Doravirine (Monograph)
Brand name: Pifeltro
Drug class: HIV Nonnucleoside Reverse Transcriptase Inhibitors
Introduction
Antiretroviral; HIV nonnucleoside reverse transcriptase inhibitor (NNRTI).
Uses for Doravirine
Treatment of HIV Infection
Used in conjunction with other antiretroviral agents (including as a fixed combination with lamivudine and tenofovir disoproxil fumarate [TDF]) for the treatment of HIV-1 infection in adults and pediatric patients weighing ≥35 kg who are antiretroviral-naive (have not previously received antiretroviral therapy) or to replace a current antiretroviral regimen in patients who are virologically suppressed (HIV-1 RNA <50 copies/mL) with no history of treatment failure and no known substitutions associated with resistance to doravirine.
Commonly used in NNRTI-based regimens that include doravirine and 2 HIV NRTIs; consult guidelines for the most current information on recommended regimens.
Selection of an initial ARV regimen should be individualized based on factors such as virologic efficacy, toxicity, pill burden, dosing frequency, drug-drug interaction potential, resistance test results, comorbid conditions, access, and cost.
Doravirine Dosage and Administration
General
Pretreatment Screening
-
Consider potential for drug interactions prior to, and during treatment with doravirine. Review concomitant medications to assess for drug interactions.
Dispensing and Administration Precautions
-
The Institute for Safe Medication Practices (ISMP) list of error-prone abbreviations, symbols, and dose designations states that the use of abbreviations for antiretroviral medications (e.g., DOR, TAF, TDF) during the medication use process should be avoided as their use has been associated with serious medication errors.
Administration
Oral Administration
Administer orally once daily without regard to food.
Must use single-entity doravirine in conjunction with other antiretrovirals.
Also commercially available in fixed-combination tablets containing doravirine, lamivudine, and tenofovir disoproxil fumarate (doravirine/lamivudine/tenofovir DF; Delstrigo).
Dosage
Pediatric Patients
HIV Infection
Oral
Pediatric patients ≥35 kg: 100 mg once daily.
Pediatric patients ≥35 kg receiving concomitant rifabutin: 100 mg twice daily (12 hours apart).
Adults
HIV Infection
Oral
100 mg once daily.
In patients receiving concomitant rifabutin, increase dosage to 100 mg twice daily (12 hours apart).
Special Populations
Hepatic Impairment
Mild or moderate hepatic impairment (Child-Pugh class A or B): Dosage adjustments not needed.
Severe hepatic impairment (Child-Pugh class C): Not studied.
Renal Impairment
Mild, moderate, or severe renal impairment: Dosage adjustments not needed.
Not adequately studied in patients with end-stage renal disease; not studied in those receiving dialysis.
Geriatric Patients
No specific dosage recommendations; use with caution.
Cautions for Doravirine
Contraindications
-
Concomitant use with potent CYP3A inducers (e.g., carbamazepine, oxcarbazepine, phenobarbital, phenytoin, enzalutamide, rifampin, rifapentine, mitotane, St. John’s wort [Hypericum perforatum]).
Warnings/Precautions
Severe Skin Reactions
Severe skin reactions, including Stevens-Johnson syndrome/toxic epidermal necrolysis, reported. Discontinue doravirine and other medications associated with severe skin reactions if a painful rash with mucosal involvement or a progressive severe rash develops. Monitor patients closely and initiate appropriate therapy.
Risk of Adverse Reactions or Loss of Virologic Response Due to Drug Interactions
Concomitant use with certain drugs may result in known or potentially clinically important drug interactions, some of which may lead to loss of therapeutic effect of doravirine and possible development of resistance.
Consider potential for drug interactions prior to and during doravirine therapy; review concomitant drugs during therapy and monitor for adverse effects.
Immune Reconstitution Syndrome
Immune reconstitution syndrome reported in HIV-infected patients receiving multiple-drug antiretroviral therapy. During the initial phase of treatment, HIV-infected patients whose immune systems respond to antiretroviral therapy may develop an inflammatory response to indolent or residual opportunistic infections (e.g., Mycobacterium avium, cytomegalovirus [CMV], Pneumocystis jirovecii [formerly P. carinii], tuberculosis); such responses may necessitate further evaluation and treatment.
Autoimmune disorders (e.g., Graves' disease, polymyositis, Guillain-Barré syndrome, autoimmune hepatitis) also reported in the setting of immune reconstitution; however, time to onset is more variable and can occur many months after initiation of antiretroviral therapy.
Specific Populations
Pregnancy
Antiretroviral Pregnancy Registry at 800-258-4263 or [Web].
Data insufficient to determine if doravirine poses a risk to pregnancy outcomes.
No adverse developmental effects observed in animal studies.
Lactation
Not known whether doravirine distributes into human milk, affects human milk production, or affects the breast-fed infant.
Distributed into milk of lactating rats.
The HHS perinatal HIV transmission guideline provides updated recommendations on infant feeding. The guideline states that patients with HIV should receive evidence-based, patient-centered counseling to support shared decision making about infant feeding. During counseling, patients should be informed that feeding with appropriate formula or pasteurized donor human milk from a milk bank eliminates the risk of postnatal HIV transmission to the infant. Additionally, achieving and maintaining viral suppression with antiretroviral therapy during pregnancy and postpartum reduces the risk of breastfeeding HIV transmission to <1%, but does not completely eliminate the risk. Replacement feeding with formula or banked pasteurized donor milk is recommended when patients with HIV are not on antiretroviral therapy and/or do not have a suppressed viral load during pregnancy (at a minimum throughout the third trimester), as well as at delivery.
Pediatric Use
Safety and efficacy established in pediatric patients weighing ≥35 kg. Safety and efficacy not established in pediatric patients weighing <35 kg.
Geriatric Use
Experience in patients ≥65 years of age insufficient to determine whether they respond differently than younger adults.
Use with caution in geriatric patients because of age-related decreases in hepatic, renal, and/or cardiac function and potential for concomitant disease and drug therapy.
Hepatic Impairment
No clinically important differences in pharmacokinetics in patients with moderate hepatic impairment (Child-Pugh class B); dosage adjustments not needed in those with mild or moderate hepatic impairment (Child-Pugh class A or B).
Not studied in patients with severe hepatic impairment (Child-Pugh class C).
Renal Impairment
Based on population pharmacokinetic analysis, renal function does not have a clinically important effect on pharmacokinetics; dosage adjustments not needed in those with mild, moderate, or severe renal impairment.
Not adequately studied in patients with end-stage renal disease; not studied in those receiving dialysis.
Common Adverse Effects
Most common adverse effects (≥5%): nausea, dizziness, headache, fatigue, diarrhea, abdominal pain, abnormal dreams.
Drug Interactions
Primarily metabolized by CYP3A. Does not inhibit CYP1A2, 2B6, 2C8, 2C9, 2C19, 2D6, or 3A4; not likely to induce CYP1A2, 2B6, or 3A4.
Does not inhibit UGT1A1. Not likely to inhibit P-glycoprotein (P-gp), organic anion transport polypeptide (OATP) 1B1, OATP1B3, bile salt export pump (BSEP), organic anion transporter (OAT) 1, OAT3, organic cation transporter (OCT) 2, multidrug and toxin extrusion transporter (MATE) 1, or MATE2K.
Drugs Affecting or Affected by Hepatic Microsomal Enzymes
Concomitant use with CYP3A inducers may decrease doravirine plasma concentrations and may reduce efficacy.
Concomitant use with CYP3A inhibitors may increase doravirine concentrations.
Not likely to have a clinically important effect on exposures of drugs metabolized by CYP isoenzymes.
Specific Drugs
|
Drug |
Interaction |
Comments |
|---|---|---|
|
Abacavir |
No in vitro evidence of antagonistic antiretroviral effects |
|
|
Antacids |
Antacid containing aluminum hydroxide, magnesium hydroxide, and simethicone: No clinically important pharmacokinetic interactions |
|
|
Anticonvulsants |
Carbamazepine, oxcarbazepine, phenobarbital, phenytoin: Decreased doravirine concentrations expected; possible decreased doravirine efficacy |
Carbamazepine, oxcarbazepine, phenobarbital, phenytoin: Concomitant use contraindicated; do not initiate doravirine until ≥4 weeks after anticonvulsant discontinued |
|
Antimycobacterials ( rifamycins) |
Rifabutin: Decreased doravirine AUC; peak plasma concentrations not affected Rifampin: Decreased doravirine AUC and peak plasma concentrations; possible decreased efficacy of doravirine Rifapentine: Decreased doravirine concentrations expected; possible decreased efficacy of doravirine |
Rifabutin: Increase dosage of doravirine to 100 mg twice daily Rifampin, rifapentine: Concomitant use contraindicated; do not initiate doravirine until ≥4 weeks after rifampin or rifapentine discontinued |
|
Atorvastatin |
No clinically important pharmacokinetic interactions |
|
|
Darunavir |
No in vitro evidence of antagonistic antiretroviral effects |
|
|
Delavirdine |
No in vitro evidence of antagonistic antiretroviral effects |
|
|
Didanosine |
No in vitro evidence of antagonistic antiretroviral effects |
|
|
Dolutegravir |
No clinically important effect on pharmacokinetics of either drug |
|
|
Efavirenz |
On day 1 of doravirine therapy (and after discontinuance of efavirenz), doravirine exposures and peak plasma concentrations decreased by 62 and 35%, respectively; on day 14 of doravirine therapy (and after discontinuance of efavirenz), doravirine exposures and peak plasma concentrations decreased by 32 and 14%, respectively No in vitro evidence of antagonistic antiretroviral effects |
Concomitant use not recommended |
|
Elbasvir and grazoprevir |
No clinically important pharmacokinetic interactions |
|
|
Emtricitabine |
No in vitro evidence of antagonistic antiretroviral effects |
|
|
Enfuvirtide |
No in vitro evidence of antagonistic antiretroviral effects |
|
|
Enzalutamide |
Decreased doravirine concentrations expected; possible decreased doravirine efficacy |
Concomitant use contraindicated; do not initiate doravirine until ≥4 weeks after enzalutamide discontinued |
|
Etravirine |
Decreased doravirine concentrations expected No in vitro evidence of antagonistic antiretroviral effects |
Concomitant use not recommended |
|
Indinavir |
No in vitro evidence of antagonistic antiretroviral effects |
|
|
Ketoconazole |
Increased doravirine exposures and peak plasma concentrations; not considered clinically important |
|
|
Lamivudine |
No clinically important pharmacokinetic interactions No in vitro evidence of antagonistic antiretroviral effects |
|
|
Ledipasvir and sofosbuvir |
No clinically important pharmacokinetic interactions |
|
|
Maraviroc |
No in vitro evidence of antagonistic antiretroviral effects |
|
|
Metformin |
No clinically important effects on metformin concentrations |
|
|
Methadone |
No clinically important effect on pharmacokinetics of either drug |
|
|
Midazolam |
No clinically important pharmacokinetic interactions |
|
|
Mitotane |
Decreased doravirine concentrations expected; possible decreased doravirine efficacy |
Concomitant use contraindicated; do not initiate doravirine until ≥4 weeks after mitotane discontinued |
|
Nevirapine |
Decreased doravirine concentrations expected No in vitro evidence of antagonistic antiretroviral effects |
Concomitant use not recommended |
|
Oral contraceptives (ethinyl estradiol and levonorgestrel) |
No clinically important pharmacokinetic interactions |
|
|
Pantoprazole |
No clinically important pharmacokinetic interactions when doravirine used concomitantly |
|
|
Raltegravir |
No in vitro evidence of antagonistic antiretroviral effects |
|
|
Rilpivirine |
No in vitro evidence of antagonistic antiretroviral effects |
|
|
Ritonavir |
Increased doravirine exposures and peak plasma concentrations; not considered clinically important |
|
|
St. John's wort (Hypericum perforatum) |
Decreased doravirine concentrations expected; possible decreased efficacy of doravirine |
Concomitant use contraindicated; do not initiate doravirine until ≥4 weeks after St. John's wort discontinued |
|
Tenofovir |
Tenofovir DF: No clinically important pharmacokinetic interactions with doravirine Tenofovir DF: No in vitro evidence of antagonistic antiretroviral effects with doravirine |
|
|
Zidovudine |
No in vitro evidence of antagonistic antiretroviral effects |
Doravirine Pharmacokinetics
Absorption
Bioavailability
64%.
Food
Relative to fasting state, administration with high-fat meal increases AUC, peak plasma concentrations, and trough plasma concentrations by 16, 3, and 36%, respectively.
Effect of food not considered clinically important.
Plasma Concentrations
Peak plasma concentrations occur 2 hours after oral administration. Steady-state concentrations achieved after 2 days.
Distribution
Extent
Distributed into milk in rats; not known whether distributed into human milk.
Plasma Protein Binding
76%.
Elimination
Metabolism
Metabolized primarily by CYP3A.
Elimination Route
Approximately 6% of oral dose eliminated in urine as unchanged doravirine; unchanged drug also eliminated to a minor extent by biliary and/or fecal routes.
Half-life
15 hours.
Special Populations
Moderate hepatic impairment (Child-Pugh class B): No clinically important effect on doravirine pharmacokinetics.
Severe renal impairment: Doravirine exposures increased by 43%.
Based on population pharmacokinetic analysis, renal function does not have a clinically important effect on doravirine pharmacokinetics.
No clinically relevant differences in pharmacokinetics based on age (adults), race, BMI, or sex.
In pediatric patients weighing ≥35 kg and <45 kg receiving doravirine 100 mg daily, AUC and peak plasma concentrations were 25 and 36% higher, respectively, compared to adults; however, not considered clinically important.
Stability
Storage
Oral
Tablets
20–25°C (excursions permitted to 15–30°C).
Store in original bottle. Protect from moisture; do not remove desiccant and keep bottle tightly closed.
Actions and Spectrum
-
Doravirine is a pyridinone HIV NNRTI antiretroviral. Inhibits replication of HIV-1 by interfering with viral polymerase activities of reverse transcriptase.
-
Inhibits polymerization reaction by noncompetitive, non-active site binding to reverse transcriptase causing conformational changes within active site that result in an inactive conformation.
-
Does not inhibit human cellular α- and β-DNA polymerases or mitochondrial γ-DNA polymerase.
-
Active against wild-type HIV-1, including certain strains resistant to other NNRTIs (i.e., those with K103N and/or Y181C substitutions).
-
HIV-1 strains resistant to doravirine have been produced in vitro and have emerged during doravirine therapy.
-
Cross-resistance occurs among HIV NNRTIs (e.g., efavirenz, etravirine, nevirapine, rilpivirine). Treatment-emergent doravirine resistance-associated substitutions can confer cross-resistance to other NNRTIs; however, treatment-emergent doravirine resistance-associated substitution Y318F does not appear to confer reduced susceptibility to efavirenz, etravirine, or rilpivirine.
Advice to Patients
-
Advise patients to take doravirine once every day at a regularly scheduled time with or without food.
-
Advise patients not to miss or skip doses since this can result in development of resistance. If a patient forgets to take doravirine, tell the patient to take the missed dose right away, unless it is almost time for the next dose. Advise the patient not to take 2 doses at one time and to take the next dose at the regularly scheduled time.
-
Advise patients that doravirine may interact with certain other drugs. For patients receiving rifabutin, importance of taking one 100-mg tablet of doravirine twice daily (approximately 12 hours apart).
-
Inform patients that signs and symptoms of inflammation from other previous infections may occur soon after initiation of antiretroviral therapy in some patients with advanced HIV infection (AIDS). These symptoms may be due to an improvement in immune response, enabling the body to fight infections that may have been present with no obvious symptoms. Advise patients to immediately inform a clinician if any symptoms of infection occur.
-
Advise patients to inform their clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs and herbal supplements (e.g., St. John’s wort), as well as any concomitant illnesses.
-
Advise women to inform their clinicians if they are or plan to become pregnant or plan to breast-feed. Inform patients that there is an antiretroviral pregnancy registry to monitor fetal outcomes in pregnant individuals exposed to doravirine.
-
Inform patients of other important precautionary information.
Additional Information
The American Society of Health-System Pharmacists, Inc. represents that the information provided in the accompanying monograph was formulated with a reasonable standard of care, and in conformity with professional standards in the field. Readers are advised that decisions regarding use of drugs are complex medical decisions requiring the independent, informed decision of an appropriate health care professional, and that the information contained in the monograph is provided for informational purposes only. The manufacturer’s labeling should be consulted for more detailed information. The American Society of Health-System Pharmacists, Inc. does not endorse or recommend the use of any drug. The information contained in the monograph is not a substitute for medical care.
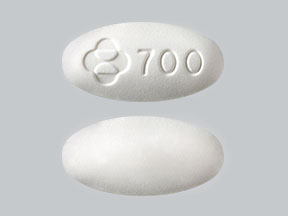
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Tablets, film-coated |
100 mg |
Pifeltro |
Merck |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions February 10, 2025. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
Reload page with references included
Related/similar drugs
Frequently asked questions
- What drugs are contained in the HIV treatment Delstrigo?
- What type of drug is Pifeltro (doravirine)?
More about doravirine
- Check interactions
- Compare alternatives
- Reviews (1)
- Side effects
- Dosage information
- During pregnancy
- Drug class: NNRTIs
- Breastfeeding
- En español