones and/or gallstones have been reported and some patients required hospitalization or experienced complications, and that discontinuance of the drug may be necessary.
-
Advise women to inform their clinician if they are or plan to become pregnant. Advise women that there is a pregnancy registry that monitors pregnancy outcomes in women exposed to atazanavir during pregnancy.
-
Advise women to inform their clinician if they plan to breast-feed.
-
Advise patients to inform their clinician of existing or contemplated concomitant therapy, including prescription and OTC drugs and dietary or herbal supplements (e.g., St. John’s wort), and any concomitant illnesses.
-
Advise patients of other important precautionary information.
Additional Information
The American Society of Health-System Pharmacists, Inc. represents that the information provided in the accompanying monograph was formulated with a reasonable standard of care, and in conformity with professional standards in the field. Readers are advised that decisions regarding use of drugs are complex medical decisions requiring the independent, informed decision of an appropriate health care professional, and that the information contained in the monograph is provided for informational purposes only. The manufacturer’s labeling should be consulted for more detailed information. The American Society of Health-System Pharmacists, Inc. does not endorse or recommend the use of any drug. The information contained in the monograph is not a substitute for medical care.
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Powder |
50 mg (of atazanavir) per packet |
Reyataz |
Bristol-Myers Squibb |
|
Capsules |
150 mg (of atazanavir)* |
Reyataz |
Bristol-Myers Squibb |
|
|
200 mg (of atazanavir) |
Reyataz |
Bristol-Myers Squibb |
||
|
300 mg (of atazanavir) |
Reyataz |
Bristol-Myers Squibb |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions December 10, 2024. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
† Off-label: Use is not currently included in the labeling approved by the US Food and Drug Administration.
Reload page with references included
Related/similar drugs
Frequently asked questions
More about atazanavir
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (4)
- Drug images
- Side effects
- Dosage information
- During pregnancy
- Drug class: protease inhibitors
- Breastfeeding
- En español