Methimazole (Monograph)
Brand name: Tapazole
Drug class: Antithyroid Agents
ATC class: H03BB02
VA class: HS852
CAS number: 60-56-0
Introduction
Antithyroid agent; thioimidazole-derivative.
Uses for Methimazole
Hyperthyroidism
Used in patients with Graves’ disease with hyperthyroidism or toxic multinodular goiter for whom surgery or radioactive iodine therapy is not an appropriate treatment option.
Amelioration of symptoms of hyperthyroidism in preparation for thyroidectomy or radioactive iodine therapy.
Considered drug of choice by some clinicians for virtually every patient who chooses antithyroid drug therapy for treatment of Graves’ disease, except during first trimester of pregnancy when propylthiouracil is preferred, for treatment of thyroid storm, and in patients with minor adverse reactions to methimazole who refuse radioactive iodine therapy or surgery. (See Fetal/Neonatal Morbidity and also Pregnancy under Cautions, and see Thyrotoxic Crisis under Uses.)
Preferred agent when an antithyroid drug is required for a pediatric patient because of postmarketing reports of severe liver injury in pediatric patients receiving propylthiouracil. (See Pediatric Use under Cautions.)
Therapy maintains patients with Graves’ disease in euthyroid state for a period of several (generally 1–2) years until spontaneous remission occurs; however, spontaneous remission does not occur in all patients, and most patients eventually require ablative therapy (i.e., surgery, radioactive iodine). Methimazole does not affect underlying cause of hyperthyroidism; minimum duration of therapy necessary before assessing whether spontaneous remission has occurred not clearly established. Some clinicians state that if methimazole is chosen as the primary therapy for Graves’ disease, continue the drug for approximately 12–18 months in adults or 1–2 years in children, then taper or discontinue if TSH concentrations return to normal at that time. If patients remain hyperthyroid after completing a course of methimazole, consider treatment with radioactive iodine or thyroidectomy. However, may consider treatment with low-dose methimazole for >12–18 months in adult patients not in remission who prefer this pharmacologic approach. In pediatric patients, also may continue methimazole therapy until the child is considered old enough for radioactive iodine therapy or surgery.
Therapy with methimazole returns the hyperthyroid patient to a normal metabolic state prior to thyroidectomy and controls the thyrotoxic crisis that may accompany thyroidectomy. Some clinicians recommend that, whenever possible, adults or children with Graves’ disease undergoing thyroidectomy or adults with toxic adenoma† [off-label] or toxic multinodular goiter undergoing surgery be rendered euthyroid with methimazole prior to the procedure.
Therapy with methimazole controls symptoms of hyperthyroidism before and after radioactive iodine therapy until the ablative effects of iodine occur. However, beneficial and detrimental effects and optimal sequencing of antithyroid drugs before or after radioactive iodine therapy not clearly established.
Some clinicians recommend considering pretreatment with methimazole prior to radioactive iodine therapy for Graves’ disease, toxic adenoma† [off-label], or toxic multinodular goiter in adults at increased risk for complications due to worsening of hyperthyroidism (e.g., geriatric patients, patients with severe hyperthyroidism [e.g., extremely symptomatic, free thyroxine (T4) estimates 2–3 times the ULN] or substantial comorbidities [e.g., cardiovascular disease]). However, other clinicians state pretreatment with methimazole prior to radioactive iodine therapy not necessary because there is insufficient evidence to indicate that radioactive iodine worsens hyperthyroidism, and that pretreatment with methimazole will only delay treatment with radioactive iodine. In addition, pretreatment with methimazole may reduce efficacy of subsequent radioactive iodine therapy.
Some clinicians suggest that children with Graves’ disease having total T4 concentrations >20 mcg/dL or free T4 estimates >5 ng/dL who are to receive radioactive iodine therapy be pretreated with methimazole and β-adrenergic blockade until total T4 and/or free T4 estimates normalize before proceeding with radioactive iodine.
Does not induce remission in patients with nodular thyroid disease (i.e., toxic adenoma† [off-label], toxic multinodular goiter); discontinuance of therapy results in relapse. Therefore, some clinicians suggest to treat adults with overt toxic adenoma or toxic multinodular goiter with either radioactive iodine therapy or thyroidectomy, and to avoid long-term methimazole therapy. However, long-term (life-long) antithyroid drug therapy may be best choice for some geriatric or otherwise ill patients with limited longevity and increased surgical risk who can be monitored regularly (e.g., residents of nursing homes or other care facilities where compliance with radiation safety regulations may be difficult) or for patients who prefer this pharmacologic approach.
Thyrotoxic Crisis
May be used for management of thyrotoxic crisis, although not considered antithyroid agent of first choice. Usually initiated before iodide (e.g., potassium iodide, strong iodine solution) therapy.
Methimazole Dosage and Administration
General
-
May use a β-adrenergic blocking agent (e.g., propranolol) concomitantly to manage peripheral signs and symptoms of hyperthyroidism, particularly cardiovascular effects (e.g., tachycardia).
Administration
Administer orally.
Oral Administration
Manufacturer recommends administering total daily dosage usually in 3 equally divided doses at approximately 8-hour intervals. Alternatively, some clinicians state that drug may be administered as a single daily dose.
Dosage
Pediatric Patients
Hyperthyroidism
Graves’ Disease with Hyperthyroidism or Toxic Multinodular Goiter
OralInitially, 0.4 mg/kg daily, usually given in 3 equally divided doses at approximately 8-hour intervals. Alternatively, some clinicians recommend usual dosage of 0.2–0.5 mg/kg daily (range: 0.1–1 mg/kg daily). These clinicians also suggest the following general dosages, calculated based on the patient's age and rounded to the nearest quarter-, half-, or whole-tablet dosage strengths: 1.25 mg daily for infants; 2.5–5 mg daily for children 1–5 years of age; 5–10 mg daily for children 5–10 years of age; and 10–20 mg daily for children 10–18 years of age. Patients with severe clinical or biochemical hyperthyroidism may receive dosages that are 50–100% higher than those usually recommended.
Maintenance dosage: Approximately half of initial dosage or less.
Optimum duration of therapy not clearly established. However, some clinicians suggest administering drug for 1–2 years, then discontinue or reduce dosage to assess whether patient is in remission. If patient is not in remission following 1–2 years of therapy, consider treatment with radioactive iodine or thyroidectomy. Alternatively, may continue methimazole therapy for extended periods as long as adverse effects do not occur and hyperthyroidism is controlled; may use methimazole therapy as a bridge to radioactive iodine therapy or surgery at a later age if remission still has not occurred. May continue low-dose methimazole in selected situations in which radioactive iodine therapy or surgery may not be suitable or possible.
Preparation for Surgical Treatment
OralInitially, 0.4 mg/kg daily, usually given in 3 equally divided doses at approximately 8-hour intervals.
Some clinicians recommend administering methimazole usually for 1–2 months to achieve euthyroidism in preparation for thyroidectomy in patients with Graves’ disease.
Preparation for Radioactive Iodine Therapy
OralInitially, 0.4 mg/kg daily, usually given in 3 equally divided doses at approximately 8-hour intervals.
Some clinicians recommend discontinuing methimazole 3–5 days before radioactive iodine therapy. Although some clinicians restart antithyroid drugs after radioactive iodine therapy, this practice is seldom required in children.
Adults
Hyperthyroidism
Graves’ Disease with Hyperthyroidism or Toxic Multinodular Goiter
OralInitially, 15 mg daily for mild hyperthyroidism, 30–40 mg daily for moderately severe hyperthyroidism, or 60 mg daily for severe hyperthyroidism. Alternatively, some clinicians recommend an initial dosage of 10–20 mg daily to restore euthyroidism.
Considerable improvement or normal thyroid function generally achieved following 4–12 weeks of therapy, after which dosage may be decreased while maintaining normal thyroid function. Carefully adjust subsequent dosage according to patient’s tolerance and therapeutic response. (See Laboratory Monitoring under Cautions.)
Maintenance dosage: Manufacturer recommends 5–15 mg daily. Alternatively, some clinicians recommend 5–10 mg daily.
Optimum duration of therapy not clearly established. However, some clinicians suggest continuing therapy for approximately 12–18 months, then taper or discontinue drug if TSH concentrations return to normal at that time. If patient remains hyperthyroid after completing a course of methimazole, consider treatment with radioactive iodine or thyroidectomy. However, may also consider long-term (>12–18 months) low-dose methimazole therapy in patients not in remission who prefer this pharmacologic approach.
Preparation for Surgical Treatment
OralInitially, 15 mg daily for mild hyperthyroidism, 30–40 mg daily for moderately severe hyperthyroidism, or 60 mg daily for severe hyperthyroidism.
Discontinue methimazole at time of procedure.
Preparation for Radioactive Iodine Therapy
OralInitially, 15 mg daily for mild hyperthyroidism, 30–40 mg daily for moderately severe hyperthyroidism, or 60 mg daily for severe hyperthyroidism.
Some clinicians recommend discontinuing methimazole 2–7 days before radioactive iodine; may restart methimazole 3–7 days after radioactive iodine, then generally taper over 4–6 weeks as thyroid function normalizes and radioactive iodine becomes effective.
Thyrotoxic Crisis
OralSome clinicians recommend 60–80 mg daily.
Special Populations
Hepatic Impairment
No specific dosage recommendations at this time.
Renal Impairment
No specific dosage recommendations at this time.
Geriatric Patients
No specific dosage recommendations at this time.
Pregnancy
If used during pregnancy for management of hyperthyroidism, a sufficient, but not excessive, dosage is necessary; use lowest possible dosage. Thyroid dysfunction diminishes in many women as pregnancy proceeds; may be possible to reduce antithyroid dosage, and, in some patients, may discontinue antithyroid therapy 2–3 weeks before delivery. (See Pregnancy under Cautions.)
Cautions for Methimazole
Contraindications
-
Known hypersensitivity to methimazole or any ingredient in the formulation.
Warnings/Precautions
Warnings
Fetal/Neonatal Morbidity
May cause fetal harm, particularly during first trimester of pregnancy. Teratogenic effects, including aplasia cutis, craniofacial malformations (facial dysmorphism, choanal atresia), and GI malformations (esophageal atresia with or without tracheoesophageal fistula, umbilical abnormalities) reported rarely in infants. May cause fetal goiter and hypothyroidism (cretinism) when administered during pregnancy.
Congenital malformations reported approximately 3 times more often with prenatal exposure to methimazole compared with propylthiouracil. Distinct and consistent pattern of congenital malformations associated with use of methimazole, but not with propylthiouracil, particularly craniofacial malformations (e.g., scalp epidermal aplasia [aplasia cutis], facial dysmorphism, choanal atresia). Specific birth defects were associated with use of methimazole during the first trimester of pregnancy and not found when the drug was administered later in pregnancy. FDA has not found a consistent pattern of birth defects associated with use of propylthiouracil and has concluded there is no convincing evidence of an association between propylthiouracil use and congenital malformations, even with use during the first trimester. (See Pregnancy under Cautions and also see Distribution under Pharmacokinetics.)
Hematologic Effects
Risk of agranulocytosis; usually occurs within first 2 months of therapy, but rarely may occur after 4 months of therapy. May be dose related (possibly occurring more frequently with higher dosages); however, may occur irrespective of dosage, length of treatment, or previous exposure to antithyroid drug, and may occur more frequently in geriatric patients.
Leukopenia, thrombocytopenia, and/or aplastic anemia (pancytopenia) may occur. Hypoprothrombinemia and bleeding also may occur. (See Laboratory Monitoring under Cautions.)
Perform baseline CBC, including white count and differential, prior to initiating therapy in patients with Graves’ disease.
Monitor patient carefully for signs or symptoms of illness (e.g., sore throat, skin eruptions, fever, chills, headache, general malaise), particularly during early stages of therapy. If fever, sore throat, or other signs or symptoms of illness occur, determine leukocyte and differential counts to assess whether agranulocytosis has developed.
If agranulocytosis or aplastic anemia (pancytopenia) occurs, discontinue methimazole and monitor bone marrow indices. In patients who develop agranulocytosis or other serious adverse effects while receiving methimazole or propylthiouracil, use of the other drug is contraindicated because of risk of cross-sensitivity between the two drugs.
Hepatotoxicity
Hepatotoxicity (including acute liver failure) reported; risk appears to be lower with methimazole than with propylthiouracil, especially in pediatric patients. (See Pediatric Use under Cautions.)
Jaundice associated with methimazole-induced hepatitis may persist for several weeks after discontinuance of the drug.
Perform liver function tests (e.g., alkaline phosphatase, aminotransferase, bilirubin) prior to initiating therapy in patients with Graves’ disease.
Promptly evaluate liver function (alkaline phosphatase, bilirubin) and hepatocellular integrity (ALT, AST) if symptoms suggestive of hepatic dysfunction (e.g., anorexia, pruritus, right upper-quadrant pain) occur. If clinically relevant liver abnormality (e.g., hepatic aminotransferase concentrations >3 times the ULN) is detected, discontinue methimazole promptly. If hepatitis occurs, discontinue methimazole.
Hypothyroidism
May cause hypothyroidism necessitating routine monitoring of TSH and free T4 concentrations with dosage adjustments to maintain a euthyroid state.
May cause fetal goiter and cretinism when administered to a pregnant woman, because the drug readily crosses the placenta. (See Fetal/Neonatal Morbidity and also see Pregnancy under Cautions.)
Sensitivity Reactions
Cross-sensitivity
Cross-sensitivity between thioamides may occur (i.e., in approximately 50% of patients switched from one thioamide agent to the other).
In patients who develop serious adverse effects (e.g., agranulocytosis) while receiving either methimazole or propylthiouracil, use of other drug also is contraindicated, because of risk of cross-sensitivity between the two drugs. In patients experiencing serious allergic reactions to methimazole, use of the alternative antithyroid drug (i.e., propylthiouracil) not recommended.
General Precautions
Laboratory Monitoring
Before initiating thioamide therapy in patients with Graves’ disease, some clinicians recommend obtaining baseline free T4 and TSH concentrations; CBC, including white count and differential; and liver function tests (e.g., alkaline phosphatase, aminotransferase, bilirubin).
Monitor thyroid function (e.g., serum free T4, serum free or total triiodothyronine [T3], TSH) periodically (e.g., every 4–8 weeks [with subsequent dosage adjustments as needed] until thyroid function is stable or patient is euthyroid); once euthyroidism is achieved, monitor thyroid function every 2–3 months. Serum TSH not a reliable parameter to monitor early in therapy because it may remain suppressed for several months after initiation of therapy despite normalization of free T4 concentrations. A suppressed TSH concentration during this period does not indicate a need for dosage increase. However, once hyperthyroidism resolves, decrease maintenance dosage if serum TSH is elevated. Monitoring serum T3 concentrations may sometimes be useful for dosage adjustment; if total or free T3 concentrations remain elevated despite low, normal, or reduced free T4 concentrations, may need to increase antithyroid dosage. When methimazole is discontinued in patients with Graves’ disease, monitor thyroid function every 1–3 months for 6–12 months to diagnose relapse early.
Determine leukocyte and differential counts in patients who develop any signs or symptoms of illness (e.g., fever, sore throat) during therapy.
Monitor PT during therapy, particularly before surgical procedures, because of possible risk of hypoprothrombinemia and bleeding.
Dermatologic Effects
If exfoliative dermatitis occurs, discontinue methimazole.
Immunologic Effects
Antineutrophil cytoplasmic antibody (ANCA)-positive vasculitis with acute renal failure, arthritis, skin ulcerations, and a vasculitic rash reported rarely. If ANCA-positive vasculitis occurs, discontinue methimazole.
Specific Populations
Pregnancy
Category D. (See Fetal/Neonatal Morbidity under Cautions and also see Distribution under Pharmacokinetics.)
Despite potential fetal hazard, antithyroid agents still considered therapy of choice for management of hyperthyroidism during pregnancy. Since methimazole may be associated with the rare development of fetal abnormalities (e.g., aplasia cutis, craniofacial malformations [facial dysmorphism, choanal atresia], GI malformations [esophageal atresia with or without tracheoesophageal fistula, umbilical abnormalities]), propylthiouracil is preferred when an antithyroid drug is indicated during organogenesis, in the first trimester of pregnancy, or just prior to the first trimester of pregnancy. (See Fetal/Neonatal Morbidity under Cautions.) Switch patients receiving methimazole to propylthiouracil if pregnancy is confirmed in first trimester. May be preferable to switch from propylthiouracil to methimazole for the second and third trimesters (i.e., after the first trimester), because of potential maternal adverse effects of propylthiouracil (e.g., hepatotoxicity). If switching from propylthiouracil to methimazole, assess thyroid function after 2 weeks and then every 2–4 weeks thereafter. Not known if risk of methimazole-induced aplasia cutis or embryopathy outweighs risk of propylthiouracil-induced hepatotoxicity.
If used during pregnancy, a sufficient, but not excessive, dosage is necessary; use lowest possible dosage to control maternal disease. Initiate or adjust antithyroid drug therapy to maintain maternal free T4 concentrations at or just above the ULN of nonpregnant reference range, or to maintain total T4 concentrations at 1.5 times the ULN or the free T4 index in the ULN, while using lowest possible dosage. Monitor free T4 and TSH concentrations approximately every 2–6 weeks in women receiving antithyroid drugs during pregnancy. As thyroid dysfunction diminishes in many women as pregnancy proceeds, may be possible to reduce dosage of antithyroid drug; in some patients, may discontinue antithyroid drug 2–3 weeks before delivery.
If used during pregnancy or if patient becomes pregnant while receiving the drug, apprise of potential hazard to the fetus; inform patient of risks of methimazole-associated fetal malformations and risks of propylthiouracil-associated hepatotoxicity when considering antithyroid drug use during pregnancy.
Lactation
Distributed into milk. However, no effect on clinical status and no toxicity observed in nursing infants.
Generally compatible with breast-feeding; moderate dosages (i.e., 20–30 mg daily) appear to be safe. Preferred antithyroid drug in nursing women because maternal use of propylthiouracil associated with severe hepatotoxicity (i.e., hepatic necrosis in either woman or child). If antithyroid drug is used in nursing women, some clinicians recommend administering drug after a feeding and in divided doses, and monitoring thyroid function of nursing infants.
Pediatric Use
Preferred over propylthiouracil when an antithyroid drug is required for a pediatric patient because of postmarketing reports of severe liver injury in pediatric patients receiving propylthiouracil. (See Hyperthyroidism under Uses.) Postmarketing cases of severe liver injury, including hepatic failure requiring liver transplantation or resulting in death, reported in pediatric patients receiving propylthiouracil; however, no such reports observed with methimazole. (See Hepatotoxicity under Cautions.)
Common Adverse Effects
Rash, urticaria, pruritus, skin pigmentation, abnormal hair loss, nausea, vomiting, arthralgia, myalgia, paresthesia, loss of taste, epigastric distress, edema, headache, drowsiness, neuritis, vertigo, jaundice, sialadenopathy, lymphadenopathy.
Drug Interactions
Drugs Known to Cause Agranulocytosis
Use concomitantly with extreme caution. (See Hematologic Effects under Cautions.)
Specific Drugs
|
Drug |
Interaction |
Comments |
|---|---|---|
|
Anticoagulants, oral (e.g., warfarin) |
Potential inhibition of vitamin K activity, resulting in increased activity of oral anticoagulants (e.g., warfarin); however, anticoagulant effect of warfarin also may be decreased |
Consider additional monitoring of PT/INR, particularly prior to surgery; adjustment of warfarin dosage may be needed |
|
β-Adrenergic blocking agents |
Possible increased clearance of β-adrenergic blocking agents with a high extraction ratio during hyperthyroid state |
Reduction of β-blocker dosage may be needed when patient becomes euthyroid |
|
Digitalis glycosides |
Possible increased serum digitalis concentrations when hyperthyroid patients receiving a stable digitalis glycoside regimen become euthyroid |
Reduction of digitalis glycoside dosage may be needed when patient becomes euthyroid |
|
Theophylline |
Possible decreased theophylline clearance when hyperthyroid patients on a stable theophylline regimen become euthyroid |
Reduction of theophylline dosage may be needed when patient becomes euthyroid |
Methimazole Pharmacokinetics
Absorption
Bioavailability
Readily and rapidly absorbed from the GI tract following oral administration. Peak plasma concentrations attained within about 1 hour.
Distribution
Extent
Readily crosses the placenta.
Distributed into milk (in concentrations approximately equal to those in maternal serum).
Elimination
Metabolism
Metabolized in the liver.
Elimination Route
Excreted in urine; approximately 12% of dose excreted in urine within 24 hours.
Half-life
5–13 hours.
Stability
Storage
Oral
Tablets
15–30°C.
Actions
-
Inhibits the synthesis of thyroid hormones by interfering with the incorporation of iodine into tyrosyl residues of thyroglobulin; also inhibits the coupling of these iodotyrosyl residues to form iodothyronine.
-
Exact mechanism(s) not fully elucidated; however, methimazole may interfere with the oxidation of iodide ion and iodotyrosyl groups.
-
Limited evidence suggests that coupling reaction is more sensitive to antithyroid agents than the iodination reaction.
-
Does not inhibit the action of thyroid hormones already formed and present in the thyroid gland or circulation; also does not interfere with effectiveness of exogenously administered thyroid hormones. Patients whose thyroid gland contains a relatively high concentration of iodine (e.g., from prior ingestion, from administration during diagnostic radiologic procedures) may respond relatively slowly to antithyroid agents.
-
Unlike propylthiouracil, does not inhibit peripheral deiodination of T4 to triiodothyronine (T3).
Advice to Patients
-
Importance of informing clinicians immediately if signs or symptoms of illness (e.g., sore throat, skin eruptions, fever, chills, headache, general malaise) occur. Importance of immediately discontinuing the drug and contacting clinicians if signs or symptoms suggestive of agranulocytosis (e.g., fever, sore throat) occur. (See Hematologic Effects under Cautions.)
-
Importance of immediately discontinuing the drug and promptly informing clinicians if symptoms suggestive of hepatic injury (e.g., pruritic rash, jaundice, acholic stools, dark urine, arthralgias, abdominal pain, nausea, fatigue) occur. (See Hepatotoxicity under Cautions.)
-
Importance of informing clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs, as well as any concomitant illnesses.
-
Importance of women immediately informing clinicians if they are or plan to become pregnant or plan to breast-feed. Necessity for clinicians to advise women of methimazole-associated fetal malformations, as well as risks of propylthiouracil-associated hepatotoxicity when considering antithyroid drug use during pregnancy.
-
Importance of informing patients of other important precautionary information. (See Cautions.)
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
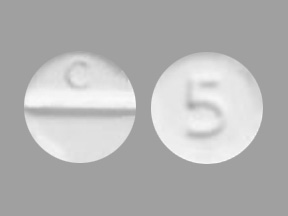
Oral |
Tablets |
5 mg* |
methIMAzole Tablets |
|
|
Tapazole (scored) |
King |
|||
|
10 mg* |
methIMAzole Tablets |
|||
|
Tapazole (scored) |
King |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions November 25, 2013. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
† Off-label: Use is not currently included in the labeling approved by the US Food and Drug Administration.
Reload page with references included
Related/similar drugs
Frequently asked questions
More about methimazole
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (114)
- Drug images
- Side effects
- Dosage information
- During pregnancy
- Support group
- Drug class: antithyroid agents
- Breastfeeding
- En español