Lynparza
Pronunciation: Lin-par-zah
Generic name: olaparib
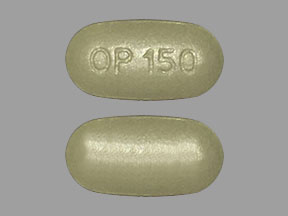
Dosage form: tablets (150mg, 100mg)
Drug class: PARP inhibitors
What is Lynparza?
Lynparza is a targeted cancer medicine used to treat specific types of ovarian cancer, breast cancer, fallopian tube cancer, pancreatic cancer, prostate cancer, and peritoneal cancer. Lynparza is often used if your cancer has a specific genetic marker, including BRAC1, BRCA2, HRR, and HER2-negative. Your doctor will test you for this gene.
Lynparza (olaparib) is a tablet that is usually taken twice daily, with or without food.
Lynparza was first FDA-approved in 2014 for advanced ovarian cancer.
How does Lynparza work?
PARP is a protein that helps damaged cells to repair themselves, including some cancer cells. If the cells are not repaired, then the cells die. Some cancer cells rely on PARP to repair their DNA so they can continue dividing. Lynparza is from a group of medicines called PARP inhibitors (poly (ADP-ribose) polymerase inhibitors). Lynparza works by blocking PARP, which means the cancer cells are no longer able to repair themselves and so die.
What is Lynparza used for?
Lynparza is FDA-approved to treat specific types of cancer.
BRCA-mutated Advanced Ovarian cancer
- first-line maintenance treatment,
- adult patients with deleterious or suspected deleterious germline or somatic BRCA-mutated advanced epithelial ovarian, fallopian tube, or primary peritoneal cancer,
- who are in complete or partial response to first-line platinum-based chemotherapy.
- patients should be selected based on an FDA-approved companion diagnostic for this medicine.
HRD-positive Advanced Ovarian Cancer
- first-line maintenance treatment in combination with bevacizumab
- adult patients with advanced epithelial ovarian, fallopian tube, or primary peritoneal cancer who are an incomplete or partial response to first-line platinum-based chemotherapy
- Cancer is associated with homologous recombination deficiency (HRD)-positive status defined by either a deleterious or suspected deleterious BRCA mutation, and/or genomic instability
- patients should be selected based on an FDA-approved companion diagnostic for this medicine.
Recurrent Ovarian Cancer
- maintenance treatment
- adult patients with recurrent epithelial ovarian, fallopian tube, or primary peritoneal cancer, who are in complete or partial response to platinum-based chemotherapy.
Germline BRCA-mutated HER2-negative High-Risk Early Breast Cancer
- adjuvant treatment of adult patients with deleterious or suspected deleterious gBRCAm human epidermal growth factor receptor 2 (HER2)-negative high-risk early breast cancer who have been treated with neoadjuvant or adjuvant chemotherapy
- patients should be selected based on an FDA-approved companion diagnostic for this medicine.
Germline BRCA-mutated HER2-negative Metastatic Breast Cancer
- adult patients with deleterious or suspected deleterious gBRCAm, HER2-negative metastatic breast cancer, who have been treated with chemotherapy in the neoadjuvant, adjuvant, or metastatic setting
- Patients with hormone receptor (HR)-positive breast cancer should have been treated with prior endocrine therapy or be considered inappropriate for endocrine therapy
- patients should be selected based on an FDA-approved companion diagnostic for this medicine.
Germline BRCA-mutated Metastatic Pancreatic Adenocarcinoma
- first-line maintenance treatment
- adult patients with deleterious or suspected deleterious gBRCAm metastatic pancreatic adenocarcinoma whose disease has not progressed on at least 16 weeks of a first-line platinum-based chemotherapy regimen
- patients should be selected based on an FDA-approved companion diagnostic for this medicine.
BRCA-mutated Metastatic Castration-Resistant Prostate Cancer
- Used in combination with abiraterone and prednisone or prednisolone for the treatment of adult patients with deleterious or suspected deleterious BRCA-mutated (BRCAm) metastatic castration-resistant prostate cancer (mCRPC).
- patients should be selected based on an FDA-approved companion diagnostic for this medicine.
Related/similar drugs
Enhertu, Erleada, Kisqali, Verzenio, Ibrance, Lupron Depot, estradiol
Warnings
Lynparza affects your immune system. You may get infections more easily, even serious or fatal infections. Call your doctor if you have a fever, weakness, tiredness, trouble breathing, easy bruising or bleeding, blood in your urine or stools, or weight loss.
You will need weekly or monthly blood tests, and your cancer treatments may be delayed based on the results.
Some people who take olaparib with a gonadotropin-releasing hormone (GnRH) medicine may develop a blood clot in the leg or in the lung. Call your doctor if you have pain or swelling in your arm or leg, shortness of breath, chest pain, rapid breathing, or fast heartbeats.
Lynparza may also cause serious lung problems. Call your doctor if you have chest pain, wheezing, trouble breathing, or a new or worsening cough.
Before taking this medicine
You should not use Lynparza if you are allergic to olaparib.
To make sure Lynparza is safe for you, tell your doctor if you have ever had:
- lung disease, breathing problems; or
- kidney disease.
Pregnancy
Lynparza can harm an unborn baby or cause a miscarriage if the mother or the father is using this medicine.
- If you are a woman, do not use this medicine if you are pregnant. You may need to have a negative pregnancy test before starting this treatment. Use effective birth control to prevent pregnancy while you are using this medicine and for at least 6 months after your last dose.
- If you are a man, use effective birth control if your sex partner is able to get pregnant. Keep using birth control for at least 3 months after your last dose. Also do not donate sperm during the 3 months after your last dose.
- Tell your doctor right away if a pregnancy occurs while either the mother or the father is using this medicine
Breastfeeding
Do not breastfeed while using this medicine, and for at least 1 month after your last dose.
How should I take Lynparza?
Take Lynparza exactly as prescribed by your doctor. Follow all directions on your prescription label and read all medication guides or instruction sheets. Your doctor may occasionally change your dose.
Lynparza is a tablet that is usually taken twice per day. Take your doses at regular intervals, about 12 hours apart. You may take this medicine with or without food. Swallow the tablet whole and do not crush, chew, or break it.
Olaparib affects your immune system. You may get infections more easily, even serious or fatal infections. Your doctor will need to examine you on a regular basis.
You may also need chest X-rays to be sure this medicine is not causing harmful effects on your lungs. Your cancer treatments may be delayed based on the results.
Dosing Information
The dose is usually 300 mg orally 2 times a day. The dose may be changed by your doctor due to renal impairment or other factors.
Lynparza is available in 150 mg and 100mg tablets.
For more detailed dosing information, click on the link below.
What happens if I miss a dose?
Skip the missed dose and use your next dose at the regular time. Do not use two doses at one time.
Do not take more than 4 Lynparza tablets in one day.
What happens if I overdose?
Seek emergency medical attention or call the Poison Help line at 1-800-222-1222.
What to avoid
Grapefruit and Seville oranges may interact with olaparib and lead to unwanted side effects. Avoid consuming grapefruit products and orange marmalades.
Lynparza side effects
Get emergency medical help if you have signs of an allergic reaction to Lynparza: hives; difficulty breathing; swelling of your face, lips, tongue, or throat.
You may get infections more easily, even serious or fatal infections. Call your doctor right away if you have signs of infection such as:
- fever, chills, weakness, feeling light-headed or very tired;
- mouth sores, skin sores;
- easy bruising, unusual bleeding;
- pain or burning when you urinate, blood in your urine or stools;
- pale skin, cold hands and feet;
- weight loss; or
- cough, wheezing, shortness of breath.
Your cancer treatments may be delayed if you have certain side effects.
Some people who take this medicine with a gonadotropin-releasing hormone (GnRH) medicine may develop a blood clot in the leg or in the lung. Call your doctor if you have pain or swelling in your arm or leg, shortness of breath, chest pain, rapid breathing, or fast heartbeats.
Common Lynparza side effects may include:
- low blood cell counts;
- nausea, vomiting, diarrhea;
- heartburn, indigestion, loss of appetite;
- dizziness, feeling weak or tired;
- headache;
- cough, shortness of breath; or
- altered sense of taste.
This is not a complete list of side effects, and others may occur. Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
What other drugs will affect Lynparza?
Sometimes it is not safe to use certain medications at the same time. Some drugs can affect your blood levels of other drugs you take, which may increase side effects or make the medications less effective.
Strong and Moderate CYP3A Inhibitors. Avoid using strong or moderate CYP3A inhibitors with this medicine. If a strong or moderate inhibitor must be used, then reduce the dose of Lynparza
Strong and Moderate CYP3A Inducers. Avoid using strong or moderate CYP3A inducers with this medicine as it decreases the olaparib exposure, which may reduce Lynparza effectiveness.
Other drugs may interact with Lynparza, including prescription and over-the-counter medicines, vitamins, and herbal products. Tell your doctor about all your current medicines and any medicine you start or stop using.
Storage
- Store at room temperature, between 68°F to 77°F (20°C to 25°C).
- Store in the original bottle to protect it from moisture.
- Keep all medicines out of reach of children.
Ingredients
Active ingredient: olaparib
Inactive ingredients:
- Tablet contains: copovidone, mannitol, colloidal silicon dioxide and sodium stearyl fumarate
- Tablet coating contains: hypromellose, polyethylene glycol 400, titanium dioxide, ferric oxide yellow and ferrosoferric oxide (150 mg tablet only)
Company
Distributed by:
AstraZeneca Pharmaceuticals LP, Wilmington, DE 19850
Popular FAQ
How long does it take Lynparza (olaparib) to work?
It takes Lynparza between two months and five months to start working depending on what cancer it is being used to treat. Continue reading
How effective is Lynparza (olaparib)?
Lynparza has been shown in studies to lower or delay the risk of the disease progression and extend survival when compared to a placebo (an inactive pill) or another cancer treatment. It is approved In the treatment of advanced or metastatic cancers, such as ovarian, breast, pancreatic or prostate cancer, as well as HER2-negative, high-risk early breast cancer with BRCA mutations. Continue reading
Does Lynparza (olaparib) cause hair loss?
Lynparza, a targeted cancer treatment, is classified as a PARP (or Poly ADP-ribose polymerase) inhibitor. PARP inhibitors like Lynparza generally do not cause hair loss. Hair loss has not been reported as a side effect of Lynparza in the package insert and clinical studies conducted by the manufacturer. Continue reading
References
More about Lynparza (olaparib)
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (17)
- Drug images
- Side effects
- Dosage information
- During pregnancy
- FDA approval history
- Drug class: PARP inhibitors
- Breastfeeding
- En español
Patient resources
Professional resources
Related treatment guides
Further information
Remember, keep this and all other medicines out of the reach of children, never share your medicines with others, and use Lynparza only for the indication prescribed.
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
Copyright 1996-2024 Cerner Multum, Inc. Version: 8.01.