Glycopyrrolate (Monograph)
Brand names: Bevespi Aerosphere (combination), Cuvposa, Lonhala Magnair, Robinul, Seebri Neohaler, Utibron Neohaler (combination)
Drug class: Antimuscarinics/Antispasmodics
VA class: AU350
CAS number: 596-51-0
Introduction
Antimuscarinic; a synthetic quaternary ammonium compound.365 366 367 368 369 a
Uses for Glycopyrrolate
COPD
Glycopyrrolate oral inhalation powder or solution: Maintenance treatment of airflow obstruction in patients with COPD, including chronic bronchitis and/or emphysema.368 369 373 374 375
Glycopyrrolate/formoterol fixed combination oral inhalation aerosol: Maintenance treatment of airflow obstruction in patients with COPD, including chronic bronchitis and/or emphysema.371 377
Glycopyrrolate/indacaterol fixed combination oral inhalation powder: Maintenance treatment of airflow obstruction in patients with COPD, including chronic bronchitis and/or emphysema.370 376
Not indicated for treatment of acute bronchospasm.368 369 370 371
Not indicated for treatment of asthma; safety and efficacy not established.370 371
Drooling
Glycopyrrolate oral solution: Symptomatic management of chronic severe drooling in pediatric patients with neurologic conditions (e.g., cerebral palsy) associated with problematic drooling.367 372
Peptic Ulcer Disease
Used orally or parenterally as an adjunct in the treatment of peptic ulcer disease;365 366 however, no conclusive data that it aids in healing, decreases rate of recurrence, or prevents complications of peptic ulcers.a b
Parenteral route preferred as adjunct in the treatment of peptic ulcer disease when rapid anticholinergic effect desired or oral administration not tolerated.365
With the advent of more effective therapies for the treatment of peptic ulcer disease, antimuscarinics have only limited usefulness in this condition.a b
Surgery
Used parenterally to inhibit salivation and excessive secretions of the respiratory tract (antisialogue).365 a b However, current surgical practice (e.g., using general anesthetics that do not stimulate salivary and tracheobronchial secretions) has reduced the need to control excessive respiratory secretions during surgery.a b
Used parenterally to prevent other cholinergic effects during surgery (e.g., cardiac arrhythmias, hypotension, bradycardia) secondary to visceral traction (resultant vagal stimulation), carotid sinus stimulation, or concomitant drugs (e.g., succinylcholine).365 a b
Used parenterally to block adverse muscarinic effects of anticholinesterase agents that are used after surgery to terminate curarization.365 a b
Ineffective for preventing acid-aspiration pneumonitis† [off-label] during surgery.a b
Related/similar drugs
Breztri Aerosphere, famotidine, pantoprazole, lidocaine, Symbicort, fentanyl, Protonix
Glycopyrrolate Dosage and Administration
Administration
Oral Administration
Tablets: Administer orally 2 or 3 times daily.366
Oral solution: Administer 3 times daily at least 1 hour before or 2 hours after meals.367 Must use an accurate measuring device to measure and administer oral solution.367
IM Administration
Injection: May be administered undiluted.365 May administer in the same syringe with other compatible preoperative medications.a (See Compatibility in Syringe under Stability.)
IV Administration
For solution and drug compatibility information, see Compatibility under Stability.
Injection: May be administered undiluted.365 Administer by direct IV injection;365 a alternatively, administer via the tubing of a running IV infusion of a compatible solution.365 a
Oral Inhalation
Oral Inhalation Powder
Administer glycopyrrolate oral inhalation powder using a special oral inhalation device (Neohaler) that delivers powdered drug from capsules.368 Administer the inhalation powder twice daily at the same time each day.368
Administer glycopyrrolate/indacaterol fixed combination oral inhalation powder using a special oral inhalation device (Neohaler) that delivers powdered drug from capsules.370 Administer the fixed-combination inhalation powder twice daily at the same time each day.370
Glycopyrrolate and glycopyrrolate/indacaterol capsules for oral inhalation should not be taken orally (i.e., swallowed).368 370
To use Neohaler device, remove cap, then open inhaler by holding the base firmly and tilting the mouthpiece.368 370 Peel away protective backing from a blister card containing glycopyrrolate or glycopyrrolate/indacaterol to expose one capsule.368 370 Do not push capsule through foil to remove it from the blister.368 370 With dry hands, remove capsule from blister; place capsule into capsule chamber of the device; do not place capsule into mouthpiece of device.368 370 Close inhaler fully until it clicks.368 370 Hold inhaler upright with the mouthpiece pointing upward; press both piercing buttons together firmly at the same time once (click will be heard), then release the piercing buttons fully.368 370 Piercing the capsule may produce very small pieces, which may pass into the mouth; pieces not expected to cause harm if swallowed or inhaled.368 370
Exhale completely; do not exhale into mouthpiece of inhaler device.368 370 Hold inhaler horizontally (piercing buttons facing left and right); place mouthpiece in mouth, closing lips firmly around it.368 370 Inhale rapidly, but steadily and as deeply as possible, without pressing the piercing buttons.368 370 During inhalation, a whirring noise created by the capsule spinning around in the chamber will be heard; a sweet flavor also may be detected.368 370 Continue holding the breath for at least 5–10 seconds or as long as comfortably possible while removing inhaler from mouth, then exhale.368 370 Open inhaler to see if any powder remains in the capsule.368 370 If powder remains, close inhaler and repeat steps for inhaling the drug.368 370 Most patients empty the capsule with 1 or 2 inhalations.368 370 Coughing may occur soon after inhaling the dose; coughing is not a concern.368 370 After inhalation, open mouthpiece and tip the device to dispose of the used capsule, then close inhaler and replace cap.368 370 Do not leave used capsules in the device.368 370
If whirring noise is not heard, capsule may be stuck in the capsule chamber.368 370 If this occurs, open inhaler and carefully loosen capsule by tapping base of the inhaler; do not press the piercing buttons.368 370 Then repeat steps to inhale the drug.368 370
Routine cleaning of inhaler not necessary; if desired, may clean mouthpiece inside and outside with a clean, dry, lint-free cloth, or may use a clean, dry, soft brush to wipe inhaler and remove any powder residue.368 370 Keep inhaler dry.368 370
Each capsule of glycopyrrolate oral inhalation powder (Seebri Neohaler) contains 15.6 mcg of glycopyrrolate.368 Actual amount of drug delivered to the lungs depends on factors such as the patient’s inspiratory flow rate and inspiratory time.368 Under standardized in vitro testing at a fixed flow rate of 90 L/minute for 1.3 seconds, Neohaler device delivered 13.1 mcg of glycopyrrolate from the 15.6-mcg capsule (equivalent to 12.5 mcg of glycopyrronium).368
Each capsule of glycopyrrolate/indacaterol oral inhalation powder (Utibron Neohaler) contains 15.6 mcg of glycopyrrolate and 27.5 mcg of indacaterol.370 Actual amount of drug delivered to the lungs depends on factors such as the patient’s inspiratory flow rate and inspiratory time.370 Under standardized in vitro testing at a fixed flow rate of 90 L/minute for 1.3 seconds, the Neohaler device delivered 12.8 mcg of glycopyrrolate (equivalent to 12.5 mcg of glycopyrronium) and 20.8 mcg of indacaterol from the capsule containing 15.6 mcg of glycopyrrolate and 27.5 mcg of indacaterol.370
Oral Inhalation Solution
Administer glycopyrrolate oral inhalation solution via nebulization using a special oral inhalation device (Magnair nebulizer system).369 Administer the inhalation solution twice daily at the same time each day.369
Glycopyrrolate solution for oral inhalation should not be taken orally (i.e., swallowed) and should not be injected.369
Assemble Magnair nebulizer system according to manufacturer's instructions for use and ensure it is working properly.369
Immediately prior to use, open the foil pouch; remove and separate the 2 single-dose vials; return one vial to the foil pouch and store in the nebulizer carrying bag.369 Insert vial to be used into bottom of medication cap until it clicks.369 Place medication cap with vial on top of handset body (with aerosol head already inserted) and turn in a clockwise direction until a click is heard; avoid touching the part of handset body that pierces the vial.369 Line up notch in medication cap with blue line on handset body.369
To administer the dose, insert mouthpiece, press controller on/off button, and breathe normally through the mouthpiece.369 Avoid tilting handset, loosening or removing medication cap, or unclasping the handset body until treatment is complete.369 At the end of treatment (2–3 minutes), a beep will sound and controller will shut off automatically.369
Follow manufacturer's instructions for cleaning handset after each treatment.369
Each single-dose vial of glycopyrrolate oral inhalation solution (Lonhala Magnair) contains 25 mcg of glycopyrrolate in 1 mL of solution.369 Actual amount of drug delivered to the lungs depends on patient factors.369 Under standardized in vitro testing, the Magnair device delivered approximately 14.2 mcg of glycopyrrolate (equivalent to 11.4 mcg of glycopyrronium) from the mouthpiece.369
Oral Inhalation Aerosol
Administer glycopyrrolate/formoterol fixed combination using a special oral inhalation device (Aerosphere) that delivers a metered-dose spray.371 Administer the oral inhalation aerosol as 2 inhalations twice daily (morning and evening).371
Before first use, ensure that inhaler device (Bevespi Aerosphere) is at room temperature.371 Remove inhaler from foil pouch.371
Shake well before each inhalation.371 Prime inhaler before first use.371 Remove cap from mouthpiece.371 Hold inhaler in upright position away from face.371 To release spray from the mouthpiece, press down firmly on center of dose indicator until canister stops moving in actuator; soft click may be heard.371 Repeat 3 more times, shaking well before each spray.371 Repeat priming process (using only 2 sprays rather than 4) if inhaler is not used for >7 days.371
Before first use, ensure that pointer on dose indicator is pointing to the right of the 120 or 30 inhalation mark in the dose indicator display window for the 120- or 28-inhalation canister, respectively.371 Color in the display window will change to red when there are only 20 or 10 sprays remaining in the inhaler for the 120- or 28-inhalation canister, respectively.371
To administer a dose, remove cap from mouthpiece.371 Shake inhaler well before each use.371 Hold inhaler with mouthpiece pointing toward face; exhale through mouth as fully and as comfortably as possible.371 Close lips around mouthpiece and tilt head back, keeping tongue below mouthpiece.371 While inhaling slowly and deeply, press down on center of dose indicator until canister stops moving in actuator and spray is released, then stop pressing.371 After inhaling, remove mouthpiece and hold breath as long as comfortably possible, up to 10 seconds, then breathe out gently.371 Repeat process for second inhalation.371 Replace cap on mouthpiece immediately after use.371
Clean inhaler once weekly to avoid drug buildup, which can block spray through the mouthpiece.371 To clean inhaler, first remove canister from actuator; do not clean canister or allow it to get wet.371 Remove cap from mouthpiece.371 Rinse actuator under warm water for about 30 seconds.371 Turn actuator upside down; rinse actuator again through mouthpiece for about 30 seconds.371 Shake as much water off mouthpiece as possible.371 Check the actuator and mouthpiece; if any drug buildup remains, repeat rinsing procedure.371 Allow the actuator to dry overnight.371 Do not put canister back into the actuator while wet.371 When the actuator is dry, gently press canister down into it; do not press too hard on canister since this may cause drug release.371 Prime inhaler after each cleaning by shaking well and releasing 2 sprays into the air away from face.371
After priming of the oral aerosol inhaler containing glycopyrrolate/formoterol (Bevespi Aerosphere), each actuation of the inhaler delivers 10.4 mcg of glycopyrrolate (equivalent to 8.3 mcg of glycopyrronium) and 5.5 mcg of formoterol fumarate from the valve.371 Dosage is expressed in terms of drug delivered from the actuator; each actuation of the inhaler delivers 9 mcg of glycopyrrolate (equivalent to 7.2 mcg of glycopyrronium) and 4.8 mcg of formoterol fumarate from the mouthpiece.371 Actual amount of drug delivered to the lungs depends on factors such as patient's coordination between actuation of the device and inspiration through the delivery system.371 The Bevespi Aerosphere inhalation aerosol delivers 28 or 120 metered sprays per 5.9- or 10.7-g canister, respectively.371
Dosage
Pediatric Patients
Drooling
Oral (Solution)
Children and adolescents 3–16 years of age: Initial dosage of 0.02 mg/kg 3 times daily; may titrate in increments of 0.02 mg/kg every 5–7 days based on therapeutic response and tolerance.367
Surgery
Preoperatively to Decrease Secretions and Block Cardiac Vagal Reflexes
IM0.004 mg/kg given 30–60 minutes prior to the anticipated time of induction of anesthesia or at the time other preanesthetic medications (e.g., opiates, sedatives) are administered.365
Children 1 month to 2 years of age may require dose of up to 0.009 mg/kg.365
Intraoperatively to Prevent Cholinergic Effects
IV0.004 mg/kg (maximum 0.1 mg); may repeat as needed at intervals of 2–3 minutes.365 However, intraoperative doses rarely are needed in children because of long duration of antimuscarinic effects of preoperative dose.365
Muscarinic Blockade during Anticholinesterase Reversal of Curariform Neuromuscular Blockade
IV0.2 mg for each 1 mg of neostigmine methylsulfate or 5 mg of pyridostigmine bromide.365
To minimize the appearance of adverse cardiac effects, administer glycopyrrolate simultaneously (e.g., mixed in the same syringe) with the anticholinesterase agent.365
If bradycardia is present, administer before the anticholinesterase agent to increase pulse to 80 bpm.a
Adults
COPD
Glycopyrrolate
Oral Inhalation (Powder)15.6 mcg (contents of one capsule) twice daily.368
Oral Inhalation (Solution)25 mcg (contents of one single-dose vial) twice daily.369
Glycopyrrolate/Formoterol Fixed Combination
Oral Inhalation (Aerosol)18 mcg of glycopyrrolate and 9.6 mcg of formoterol fumarate (2 inhalations of a preparation containing 9 mcg of glycopyrrolate/4.8 mcg of formoterol fumarate) twice daily.371
Glycopyrrolate/Indacaterol Fixed Combination:
Oral Inhalation (Powder)15.6 mcg of glycopyrrolate and 27.5 mcg of indacaterol (contents of one capsule) twice daily.370
Peptic Ulcer Disease
Oral (Tablets)
Initially, 1 mg 3 times daily (morning, early afternoon, and bedtime); may increase bedtime dose to 2 mg if needed to control overnight symptoms.366
Alternatively, 2 mg given 2 or 3 times daily at equally spaced intervals.366
Maintenance dosage of 1 mg twice daily adequate in most adults.366
Adjust dosage carefully according to individual requirements and response.366
IV or IM
0.1 mg administered at 4-hour intervals 3 or 4 times daily.365
0.2 mg may be given when a more profound antimuscarinic effect is desired.365
Some patients may need only a single dose; patient response dictates frequency of administration, up to a maximum of 4 times daily.365
Surgery
Preoperatively to Decrease Secretions and Block Cardiac Vagal Reflexes
IM0.004 mg/kg given 30–60 minutes prior to the anticipated time of induction of anesthesia or at the time other preanesthetic medications (e.g., opiates, sedatives) are administered.365
Intraoperatively to Prevent Cholinergic Effects
IVUsual dose is 0.1 mg; may repeat as needed at intervals of 2–3 minutes.365
Muscarinic Blockade during Anticholinesterase Reversal of Curariform Neuromuscular Blockade
IV0.2 mg for each 1 mg of neostigmine methylsulfate or 5 mg of pyridostigmine bromide.365
To minimize the appearance of adverse cardiac effects, administer glycopyrrolate simultaneously (e.g., mixed in the same syringe) with the anticholinesterase agent.365
If bradycardia is present, administer before the anticholinesterase agent to increase pulse to 80 bpm.a
Prescribing Limits
Pediatric Patients
Drooling
Oral (Solution)
Maximum 0.1 mg/kg 3 times daily (≤1.5–3 mg per dose based upon weight).367
Adults
COPD
Glycopyrrolate
Oral Inhalation (Powder)Maximum 15.6 mcg (contents of one capsule) twice daily.368
Oral Inhalation (Solution)Maximum 25 mcg (contents of one single-dose vial) twice daily.369
Glycopyrrolate/Formoterol Fixed Combination
Oral Inhalation (Aerosol)Maximum 18 mcg of glycopyrrolate and 9.6 mcg of formoterol fumarate twice daily.371
Glycopyrrolate/Indacaterol Fixed Combination
Oral Inhalation (Powder)Maximum 15.6 mcg of glycopyrrolate and 27.5 mcg of indacaterol (contents of one capsule) twice daily.370
Peptic Ulcer Disease
Oral (Tablets)
IV or IM
Special Populations
Hepatic Impairment
IM or IV: Manufacturer makes no dosage recommendations.365
Oral (solution or tablets): Manufacturers make no dosage recommendations.366 367
Oral inhalation (powder or solution): No dosage adjustment needed for hepatic impairment.368 369
Renal Impairment
IM or IV: Dosage reduction may be necessary.365 (See Renal Impairment under Cautions.)
Oral inhalation (powder or solution): No dosage adjustment needed in patients with mild to moderate renal impairment.368 369 (See Renal Impairment under Cautions.)
Geriatric Patients
IM or IV: Select dosage with caution because of age-related decreases in hepatic, renal, and/or cardiac function and concomitant disease and drug therapy.365
Oral inhalation (powder or solution): No dosage adjustment needed.368 369
Cautions for Glycopyrrolate
Contraindications
- Oral, IM, IV, and Oral Inhalation:
-
Known hypersensitivity to glycopyrrolate or any ingredient in the formulation.365 366 368 369 370
- Oral Therapy and Prolonged Parenteral Therapy (e.g., for Treatment of Peptic Ulcer)
-
Obstructive uropathy (e.g., bladder neck obstruction secondary to prostatic hypertrophy).365 366 b
-
Obstructive GI disease (e.g., pyloroduodenal stenosis, achalasia).365 366 b
-
Intestinal atony (especially in geriatric and debilitated patients).365 366 b
-
Toxic megacolon complicating ulcerative colitis.365 366 367 b
-
Acute hemorrhage when cardiovascular status is unstable.365 366 367 b
-
Myasthenia gravis365 366 367 b (unless used to reduce adverse muscarinic effects of an anticholinesterase agent such as neostigmine).b
-
Oral solution: Concomitant use of solid dosage forms of potassium chloride.367
- Oral Inhalation
-
Glycopyrrolate/indacaterol and glycopyrrolate/formoterol fixed combinations: Patients with asthma without concomitant use of a long-term asthma controller therapy.370 371
Warnings/Precautions
Warnings
Overdosage
Avoid overdosage. Potential risk of curariform neuromuscular blockade resulting in muscle weakness or paralysis with overdosage.365 366 b
Thermoregulatory Effects
Presence of fever, exposure to high environmental temperatures, and/or physical exertion may result in heat prostration due to decreased sweating, particularly in children and geriatric patients.365 366 367 b
CNS Effects
Risk of drowsiness.365 366 367 b Performance of activities requiring mental alertness (e.g., operating machinery, driving a motor vehicle) may be impaired.365 366 367 b
Intestinal Obstruction
Extreme caution in patients with diarrhea (especially in those with ileostomy or colostomy) because diarrhea may be an early sign of intestinal obstruction.365 366 367 b
Oral solution: Monitor for constipation, especially during first 4–5 days of therapy or after a dosage increase.367 Intestinal pseudo-obstruction reported; may present as abdominal distension, pain, nausea, or vomiting.367
Major Toxicities
Cardiovascular Effects
Caution in cardiac arrhythmias (including tachyarrhythmia), CHF, or CAD365 366 367 since antimuscarinics block vagal inhibition of the SA nodal pacemaker.b Investigate cause of tachycardia before administering glycopyrrolate injection, since an increase in heart rate may occur.365
GI Disorders
Extreme caution in known or suspected GI infections because of decreased GI motility and retention of causative organism and/or toxins.b
Extreme caution in mild to moderate ulcerative colitis; large doses may suppress intestinal motility, resulting in paralytic ileus and toxic megacolon.365 366 367 b
Caution in gastric ulcer because of delayed gastric emptying and possible antral stenosis.365 b
Caution in esophageal reflux and hiatal hernia because of decreased gastric motility and lower esophageal sphincter pressure leading to gastric retention and reflux aggravation.365 366 367 b
GU Disorders
Extreme caution in patients with partial obstructive uropathy or prostatic hypertrophy because of decreased tone and amplitude of contractions of ureters and bladder and resultant urinary retention.365 366 b (See Contraindications under Cautions.)
Oral inhalation (powder or solution): Use with caution in patients with urinary retention.368 369 Be alert for signs and symptoms of urinary retention, especially in patients with prostatic hyperplasia or bladder neck obstruction.368 369
General Precautions
Use of Fixed Combinations
When used in fixed combination with formoterol or indacaterol, consider cautions, precautions, contraindications, and interactions associated with formoterol or indacaterol.370 371
Deterioration of COPD and Acute Episodes
Oral inhalation: Do not initiate in patients with acutely deteriorating COPD, which may be life-threatening.368 369 370 371
Do not use orally inhaled glycopyrrolate for relief of acute symptoms of COPD.368 369 Not studied in patients with acute symptoms; do not use extra doses of the drug in such situations.368 369 Use a short-acting, inhaled β2-agonist as needed for acute symptoms.368 369
Failure to respond to a previously effective dosage of orally inhaled glycopyrrolate or to a supplemental short-acting, inhaled β2-agonist (e.g., increased need for additional short-acting, inhaled β2-agonists) may indicate substantially worsening COPD.368 369 Immediately reevaluate patient and treatment regimen.368 369 Do not use extra or increased dosages of the drug in such situations.368 369
Paradoxical Bronchospasm
Oral inhalation: Possible acute, life-threatening paradoxical bronchospasm.368 369 If paradoxical bronchospasm occurs, treat with a short-acting, inhaled β2-agonist; immediately discontinue therapy and institute alternative therapy.368 369
Sensitivity Reactions
Oral inhalation: Immediate hypersensitivity reactions (e.g., angioedema) may occur.368 369 If hypersensitivity reactions (especially angioedema, urticaria, rash) occurs, discontinue the drug immediately and consider alternative therapy.368 369 Use glycopyrrolate and glycopyrrolate/indacaterol oral inhalation powder with caution in patients with severe hypersensitivity to milk proteins.368 370
Neuropathy
Caution in patients with autonomic neuropathy.365 366 367 b
Down Syndrome, Spastic Paralysis, and Brain Damage
Increased sensitivity to antimuscarinic effects (e.g., mydriasis, positive chronotropic effect).365 b
Hypertension
Caution in hypertensive patients.365 366 367 b
Hyperthyroidism
Caution in hyperthyroid patients.365 366 367 b
Ophthalmic Effects
Blurred vision or sensitivity of the eyes to light may occur.365 366 b
Oral inhalation: Use with caution in patients with narrow-angle glaucoma.368 369 Be alert for signs and symptoms of acute narrow-angle glaucoma.368 369
Specific Populations
Pregnancy
IM or IV: Category B.365 Use during pregnancy only if clearly needed.365
Oral: No controlled studies to date to establish safety during pregnancy;366 367 weigh potential benefits against risks.366
Oral inhalation: Category C.368 370 371 No adequate and well-controlled studies in pregnant women;368 369 370 371 use during pregnancy only if potential benefits outweigh risks.368 369 370 371
Lactation
Not known whether glycopyrrolate is distributed into milk, affects milk production, or affects the breast-fed infant.365 366 367 368 369 Distribution of drug and its metabolites into milk reported in rats.368 369
Like other anticholinergics, may suppress lactation.365 366
Use caution in nursing women.365 368 Consider benefits of breast-feeding and importance of the drug to the woman along with potential adverse effects to the breast-fed infant from the drug or from the underlying maternal condition.367 369
Oral inhalation: Discontinue nursing or the drug.368 370 371
Pediatric Use
Oral (solution): Safety and efficacy not established in pediatric patients <3 years of age.367
Oral (tablets), IM, or IV: Manufacturers state safety and efficacy not established in pediatric patients (including safety and efficacy for treatment of peptic ulcer disease in pediatric patients).365 366 Use with caution; infants and young children may be more susceptible to antimuscarinic effects.365 b Patients with Down syndrome and children with spastic paralysis or brain damage may be hypersensitive to antimuscarinic effects (e.g., mydriasis, positive chronotropic effect).365 b
Oral inhalation: Manufacturers state safety and efficacy not established in pediatric patients.368 369 370 371
IV: Dysrhythmias reported in pediatric patients receiving IV glycopyrrolate preoperatively or during anesthesia.365
IV: Large amounts of benzyl alcohol (i.e., 100–400 mg/kg daily) associated with toxicity in neonates;359 360 361 362 363 364 each mL of glycopyrrolate injection contains 9 mg of benzyl alcohol.365 Manufacturer does not recommend use in neonates;365 AAP states that the presence of small amounts of this preservative in a commercially available injection should not proscribe its use when indicated in neonates.359
Geriatric Use
Oral, IM, or IV: Use with caution;365 366 b possible increased susceptibility to the adverse effects of antimuscarinics.365 b
Oral inhalation: No overall differences in safety and efficacy observed between patients ≥65 years of age and younger adults.368 369 370 371 No dosage adjustments needed.368 369 370 371
Hepatic Impairment
Oral, IM, or IV: Use with caution.365 366 b
Oral inhalation (powder or solution): No dosage adjustments needed in patients with mild to moderate hepatic impairment.368 369 370 Not studied in those with severe hepatic impairment.370
Oral inhalation (aerosol): Monitor closely.371
Renal Impairment
Oral, IM, or IV: Use with caution.365 366 367 b Elimination may be severely impaired.365 367 Dosage reduction may be necessary.365
Oral inhalation (powder or solution): Glycopyrrolate exposure may be increased in patients with severe renal impairment.368 370 Use in those with severe renal impairment or end-stage renal disease requiring dialysis only if expected benefits outweigh potential risks.368 370 No dosage adjustment needed in patients with mild to moderate renal impairment.368 369 370
Oral inhalation (aerosol): Use in patients with severe renal impairment or end-stage renal disease requiring dialysis only if expected benefit outweighs potential risk.371
Common Adverse Effects
Oral (tablets), IM, or IV: Xerostomia, decreased sweating, urinary hesitancy and retention, blurred vision, tachycardia, palpitations, dilatation of the pupil, cycloplegia, increased ocular tension, loss of taste, headaches, nervousness, mental confusion, drowsiness, weakness, dizziness, insomnia, nasal congestion, sinusitis, upper respiratory tract infection, constipation, nausea, vomiting, bloated feeling, impotence, allergic reaction, urticaria.365 366 b Ocular and CNS effects are less common with glycopyrrolate than with tertiary amine antimuscarinics.365 366 b
Oral (solution): Dry mouth, vomiting, constipation, flushing, nasal congestion.367
Oral inhalation (powder): Upper respiratory tract infection,368 373 374 375 nasopharyngitis,368 373 374 375 urinary tract infection,368 373 374 375 sinusitis,368 373 374 375 oropharyngeal pain,368 373 374 375 diarrhea,368 374 375 nausea,368 375 upper abdominal pain,368 fatigue,368 375 bronchitis,368 373 374 375 pneumonia,368 373 rhinitis,368 374 nasal congestion,375 back pain,368 374 375 arthralgia,368 dyspnea,368 374 375 wheezing.368
Oral inhalation (solution): Dyspnea, diarrhea, upper respiratory tract infection, peripheral edema, bronchitis, nasopharyngitis, pneumonia, sinusitis, urinary tract infection, back pain, headache, cough, oropharyngeal pain, hypertension.369
Drug Interactions
Orally Administered Drugs
Potential pharmacokinetic interaction (altered GI absorption of various drugs); antimuscarinics may inhibit GI motility, delay gastric emptying, and prolong GI transit time.b
Specific Drugs
|
Drug |
Interaction |
Comments |
|---|---|---|
|
β2-Adrenergic agonists |
Glycopyrrolate oral inhalation: No interactions reported368 369 |
|
|
Amantadine |
Use concomitantly with caution;b consider reducing dosage of glycopyrrolate367 |
|
|
Antacids |
Possible decreased absorption of antimuscarinicb |
Administer oral glycopyrrolate at least 1 hour before antacidsb |
|
Antiarrhythmic agents (quinidine, disopyramide, procainamide) |
Possible additive anticholinergic effectsb |
Use concomitantly with cautionb |
|
Anticholinergic drugs |
Glycopyrrolate oral inhalation: Avoid concomitant use with other anticholinergic-containing drugs368 369 |
|
|
Antidepressants, tricyclic |
Use concomitantly with cautionb |
|
|
Antihistamines (meclizine) |
Possible additive anticholinergic effectsb |
Use concomitantly with cautionb |
|
Antiparkinsonian agents |
Use concomitantly with cautionb |
|
|
Atenolol |
Possible increased bioavailability of atenolol367 |
May need to reduce atenolol dosage367 |
|
Cimetidine |
Possible increase in glycopyrrolate exposure368 |
|
|
Corticosteroids |
Possible increased IOPb Glycopyrrolate oral inhalation: No interactions reported with oral or inhaled corticosteroids368 369 |
|
|
Digoxin |
Digoxin slow dissolution tablets: Possible increased concentrations and effects of digoxin367 |
Monitor for increased digoxin concentrations; consider alternative digoxin dosage forms (e.g., capsules, elixir)367 |
|
Haloperidol |
Possible decreased haloperidol concentrations; possible worsening of schizophrenic symptoms and development of tardive dyskinesia367 |
Closely monitor if concomitant use cannot be avoided367 |
|
Ketoconazole |
Possible decreased ketoconazole absorptionb |
If concomitant therapy is necessary, give antimuscarinic at least 2 hours after ketoconazoleb |
|
Levodopa |
Possible increased gastric metabolism of levodopa and decreased levodopa absorption in the small intestine367 b |
Toxicity may result from increased levodopa absorption if antimuscarinic is discontinued without a concomitant reduction in levodopa dosageb Consider increasing levodopa dosage when glycopyrrolate therapy initiated367 |
|
Meperidine |
Possible additive anticholinergic effectsb |
Use concomitantly with cautionb |
|
Metformin |
Possible increase in metformin concentrations and effects367 |
Monitor clinical response to metformin and reduce dosage if needed367 |
|
Methylxanthines |
Glycopyrrolate oral inhalation: No interactions reported368 |
|
|
Phenothiazines |
Use concomitantly with cautionb |
|
|
Potassium chloride |
Glycopyrrolate may potentiate potassium chloride’s local GI mucosal effects365 b Glycopyrrolate oral solution: Passage of potassium chloride tablets through the GI tract may be arrested or delayed367 |
Use glycopyrrolate cautiously with potassium chloride preparations (especially wax-matrix preparations); monitor carefully for evidence of GI mucosal lesionsb Glycopyrrolate oral solution: Concomitant use with solid oral dosage forms of potassium chloride contraindicated367 |
|
Skeletal muscle relaxants |
Possible additive anticholinergic effectsb |
Use concomitantly with cautionb |
Glycopyrrolate Pharmacokinetics
Absorption
Bioavailability
Incompletely absorbed from the GI tract.367 a b
Following oral administration of glycopyrrolate tablets in children, mean absolute bioavailability was low (about 3%) and variable (range: 1–13%).367
Following oral administration of glycopyrrolate solution, mean time to peak concentrations is about 3 hours.367
Rapidly absorbed following IM injection.b
Following oral inhalation of glycopyrrolate powder via the Neohaler device, drug is rapidly absorbed with peak plasma concentrations at 5 minutes.368 Absolute bioavailability of about 40%; 90% of systemic exposure resulting from lung absorption and 10% from GI absorption.368 Steady-state concentrations achieved within 1 week following repeated once-daily inhalation; no evidence of changes in pharmacokinetics over time.368 Linear pharmacokinetics observed following inhalation of 31.2–249.6 mcg daily.368
Following oral inhalation of glycopyrrolate solution via the Magnair nebulizer system, drug is rapidly absorbed with peak plasma concentrations occurring within 20 minutes.369 Steady-state concentrations achieved within 1 week of treatment initiation; 2- to 3-fold accumulation of systemic drug exposure observed at steady state following twice-daily dosing.369
Onset
Following IV administration, onset of action generally occurs within 1 minute.365 a
Following IM injection, effects are evident within 15–30 minutes and peak within 30–45 minutes.365 a
Duration
Following oral administration, anticholinergic effects may persist for up to 8–12 hours.a
Following parenteral administration, vagal blocking effects persist for 2–3 hours and the antisialogue effects persist up to 7 hours.365 a
Effect of Food
Oral solution: Administration with a high-fat meal decreases absorption.367
Distribution
Extent
Rapidly distributed throughout the body with highest concentrations in the stomach and intestine following IV administration in animals.a b
Does not readily cross lipid membranes;365 366 does not readily cross the blood-brain barrier or penetrate the eye.365 366 b
Glycopyrrolate crosses the placenta to a limited extent; not known whether distributed into milk.365 366
Plasma Protein Binding
38–41% at concentrations of 1–10 ng/mL in vitro.368 369
Elimination
Metabolism
Small amounts are metabolized to one or more metabolites.367 a
Orally inhaled glycopyrrolate: In vitro studies show hydroxylation resulting in a variety of mono- and bis-hydroxylated metabolites and direct hydrolysis resulting in formation of a carboxylic acid derivative (M9).368 369
Multiple CYP isoenzymes appear to contribute to oxidative biotransformation of glycopyrrolate; hydrolysis to M9 likely catalyzed by members from the cholinesterase family presystemically and/or via first- pass metabolism from the swallowed dose fraction of orally inhaled drug.368 369
Elimination Route
Excreted principally as unchanged drug in feces via biliary excretion and in urine.365 a In adults, approximately 65–80% of an IV dose eliminated in urine as unchanged drug.367
Following repeated oral inhalation, glucuronide and/or sulfate conjugates found in urine, accounting for about 3% of inhaled dose.368
Renal elimination of parent drug accounts for about 60–70% of systemically available glycopyrrolate following oral inhalation; active tubular secretion contributes to renal clearance.368 369 Most nonrenal clearance believed to result from metabolism, with biliary clearance contributing a small role.368 369
Half-life
IV: About 50 minutes in adults, 19–99 minutes in children, and 22–130 minutes in infants.365
IM: About 33–75 minutes.365
Oral solution: About 3 hours.367
Oral inhalation powder: 33–53 hours.368
Special Populations
In patients undergoing renal transplantation, half-life of IV glycopyrrolate is prolonged to 47 minutes compared with 19 minutes in healthy individuals.365
Systemic exposure increased in patients with renal failure.367 368
Oral inhalation powder: Systemic exposure increased by 1.4-fold in patients with mild to moderate renal failure and 2.2-fold in those with severe renal impairment and end-stage renal disease.368
Oral inhalation solution: Effects of renal impairment on pharmacokinetics not studied to date.369
Pharmacokinetics not evaluated in patients with hepatic impairment.367 368
Oral inhalation powder: Age, body weight, race, gender, or smoking status did not produce clinically relevant effects on systemic drug exposure.368
Oral inhalation solution: Age, body weight, or race did not produce clinically relevant effects on systemic drug exposure.369
Stability
Storage
Oral Inhalation
Aerosol
Glycopyrrolate/formoterol: 20–25°C (may be exposed to 15–30°C).371 Discard 3 months after foil pouch opened or when dose indicator reads “0”, whichever comes first.371
Powder
Glycopyrrolate and glycopyrrolate/indacaterol: 25°C (may be exposed to 15–30°C).368 370
Keep dry-powder capsules in the foil-sealed blisters until immediately before use.368 370 Remove one capsule immediately before use.368 370 Discard capsules if opened and exposed to air (i.e., not used immediately).368 370
Solution
Glycopyrrolate: 20–25°C.369
Store single-dose vials in protective foil pouch.369 After opening pouch, return unused vials to pouch for storage; discard any vials not used within 7 days of opening pouch.369 Discard vials containing solution that is not colorless.369
Oral
Solution
20–25°C (may be exposed to 15–30°C).367
Tablets
20–25°C in tight containers (may be exposed to 15–30°C).366
Parenteral
Injection
20–25°C.365
Compatibility
Parenteral
Solution Compatibility
If the pH of the admixture is >6, rapid ester hydrolysis of glycopyrrolate generally occurs.365 a
|
Dextrose 5% in sodium chloride 0.45% |
|
Dextrose 5 or 10% in water |
|
Ringer’s injection |
|
Sodium chloride 0.9% |
|
Ringer’s injection, lactated |
Drug Compatibility
Generally incompatible with drugs that have a pH >6.365 a If the pH of the admixture is >6, rapid ester hydrolysis of glycopyrrolate generally occurs.a HID
|
Compatible |
|---|
|
Buprenorphine HCl with haloperidol lactate |
|
Incompatible |
|
Methylprednisolone sodium succinate |
|
Compatible |
|---|
|
Propofol |
|
Palonosetron HCl |
|
Compatible |
|---|
|
Atropine sulfate |
|
Buprenorphine HCl with haloperidol lactate |
|
Butorphanol tartrate |
|
Chlorpromazine HCl |
|
Codeine phosphate |
|
Diphenhydramine HCl |
|
Droperidol |
|
Fentanyl citrate |
|
Hydromorphone HCl |
|
Hydroxyzine HCl |
|
Levorphanol tartrate |
|
Lidocaine HCl |
|
Meperidine HCl |
|
Midazolam HCl |
|
Morphine sulfate |
|
Nalbuphine HCl |
|
Neostigmine methylsulfate |
|
Ondansetron HCl |
|
Oxymorphone HCl |
|
Physostigmine salicylate |
|
Procaine HCl (no longer commercially available in US) |
|
Prochlorperazine edisylate |
|
Promethazine HCl |
|
Pyridostigmine bromide |
|
Ranitidine HCl |
|
Scopolamine HBr |
|
Trimethobenzamide HCl |
|
Incompatible |
|
Chloramphenicol sodium succinate |
|
Dexamethasone sodium phosphate |
|
Diazepam |
|
Dimenhydrinate |
|
Methohexital sodium |
|
Pentazocine lactate |
|
Pentobarbital sodium |
|
Secobarbital sodium |
|
Sodium bicarbonate |
|
Thiopental sodium (no longer commercially available in US) |
Actions
-
Glycopyrrolate competitively inhibits acetylcholine or other cholinergic stimuli at autonomic effectors innervated by postganglionic cholinergic nerves and, to a lesser extent, on smooth muscles that lack cholinergic innervation.365 366 367 368 b
-
At usual doses, principally antagonizes cholinergic stimuli at muscarinic receptors and has little or no effect on cholinergic stimuli at nicotinic receptors.b
-
At high doses, may produce substantial ganglionic blockade with resultant adverse effects (e.g., impotence, postural hypotension); in overdosage, may cause curariform neuromuscular blockade.b
-
Antimuscarinics also referred to as anticholinergics (cholinergic blocking agents), but this term is appropriate only when it describes the antagonism of cholinergic stimuli at any cholinergic receptor, whether muscarinic or nicotinic.b
-
Also referred to as parasympatholytics since the antagonized functions principally are under the parasympathetic division of the nervous system.b
-
Receptors at various sites are not equally sensitive to inhibition of muscarinic effects.b Relative sensitivity of physiologic functions (proceeding from the most sensitive) is as follows: secretions of the salivary, bronchial, and sweat glands; pupillary dilation; ocular accommodation, and heart rate; contraction of the detrusor muscle of the bladder and smooth muscle of the GI tract; and gastric secretion and motility.b Doses used to decrease gastric secretions are likely to cause dryness of the mouth (xerostomia) and interfere with visual accommodation, and possibly cause difficulty in urinating.b
-
Competitively and reversibly inhibits the actions of acetylcholine and other cholinergic stimuli at M3 receptors in the smooth muscle of the respiratory tract resulting in bronchodilation.368 369
Advice to Patients
-
A copy of the manufacturer's patient information (medication guide) and instructions for use must be provided to all patients each time glycopyrrolate for oral inhalation (alone or in fixed combination with formoterol or indacaterol) is dispensed.368 369 370 371 Importance of instructing patients to read the patient information and instructions for use prior to initiation of therapy and each time the prescription is refilled.368 369 370 371
-
Importance of understanding proper storage, preparation, and inhalation techniques, including use of the drug-specific oral inhalation device.368 369 370 371
-
When using glycopyrrolate or glycopyrrolate/indacaterol dry-powder capsules for oral inhalation, importance of advising patients not to swallow the capsules or to use them with any capsule inhaler other than the Neohaler device.368 370 Importance of advising patients to use the new inhaler handset provided with each new prescription.368 370
-
Importance of adherence to oral inhalation dosing schedules, including not altering the dose or frequency of use of such drugs, unless otherwise instructed by a clinician.368 369 370 371
-
Advise patients that if an oral inhalation dose of glycopyrrolate alone or in fixed combination with formoterol or indacaterol is missed, the next dose should be taken at the regularly scheduled time; importance of not using more than one capsule or vial at a time or more than 2 capsules or vials in one day or using inhaler more frequently than recommended.368 369 370 371
-
Advise patients that oral inhalation therapy with glycopyrrolate alone or in fixed combination with formoterol or indacaterol does not relieve acute COPD symptoms; importance of not using extra doses for such symptoms.368 369 370 371
-
Importance of all patients being provided with and instructed in the use of a short-acting, inhaled β2-adrenergic agonist (e.g., albuterol) for treatment of acute COPD symptoms.368 369 370 371
-
When initiating oral inhalation therapy with glycopyrrolate in fixed combination with formoterol or indacaterol, importance of discontinuing regular use of short-acting, inhaled β2-agonists and using them only to relieve acute symptoms.370 371
-
Importance of contacting a clinician immediately if symptoms worsen or the short-acting, inhaled β2-agonist becomes less effective or more inhalations than usual are required to relieve symptoms.368 369 370 371
-
Importance of patients not discontinuing oral inhalation therapy without medical supervision, since symptoms may recur after discontinuance.368 369 370 371
-
Advise patients of the risk of paradoxical bronchospasm with use of oral inhalation therapy.368 369 370 371 If paradoxical bronchospasm occurs, discontinue the drug.368 369 370 371
-
When oral inhalation therapy with glycopyrrolate in fixed combination with formoterol or indacaterol is used, importance of informing patients of important cautionary information about formoterol or indacaterol.370 371
-
When glycopyrrolate oral solution is used, important of administering the oral solution at least 1 hour before or 2 hours after meals.367 Importance of using an accurate measuring device to administer the oral solution.367
-
Importance of not increasing the dosage of glycopyrrolate oral solution without contacting a clinician.367
-
Advise patients or caregivers that if troublesome adverse effects develop following a dosage increase of glycopyrrolate oral solution, importance of returning to the previous dosage and contacting a clinician.367
-
Advise patients that urinary hesitancy or retention may occur;365 366 367 368 b importance of contacting a clinician immediately if signs or symptoms of urinary retention (e.g., difficulty passing urine, painful urination) occur.368 369 370 371
-
Advise patients that dry mouth365 366 367 b or sensitivity of eyes to light365 b may occur.
-
Importance of contacting a clinician immediately if signs or symptoms of acute narrow-angle glaucoma (e.g., eye pain or discomfort, blurred vision, visual halos or colored images in association with red eyes from conjunctival congestion or corneal edema) occur.368 369 370 371
-
Importance of advising patients that constipation, vomiting, or flushing of the skin or face may occur.367 If constipation occurs in a patient receiving glycopyrrolate oral solution, importance of discontinuing the drug and contacting a clinician.367
-
Importance of advising patients that if rash, hives, or allergic reaction occurs during therapy with glycopyrrolate oral solution, discontinue the drug and contact a clinician.367
-
Risk of hyperthermia and heat prostration;365 366 367 b importance of advising patients to avoid exposure to high environmental temperatures and avoid use when febrile.367
-
Risk of dizziness, drowsiness, or blurred vision;365 366 367 b importance of advising patients to avoid activities requiring mental alertness and/or visual acuity (e.g., driving, operating machinery, hazardous work) until effects on individual are known.365 366 367 b
-
Importance of informing clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs, as well as any concomitant illnesses.365 366 367 368 369 370 371
-
Importance of women informing clinicians if they are or plan to become pregnant or plan to breast-feed.365 366 368 369 370 371
-
Importance of informing patients of other important precautionary information.365 366 367 368 369 370 371 (See Cautions.)
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Solution |
0.2 mg/mL |
Cuvposa |
Merz |
|
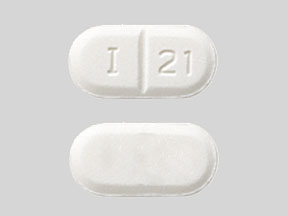
Tablets |
1 mg* |
Glycopyrrolate Tablets |
||
|
Robinul (scored) |
Shionogi |
|||
|
2 mg* |
Glycopyrrolate Tablets |
|||
|
Robinul Forte (scored) |
Shionogi |
|||
|
Oral Inhalation |
Powder, for inhalation (contained in capsules) |
15.6 mcg |
Seebri Neohaler |
Sunovion |
|
Solution, for nebulization |
25 mcg/mL |
Lonhala Magnair |
Sunovion |
|
|
Parenteral |
Injection |
0.2 mg/mL* |
Robinul |
West-ward |
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral Inhalation |
Aerosol |
9 mcg with Formoterol Fumarate 4.8 mcg per metered spray |
Bevespi Aerosphere (with hydrofluoroalkane propellant) |
AstraZeneca |
|
Powder, for inhalation (contained in capsules) |
15.6 mcg with Indacaterol 27.5 mcg |
Utibron Neohaler |
Sunovion |
AHFS DI Essentials™. © Copyright 2024, Selected Revisions December 2, 2012. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
† Off-label: Use is not currently included in the labeling approved by the US Food and Drug Administration.
References
Only references cited for selected revisions after 1984 are available electronically.
359. American Academy of Pediatrics Committee on Fetus and Newborn and Committee on Drugs. Benzyl alcohol: toxic agent in neonatal units. Pediatrics. 1983; 72:356-8. http://www.ncbi.nlm.nih.gov/pubmed/6889041?dopt=AbstractPlus
360. Anon. Benzyl alcohol may be toxic to newborns. FDA Drug Bull. 1982; 12(2):10-1.
361. Centers for Disease Control. Neonatal deaths associated with use of benzyl alcohol. MMWR Morb Mortal Wkly Rep. 1982; 31:290-1. http://www.ncbi.nlm.nih.gov/pubmed/6810084?dopt=AbstractPlus
362. Gershanik J, Boecler B, Ensley H et al. The gasping syndrome and benzyl alcohol poisoning. N Engl J Med. 1982; 307:1384-8. http://www.ncbi.nlm.nih.gov/pubmed/7133084?dopt=AbstractPlus
363. Menon PA, Thach BT, Smith CH et al. Benzyl alcohol toxicity in a neonatal intensive care unit: incidence, symptomatology, and mortality. Am J Perinatol. 1984; 1:288-92. http://www.ncbi.nlm.nih.gov/pubmed/6440575?dopt=AbstractPlus
364. Anderson CW, Ng KJ, Andresen B et al. Benzyl alcohol poisoning in a premature newborn infant. Am J Obstet Gynecol. 1984; 148:344-6. http://www.ncbi.nlm.nih.gov/pubmed/6695984?dopt=AbstractPlus
365. West-ward Pharmaceuticals. Robinul (glycopyrrolate) injection prescribing information. Eatontown, NJ; 2011 Dec.
366. Shionogi Inc. Robinul (glycopyrrolate) and Robinul Forte (glycopyrrolate) tablets prescribing information. Florham Park, NJ; 2011 Dec.
367. Merz Pharmaceuticals, LLC. Cuvposa (glycopyrrolate) oral solution prescribing information. Raleigh, NC; 2016 May.
368. Sunovion Pharmaceuticals, Inc. Seebri Neohaler (glycopyrrolate) inhalation powder prescribing information. Marlborough, MA; 2017 Jul.
369. Sunovion Pharmaceuticals, Inc. Lonhala Magnair (glycopyrrolate) inhalation solution prescribing information. Marlborough, MA; 2017 Dec.
370. Sunovion Pharmaceutials, Inc. Utibron Neohaler (indacaterol/glycopyrrolate) inhalation powder prescribing information. Marlborough, MA; 2017 May.
371. AstraZeneca Pharmaceuticals LP. Bevespi Aerosphere (glycopyrrolate and formoterol fumarate) inhalation aerosol prescribing information. Wilmington, DE; 2017 Jun.
372. Parr JR, Todhunter E, Pennington L et al. Drooling Reduction Intervention randomised trial (DRI): comparing the efficacy and acceptability of hyoscine patches and glycopyrronium liquid on drooling in children with neurodisability. Arch Dis Child. 2018; 103:371-376. http://www.ncbi.nlm.nih.gov/pubmed/29192000?dopt=AbstractPlus
373. LaForce C, Feldman G, Spangenthal S et al. Efficacy and safety of twice-daily glycopyrrolate in patients with stable, symptomatic COPD with moderate-to-severe airflow limitation: the GEM1 study. Int J Chron Obstruct Pulmon Dis. 2016; 11:1233-43. http://www.ncbi.nlm.nih.gov/pubmed/27354782?dopt=AbstractPlus
374. Kerwin E, Siler TM, Korenblat P et al. Efficacy and Safety of Twice-Daily Glycopyrrolate Versus Placebo in Patients With COPD: The GEM2 Study. Chronic Obstr Pulm Dis. 2016; 3:549-559. http://www.ncbi.nlm.nih.gov/pubmed/28848879?dopt=AbstractPlus
375. Mahler DA, Gifford AH, Satti A et al. Long-term safety of glycopyrrolate: A randomized study in patients with moderate-to-severe COPD (GEM3). Respir Med. 2016; 115:39-45. http://www.ncbi.nlm.nih.gov/pubmed/27215502?dopt=AbstractPlus
376. Mahler DA, Kerwin E, Ayers T et al. FLIGHT1 and FLIGHT2: Efficacy and Safety of QVA149 (Indacaterol/Glycopyrrolate) versus Its Monocomponents and Placebo in Patients with Chronic Obstructive Pulmonary Disease. Am J Respir Crit Care Med. 2015; 192:1068-79. http://www.ncbi.nlm.nih.gov/pubmed/26177074?dopt=AbstractPlus
377. Martinez FJ, Rabe KF, Ferguson GT et al. Efficacy and Safety of Glycopyrrolate/Formoterol Metered Dose Inhaler Formulated Using Co-Suspension Delivery Technology in Patients With COPD. Chest. 2017; 151:340-57. http://www.ncbi.nlm.nih.gov/pubmed/27916620?dopt=AbstractPlus
a. AHFS drug information. McEvoy GK, ed. Glycopyrrolate. Bethesda, MD: American Society of Health-System Pharmacists.
b. AHFS drug information 2006. McEvoy GK, ed. Antimuscarinics/antispasmodics general statement. Bethesda, MD: American Society of Health-System Pharmacists; 2006:1257-1264.
HID. McEvoy, GK, ed. Handbook on injectable drugs. 20th ed. Bethesda, MD: American Society of Health-System Pharmacists; 2018:661-6.
More about glycopyrrolate
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (18)
- Drug images
- Side effects
- Dosage information
- During pregnancy
- Drug class: anticholinergic bronchodilators
- Breastfeeding
Patient resources
Professional resources
- Glycopyrrolate Injection prescribing information
- Glycopyrrolate Oral Solution (FDA)
- Glycopyrrolate Tablets (FDA)
Other brands
Robinul, Cuvposa, Seebri Neohaler, Dartisla ODT, ... +2 more