Valoctocogene Roxaparvovec (Monograph)
Brand name: Roctavian
Drug class: Gene Therapy
Introduction
Valoctocogene roxaparvovec-rvox is a recombinant adeno-associated virus serotype 5 (AAV5) vector-based gene therapy containing a DNA sequence encoding the B-domain deleted SQ form of human coagulation factor VIII.
Uses for Valoctocogene Roxaparvovec
Valoctocogene roxaparvovec-rvox has the following uses:
Valoctocogene roxaparvovec-rvox is indicated for the treatment of adults with severe hemophilia A (congenital factor VIII deficiency with factor VIII activity < 1 IU/dL) without pre-existing antibodies to adeno-associated virus serotype 5 (AAV5) detected by an FDA-approved test. Designated an orphan drug by FDA for this use.
Efficacy of valoctocogene roxaparvovec-rvox was evaluated in a phase 3 open-label single-dose, single-arm multinational study in 134 adult males with severe hemophilia A. Patients without detectable, pre-existing antibodies to AAV5 capsid were eligible for therapy. Patients received a single IV dose of valoctocogene roxaparvovec-rvox 6 x 1013 vg/kg. The mean annualized bleeding rate during the efficacy evaluation period (median follow-up of 3 years) was 2.6 bleeds/year compared to a mean baseline annualized bleeding rate of 5.4 bleeds/year. The majority of patients treated with valoctocogene roxaparvovec-rvox received immunosuppressive medications, including steroids, to control elevations in transaminases and to prevent loss of transgene expression. In the study population, a total of 5 patients (4%) did not respond and 17 patients (15%) lost response to treatment over a median time of 2.3 (range: 1.0 to 3.3) years. Further study is needed to evaluate long-term durability and safety.
The National Hemophilia Society's Medical and Scientific Advisory Council (MASAC) has published guidance for hemophilia treatment centers on delivering gene therapy for hemophilia. For additional information, consult the guidelines at https://www.hemophilia.org/healthcare-professionals/guidelines-on-care/masac-documents/masac-document-277-masac-recommendations-on-hemophilia-treatment-center-preparedness-for-delivering-gene-therapy-for-hemophilia.
Valoctocogene Roxaparvovec Dosage and Administration
General
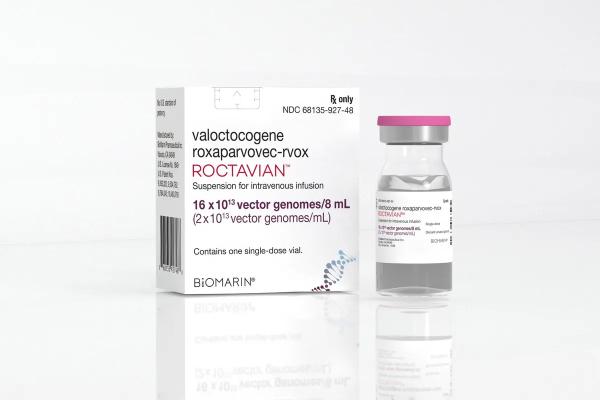
Valoctocogene roxaparvovec-rvox is available in the following dosage form(s) and strength(s):
-
Suspension for IV infusion.
-
Valoctocogene roxaparvovec-rvox has a nominal concentration of 2 × 1013 vector genomes (vg) valoctocogene roxaparvovec-rvox per mL; each vial contains an extractable volume of not less than 8 mL (16 × 1013 vg).
Dosage
It is essential that the manufacturer's labeling be consulted for more detailed information on dosage and administration of this drug. Dosage summary:
Adults
Dosage and Administration
For one-time single-dose IV use only. Administer as an IV infusion through a peripheral venous catheter; do not administer as an IV push or bolus.
-
Treatment with valoctocogene roxaparvovec-rvox should be under the supervision of a physician experienced in the treatment of hemophilia and/or bleeding disorders.
-
Administer valoctocogene roxaparvovec-rvox in a setting where personnel and equipment are immediately available to treat infusion-related reactions.
-
Perform baseline testing to select patients, including testing for pre-existing antibodies to adeno-associated virus serotype 5 (AAV5), factor VIII inhibitor presence, and liver health assessments. Information on FDA-approved tests for the detection of antibodies to AAV5 is available at: [Web].
-
The recommended dose of valoctocogene roxaparvovec-rvox is 6 × 1013 vector genomes (vg) per kg of body weight administered as a single IV infusion using a flow rate-controlled syringe pump. See Full Prescribing Information for instructions on calculating dose and number of vials required.
-
Start the infusion at 1 mL/minute. If tolerated, the rate may be increased every 30 minutes by 1 mL/minute up to a maximum rate of 4 mL/minute. The infusion time depends on infusion volume, rate and patient response and can be, for example, 2 to 5 hours or longer for a patient weighing 100 kg.
-
If an infusion-related reaction occurs during administration, decrease the infusion rate or stop the infusion. Administer treatment as needed to manage infusion reaction. If the infusion is stopped, restart the infusion at a rate of 1 mL/minute and consider maintaining it at a previously tolerated level for the remainder of the infusion. If the infusion needs to be restarted, the infusion should be completed within 10 hours of initial drug product thaw. Discontinue infusion for anaphylaxis.
-
See Full Prescribing Information for additional instructions on preparation and administration of valoctocogene roxaparvovec-rvox, and for monitoring recommendations.
Cautions for Valoctocogene Roxaparvovec
Contraindications
-
Active infections, either acute or uncontrolled chronic.
-
Known significant hepatic fibrosis (stage 3 or 4), or cirrhosis.
-
Known hypersensitivity to mannitol.
Warnings/Precautions
Infusion-related Reactions
Infusion-related reactions, including hypersensitivity reactions and anaphylaxis, have occurred during and/or following valoctocogene roxaparvovec administration. Symptoms included one or more of the following: urticaria, pruritus, rash, sneezing, coughing, dyspnea, rhinorrhea, watery eyes, tingling throat, nausea, diarrhea, hypotension, tachycardia, presyncope, pyrexia, rigors, and chills.
Monitor patients during and for at least 3 hours after completion of valoctocogene roxaparvovec infusion. Do not infuse the product faster than 4 mL/minute.
In the event of an infusion reaction, administration of valoctocogene roxaparvovec-rvox should be slowed or stopped. Restart at a lower rate after the infusion reaction has resolved. Discontinue infusion for anaphylaxis. Consider treatment with a corticosteroid, antihistamine, and other measures for management of an infusion reaction.
Hepatotoxicity
IV administration of a liver-directed AAV vector could lead to liver enzyme elevations (transaminitis), especially ALT elevation. Transaminitis is presumed to occur due to immune-mediated injury of transduced hepatocytes and may reduce the therapeutic efficacy of AAV-vector based gene therapy.
Majority of patients treated with valoctocogene roxaparvovec-rvox experienced ALT elevations. Most ALT elevations occurred within the first year following valoctocogene roxaparvovec-rvox administration, especially within the first 26 weeks, were low-grade, and resolved. The median time (range) to the first ALT elevation (defined as ALT ≥ 1.5 × baseline or above ULN) was 7 weeks (0.4, 159 weeks) and the median duration (range) was 4 weeks (0.1, 135 weeks). Some ALT elevations were associated with a decline in factor VIII activity.
The majority of the 112 patients in the clinical trial of valoctocogene roxaparvovec-rvox required corticosteroids for ALT elevation. The median duration (range) of corticosteroid use was 35 weeks (3, 120 weeks). The median duration (range) of alternate immunosuppressive medications use was 26 weeks (6, 118 weeks). In 20 (18%) patients, the duration of immunosuppression was > 1 year.
Monitor ALT and institute corticosteroid treatment in response to ALT elevations, as required. Monitor ALT and factor VIII activity levels weekly and, as clinically indicated, during corticosteroid therapy. Monitor for and manage adverse reactions secondary to corticosteroid therapy.
Since some ALT elevations have been attributed to alcohol consumption in clinical studies, patients should abstain from alcohol consumption for at least a year following valoctocogene roxaparvovec infusion and limit alcohol use thereafter. Concomitant medications may cause hepatotoxicity, or decrease factor VIII activity, or change plasma corticosteroid levels which may impact liver enzyme elevation and/or factor VIII activity. Closely monitor concomitant medication use including herbal products and nutritional supplements and consider alternative medications in case of potential drug interactions.
Thromboembolic Events
Elevated factor VIII activity level above the ULN as measured by the chromogenic substrate assays (CSA), or one-stage clotting assays (OSA), or both assays has occurred following valoctocogene roxaparvovec-rvox administration. Thirty-eight (28%) patients experienced elevations of factor VIII above ULN with a median time to first occurrence of 14 weeks and a median total duration above ULN of 12 weeks.
An increase in factor VIII activity may increase the risk for venous and arterial thromboembolic events. There are no data in patients with a history of venous or arterial thromboembolism or known history of thrombophilia since such patients were excluded from clinical trials of valoctocogene roxaparvovec-rvox.
Evaluate patients for risk of thrombosis including general cardiovascular risk factors before and after administration of valoctocogene roxaparvovec. Advise patients on their individual risk of thrombosis in relation to their factor VIII activity levels above ULN and consider prophylactic anticoagulation. Advise patients to seek immediate medical attention for signs or symptoms indicative of a thrombotic event.
Monitoring Laboratory Tests
Factor VIII Assays
Factor VIII activity produced by valoctocogene roxaparvovec-rvox in human plasma is higher if measured with OSA compared to CSA. In clinical studies, there was a high correlation between OSA and CSA factor VIII activity levels across the entire range of each assay's results. For routine clinical monitoring of factor VIII activity levels, either assay may be used. The conversion factor between the assays can be approximated based on clinical study results (central laboratory) to be: OSA = 1.5 × CSA. For example, a factor VIII activity level of 50 IU/dL using CSA calculates to a level of 75 IU/dL using OSA. The OSA to CSA ratio depends on the factor VIII assay reagents used by the laboratory and can range from 1.3 to 2.0, therefore, the same type of OSA or CSA reagents should be used to monitor factor VIII levels over time.
When switching from hemostatic products prior to valoctocogene roxaparvovec treatment, physicians should refer to the relevant prescribing information to avoid the potential for factor VIII activity assay interference during the transition period.
Factor VIII Inhibitors
Monitor patients through appropriate clinical observations and laboratory tests for the development of factor VIII inhibitors after valoctocogene roxaparvovec administration. Perform an assay that detects factor VIII inhibitors if bleeding is not controlled, or plasma factor VIII activity levels decrease.
Malignancy
The integration of liver-targeting AAV vector DNA into the genome may carry the theoretical risk of hepatocellular carcinoma development.
Valoctocogene roxaparvovec is composed of a non-replicating AAV5 vector whose DNA persists largely in episomal form. Low levels of vector integration were found following evaluation of liver samples from 5 patients and parotid gland tissue sample from 1 patient in clinical studies and liver samples from 12 nonhuman primates. Valoctocogene roxaparvovec can also insert into the DNA of other human body cells. No malignancies assessed as being likely related to valoctocogene roxaparvovec-rvox were observed in clinical studies.
Monitor patients with risk factors for hepatocellular carcinoma (e.g., hepatitis B or C, non-alcoholic fatty liver disease, chronic alcohol consumption, non-alcoholic steatohepatitis, advanced age) with regular liver ultrasound (e.g., annually) and alpha-fetoprotein testing for 5 years following valoctocogene roxaparvovec administration.
In the event that a malignancy occurs, contact BioMarin Pharmaceutical Inc. at 1-866-906-6100 to obtain instructions on collecting patient samples for testing.
Specific Populations
Pregnancy
Valoctocogene roxaparvovec is not intended for administration in women. There are no data on the use of valoctocogene roxaparvovec-rvox in pregnant women to inform a drug-associated risk of adverse developmental outcome. Animal reproduction and developmental toxicity studies have not been conducted with valoctocogene roxaparvovec-rvox. It is not known whether valoctocogene roxaparvovec can cause fetal harm when administered to a pregnant woman or can affect reproduction capacity.
The estimated background risk of major birth defects and miscarriage for the indicated population is unknown. In the US general population, the estimated background risk of major birth defects occurs in 2 to 4% of the general population and miscarriage occurs in 15 to 20% of clinically recognized pregnancies.
Lactation
Valoctocogene roxaparvovec is not intended for administration in women. There is no information regarding the presence of valoctocogene roxaparvovec-rvox in human milk, the effects on the breastfed infant, or the effects on milk production.
Females and Males of Reproductive Potential
Valoctocogene roxaparvovec is not intended for administration in women.
In clinical studies, after administration of valoctocogene roxaparvovec-rvox, transgene DNA was detectable in semen. In nonclinical studies in healthy mice, the vector DNA was detected in the testes for at least 182 days post-administration of valoctocogene roxaparvovec-rvox at a dose level of 2.1 × 1014vg/kg. In a mating study in immune-deficient mice, valoctocogene roxaparvovec-rvox was not detected in liver tissues of offspring of naïve females mated with dosed males.
For 6 months after administration of valoctocogene roxaparvovec, men of reproductive potential and their female partners must prevent or postpone pregnancy using an effective form of contraception, and men must not donate semen.
Pediatric Use
The safety and effectiveness of valoctocogene roxaparvovec in pediatric patients have not been established.
Geriatric Use
A single patient ≥ 65 years of age was treated with valoctocogene roxaparvovec-rvox in clinical studies. Clinical studies did not include sufficient numbers of patients 65 years of age and over to determine whether efficacy or safety differs compared to younger patients.
Human Immunodeficiency Virus (HIV) Positive Patients
In clinical studies, 3 HIV infected patients have been treated with valoctocogene roxaparvovec-rvox. Clinical studies did not include sufficient numbers of patients with HIV to determine whether efficacy and safety differs compared to patients without HIV infection.
A single HIV infected patient treated with valoctocogene roxaparvovec-rvox developed hepatocellular injury that subsequently resolved and was attributed to concomitant administration with the antiretroviral drug efavirenz.
Factor VIII Inhibitors
The safety and effectiveness of valoctocogene roxaparvovec in patients with prior or active factor VIII inhibitors have not been established. Patients with active factor VIII inhibitors should not take valoctocogene roxaparvovec.
After administration of valoctocogene roxaparvovec, patients should be monitored for the development of factor VIII inhibitors by appropriate clinical observations and laboratory tests.
Hepatic Impairment
The safety and effectiveness of valoctocogene roxaparvovec in patients with hepatic impairment has not been established. Clinical studies excluded patients with known hepatic cirrhosis, significant fibrosis (stage 3 or 4 on the Batts-Ludwig scale or equivalent), current hepatitis B or C, or history of hepatic malignancy. No dose adjustments can be recommended for patients with hepatic impairment.
Renal Impairment
The safety and effectiveness of valoctocogene roxaparvovec in patients with renal impairment has not been established. No dose adjustments can be recommended for patients with renal impairment.
Common Adverse Effects
-
Most common adverse reactions (incidence ≥ 5%) were nausea, fatigue, headache, infusion-related reactions, vomiting, and abdominal pain.
-
Most common laboratory abnormalities (incidence ≥ 10%) were increased ALT, increased AST, increased lactate dehydrogenase (LDH), increased creatine phosphokinase (CPK), increased factor VIII activity levels, increased gamma-glutamyl transferase (GGT) and increased bilirubin concentrations > ULN.
Drug Interactions
Specific Drugs
It is essential that the manufacturer's labeling be consulted for more detailed information on interactions with this drug, including possible dosage adjustments. Interaction highlights:
Prior to valoctocogene roxaparvovec administration, the patient's existing medications should be reviewed to determine if they should be modified to prevent anticipated interactions described in this section.
Concomitant medications should be monitored after valoctocogene roxaparvovec administration, and the need to change concomitant medications based on patient's hepatic status and risk should be evaluated. When a new medication is started, close monitoring of ALT and factor VIII activity levels (e.g., weekly to every 2 weeks for the first month) is recommended to assess potential effects on both levels.
No in vivo interaction studies have been performed.
Isotretinoin: In one patient, decreased factor VIII activity without ALT elevation was detected after starting treatment with systemic isotretinoin following valoctocogene roxaparvovec-rvox infusion. An in vitro study in human primary hepatocytes indicated that isotretinoin suppressed factor VIII transcription independent of hepatotoxicity, without impact on ALT, and expression was partially restored upon cessation of isotretinoin treatment. Isotretinoin is not recommended in patients who are benefiting from valoctocogene roxaparvovec.
Efavirenz: One HIV positive patient treated with valoctocogene roxaparvovec-rvox at a dose of 4 × 1013 vg/kg while on an antiretroviral therapy regimen consisting of efavirenz, lamivudine, and tenofovir experienced asymptomatic elevations of ALT, AST, and GGT (> 5.0 × ULN) and serum bilirubin (> ULN and up to 1.5 × ULN) at Week 4. The reaction resolved after the antiretroviral therapy regimen was changed to a regimen without efavirenz. An in vitro study in human primary hepatocytes indicated that efavirenz suppressed factor VIII transcription independent of hepatotoxicity, and expression was not restored upon discontinuation of efavirenz. Efavirenz is not recommended in patients treated with valoctocogene roxaparvovec.
Interactions with agents that may reduce or increase plasma concentrations of corticosteroids: Agents that may reduce or increase the plasma concentration of corticosteroids (e.g., agents that induce or inhibit cytochrome P450 3A4) can decrease the efficacy of the corticosteroid regimen or increase their side effects.
Vaccinations: Prior to valoctocogene roxaparvovec-rvox infusion, ensure up to date vaccinations. Individual vaccination schedules may need to be adjusted to accommodate concomitant immunosuppressive therapy. Live vaccines should not be administered to patients while on immunosuppressive therapy.
Actions
Mechanism of Action
Valoctocogene roxaparvovec-rvox is an adeno-associated virus serotype 5 (AAV5) based gene therapy vector, designed to introduce a functional copy of a transgene encoding the B-domain deleted SQ form of human coagulation factor VIII (hFVIII-SQ). Transcription of this transgene occurs within the liver, using a liver-specific promoter, which results in the expression of hFVIII-SQ. The expressed hFVIII-SQ replaces the missing coagulation factor VIII needed for effective hemostasis. Valoctocogene roxaparvovec-rvox is derived from naturally occurring adeno-associated virus using recombinant technology.
Advice to Patients
-
Inform patients of the risks and required precautions prior to valoctocogene roxaparvovec infusion.
-
Inform patients that prior to dosing valoctocogene roxaparvovec, blood tests to look for factor VIII inhibitors and detect antibodies to AAV5 will be necessary. If these tests are positive, the patient will not be a candidate for valoctocogene roxaparvovec.
-
Inform patients that prior to dosing valoctocogene roxaparvovec, liver health assessments, which include measuring liver function tests, liver ultrasound, and elastography or laboratory assessments for assessing hepatic fibrosis, will be necessary. If these tests are abnormal, the patient may not be a good candidate for valoctocogene roxaparvovec.
-
Inform patients that prior to dosing valoctocogene roxaparvovec, it will be necesssary to assess for suitability for corticosteroids and/or other immunosuppressive therapy. Inform patients that they may receive corticosteroids and/or other immunosuppressive agents for an extended period of time and communicate any risks associated with these therapies. The baseline assessment for suitability for immunosuppression may deem that the patient is not a good candidate for immunosuppression and hence not a good candidate for valoctocogene roxaparvovec.
-
Inform patients that infusion reactions including anaphylaxis have occurred. Patients will be monitored during and for at least 3 hours after infusion.
-
Educate patients on possible symptoms of infusion reactions during and after infusion and advise them to immediately inform medical staff if they experience such a reaction. When discharging the patient, provide instructions on actions in case of a new or recurrent reaction and when to seek medical attention.
-
Inform patients of the importance of liver enzyme and factor VIII level monitoring. Valoctocogene roxaparvovec can cause elevation of certain liver enzymes. Elevation in liver enzymes may be associated with decrease in factor VIII activity. Weekly blood test will be required for at least 26 weeks. Monitoring beyond this time is usually less frequent but depends on clinical situation, prior laboratory test results, and ongoing treatment with corticosteroids or other immunosuppressive therapy.
-
Advise patients on tapering factor VIII concentrates/hemostatic agents and, as necessary, on whether and how to continue or re-start their use, and on actions in case of invasive procedures, surgery, trauma, or bleeds.
-
Advise patients that not all patients may respond to valoctocogene roxaparvovec and that currently it is not possible to predict who will respond and how long the treatment response will continue. Counsel patients, as necessary, on when they may need to re-instate prophylactic use of factor VIII concentrates/hemostatic agents.
-
Inform patients undergoing corticosteroid treatment to adhere to the regimen and about potential adverse reactions and necessary precautions.
-
Advise patients that treatment with immunosuppressive agents other than corticosteroids may be required in case of intolerance, or adverse event from or failure of corticosteroid therapy.
-
Advise patients on how to maintain or improve hepatic health. Advise patients that they should abstain from consuming alcohol for at least one year after treatment and how much alcohol may be acceptable for them in the longer term.
-
Advise patients not to use any medications, herbal products, or supplements without first confirming with a health professional that they are not hepatotoxic. If use of a hepatotoxic agent appears unavoidable, the patient's healthcare provider should discuss potential alternatives and any implications for patient monitoring (i.e., more frequent monitoring of liver enzymes and factor VIII activity).
-
Inform patients that elevated factor VIII activity above the upper limit of normal has occurred following valoctocogene roxaparvovec-rvox administration. Such elevations of factor VIII activity may increase the risk of a thromboembolic event.
-
As necessary, advise patients of their risk factors for thrombotic events and general cardiovascular risk factors, how to minimize their risk, how to recognize a thrombotic event and to seek immediate medical attention if they observe signs or symptoms that can indicate a thrombotic event.
-
Advise patients that, after a male patient has been treated with valoctocogene roxaparvovec, the patient and/or his female partner must avoid pregnancy for a period of 6 months, and that male patients must not donate semen for a period of 6 months.
-
Instruct patients on acceptable methods of contraception.
-
Advise patients not to donate blood, organs, tissues, and cells for transplantation after treatment with valoctocogene roxaparvovec.
-
Advise patients that valoctocogene roxaparvovec is a one-time treatment. Currently, treatment with valoctocogene roxaparvovec precludes the patient from receiving another gene therapy for hemophilia.
-
Inform patients that since valoctocogene roxaparvovec is a liver-directed AAV therapy, there may be a theoretical risk of hepatocellular carcinoma. Patients with risk factors for hepatocellular carcinoma should be monitored regularly for 5 years with regular ultrasound and blood tests (alpha-fetoprotein). No malignancies assessed as being likely related to valoctocogene roxaparvovec-rvox treatment have been reported in clinical trials. Since the vector can insert into DNA of any cell, other malignancies may also occur.
-
Advise patients to contact BioMarin Pharmaceutical Inc. (1-866-906-6100) if they are diagnosed with any malignancy.
-
Inform patients that they should be enrolled in a 15-year registry to evaluate the long-term efficacy and safety of hemophilia treatments.
Additional Information
AHFSfirstRelease™. For additional information until a more detailed monograph is developed and published, the manufacturer's labeling should be consulted. It is essential that the manufacturer's labeling be consulted for more detailed information on usual uses, dosage and administration, cautions, precautions, contraindications, potential drug interactions, laboratory test interferences, and acute toxicity.
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Parenteral |
Suspension, for IV infusion |
nominally 2 × 1013 vector genomes (vg) per mL |
Roctavian (one single-dose vial containing an extractable volume of not less than 8 mL, containing 16 × 1013 vg) |
BioMarin |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions July 21, 2023. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
Reload page with references included
Related/similar drugs
Biological Products Related to valoctocogene roxaparvovec
Find detailed information on biosimilars for this medication.
More about valoctocogene roxaparvovec
- Check interactions
- Compare alternatives
- Side effects
- Dosage information
- During pregnancy
- Drug class: miscellaneous coagulation modifiers
- En español