Doravirine, Lamivudine, and Tenofovir Disoproxil (Monograph)
Drug class: HIV Nonnucleoside Reverse Transcriptase Inhibitors
Warning
- Post-Treatment Acute Exacerbation of HBV Infection
-
Severe, acute exacerbations of HBV infection reported following discontinuance of lamivudine or tenofovir DF in patients coinfected with HIV and HBV. Monitor hepatic function closely with both clinical and laboratory follow-up for at least several months after doravirine/lamivudine/tenofovir DF is discontinued in patients coinfected with HIV and HBV. If appropriate, initiation of HBV treatment may be warranted.
Introduction
Antiretroviral; fixed combination of doravirine, lamivudine, and tenofovir disoproxil fumarate (doravirine/lamivudine/tenofovir DF). Doravirine is an HIV nonnucleoside reverse transcriptase inhibitor (NNRTI), lamivudine is an HIV nucleoside reverse transcriptase inhibitor (NRTI), and tenofovir DF is an HIV nucleotide reverse transcriptase inhibitor classified as an NRTI.
Uses for Doravirine, Lamivudine, and Tenofovir Disoproxil
Treatment of HIV Infection
Treatment of HIV-1 infection in adults and pediatric patients weighing ≥35 kg who are antiretroviral-naïve or to replace a current antiretroviral regimen in patients who are virologically suppressed (HIV-1 RNA levels <50 copies/mL) on a stable antiretroviral regimen with no history of treatment failure and no known resistance to any of the individual components of the fixed combination.
Doravirine/lamivudine/tenofovir DF is used as a single-tablet antiretroviral regimen; consult guidelines for the most current information on recommended regimens. Selection of an initial antiretroviral regimen should be individualized based on factors such as virologic efficacy, toxicity, pill burden, dosing frequency, drug-drug interaction potential, resistance test results, comorbid conditions, access, and cost.
Doravirine, Lamivudine, and Tenofovir Disoproxil Dosage and Administration
General
Pretreatment Screening
-
Test patients for hepatitis B virus (HBV) infection prior to or when initiating doravirine/lamivudine/tenofovir DF.
-
Evaluate serum creatinine, estimated creatinine clearance, urine glucose, and urine protein in all patients prior to and when initiating doravirine/lamivudine/tenofovir DF. In patients with chronic kidney disease, additionally assess serum phosphorus.
Patient Monitoring
-
Monitor serum creatinine, estimated creatinine clearance, urine glucose, and urine protein periodically in all patients during treatment with doravirine/lamivudine/tenofovir DF. In patients with chronic kidney disease, additionally monitor serum phosphorus.
-
Consider monitoring bone mineral density (BMD) in adults and pediatric patients who have a history of pathologic bone fracture or other risk factors for osteoporosis or bone loss.
Dispensing and Administration Precautions
-
The ISMP list of error-prone abbreviations, symbols, and dose designations states that the use of abbreviations for antiretroviral medications (e.g., DOR, TAF, TDF) during the medication use process should be avoided as their use has been associated with serious medication errors.
Other General Considerations
-
Avoid doravirine/lamivudine/tenofovir DF in patients who are receiving or have recently received a nephrotoxic agent (e.g., high-dose or multiple nonsteroidal anti-inflammatory agents [NSAIAs]). Consider alternatives to NSAIAs if such therapy is needed in patients at risk for renal dysfunction.
Administration
Oral Administration
Administer orally once daily without regard to food.
Doravirine/lamivudine/tenofovir DF is used alone as a complete antiretroviral regimen.
If a dose is missed, take the missed dose as soon as possible, unless it is almost time for the next dose; do not take 2 doses at one time.
Dosage
Each fixed-combination tablet of doravirine/lamivudine/tenofovir DF contains doravirine 100 mg, lamivudine 300 mg, and tenofovir DF 300 mg.
Pediatric Patients
Treatment of HIV Infection
Oral
Antiretroviral-naïve or -virologically suppressed weighing ≥35 kg: 1 tablet of doravirine/lamivudine/tenofovir DF (doravirine 100 mg, lamivudine 300 mg, tenofovir DF 300 mg) once daily.
Adults
Treatment of HIV Infection
Oral
Antiretroviral-naïve or -virologically suppressed: 1 tablet of doravirine/lamivudine/tenofovir DF (doravirine 100 mg, lamivudine 300 mg, tenofovir DF 300 mg) once daily.
Dosage Modification for Concomitant Use with Rifabutin
In patients receiving concomitant therapy with rifabutin, recommended dosage of doravirine/lamivudine/tenofovir DF is 1 tablet (doravirine 100 mg, lamivudine 300 mg, tenofovir DF 300 mg) once daily and one 100-mg tablet of single-entity doravirine once daily given approximately 12 hours after the fixed-combination tablet.
Special Populations
Hepatic Impairment
Mild or moderate hepatic impairment (Child-Pugh class A or B): Dosage adjustments not needed.
Severe hepatic impairment (Child-Pugh class C): Not studied.
Renal Impairment
Estimated Clcr <50 mL/minute: Not recommended.
Geriatric Patients
No specific dosage recommendations; use with caution because of possible age-related decreases in hepatic, renal, and/or cardiac function and potential for concomitant disease and drug therapy.
Cautions for Doravirine, Lamivudine, and Tenofovir Disoproxil
Contraindications
-
Concomitant use with potent CYP3A inducers (e.g., carbamazepine, oxcarbazepine, phenobarbital, phenytoin, enzalutamide, rifampin, rifapentine, mitotane, St. John’s wort [Hypericum perforatum]).
-
History of hypersensitivity reaction to lamivudine.
Warnings/Precautions
Warnings
Post-treatment Acute Exacerbation of Hepatitis B
In HIV-infected patients with HBV coinfection, severe acute exacerbations of HBV, including liver decompensation and liver failure, reported following discontinuance of lamivudine or tenofovir DF (components of doravirine/lamivudine/tenofovir DF). (See Boxed Warning.) Such reactions could occur following discontinuance of doravirine/lamivudine/tenofovir DF.
Test all HIV-infected patients for presence of HBV before initiating antiretroviral therapy. Closely monitor hepatic function (using both clinical and laboratory follow-up) for at least several months after doravirine/lamivudine/tenofovir DF is discontinued in patients coinfected with HIV and HBV. If appropriate, initiation of HBV treatment may be warranted, especially in patients with advanced liver disease or cirrhosis.
Other Warnings and Precautions
Severe Skin Reactions
Severe skin reactions, including Stevens-Johnson syndrome/toxic epidermal necrolysis, reported. Discontinue doravirine and other medications associated with severe skin reactions if a painful rash with mucosal involvement or a progressive severe rash develops. Monitor patients closely and initiate appropriate therapy.
New Onset or Worsening Renal Impairment
Renal impairment, including acute renal failure and Fanconi syndrome (renal tubular injury with hypophosphatemia), reported with tenofovir DF (a component of doravirine/lamivudine/tenofovir DF).
Determine Scr, estimated Clcr, urine glucose, and urine protein prior to initiation of doravirine/lamivudine/tenofovir DF and routinely monitor as clinically appropriate during treatment. Also determine serum phosphorus in those with chronic kidney disease.
Discontinue doravirine/lamivudine/tenofovir DF if clinically important decreases in renal function or evidence of Fanconi syndrome occurs or if estimated Clcr decreases to <50 mL/minute.
Because persistent or worsening bone pain, pain in extremities, fractures, and/or muscular pain or weakness may be manifestations of proximal renal tubulopathy, promptly evaluate renal function in patients at risk for renal dysfunction who present with such symptoms.
Avoid doravirine/lamivudine/tenofovir DF in patients who are receiving or have recently received a nephrotoxic drug (e.g., high-dose or multiple NSAIAs). Acute renal failure reported after initiation of high-dose or multiple NSAIAs in HIV-infected patients at risk for renal dysfunction who appeared stable while receiving tenofovir DF; hospitalization and renal replacement therapy required in some patients. Consider alternatives to NSAIAs in patients at risk for renal dysfunction.
Bone Loss and Mineralization Defects
Decreases in bone mineral density (BMD) from baseline, increases in several biochemical markers of bone metabolism, and increased serum parathyroid hormone and 1,25 vitamin D levels reported in adults receiving tenofovir DF (a component of doravirine/lamivudine/tenofovir DF). Effects of tenofovir-associated changes in BMD on long-term bone health and future fracture risk unknown. Similar bone effects observed with tenofovir DF in adults and pediatric patients 2 to <18 years of age.
Osteomalacia associated with proximal renal tubulopathy, which may contribute to fractures, reported with tenofovir DF. Arthralgia and muscle pain or weakness also reported in cases of proximal renal tubulopathy. Consider hypophosphatemia and osteomalacia secondary to proximal renal tubulopathy in patients at risk of renal dysfunction who present with persistent or worsening bone or muscle symptoms while receiving preparations containing tenofovir DF.
Consider BMD monitoring in patients with history of pathologic bone fracture or other risk factors for osteoporosis or bone loss. Effect of calcium and vitamin D supplementation not studied, but may be beneficial for all patients. If bone abnormalities suspected, obtain appropriate consultation.
Interactions
Concomitant use with certain drugs may result in known or potentially clinically important drug interactions, some of which may lead to loss of therapeutic effect of the antiretrovirals and possible development of resistance or may increase plasma concentrations of the antiretroviral agents and/or concomitant drugs leading to clinically important adverse reactions.
Consider potential for drug interactions prior to and during doravirine/lamivudine/tenofovir DF therapy; review concomitant drugs during doravirine/lamivudine/tenofovir DF therapy and monitor for adverse effects.
Immune Reconstitution Syndrome
Immune reconstitution syndrome reported in HIV-infected patients receiving multiple-drug antiretroviral therapy. During the initial phase of treatment, HIV-infected patients whose immune system responds to antiretroviral therapy may develop an inflammatory response to indolent or residual opportunistic infections (e.g., Mycobacterium avium, cytomegalovirus [CMV], Pneumocystis jirovecii [formerly P. carinii], tuberculosis); such responses may necessitate further evaluation and treatment.
Autoimmune disorders (e.g., Graves' disease, polymyositis, Guillain-Barré syndrome, autoimmune hepatitis) also reported in the setting of immune reconstitution; however, time to onset is more variable and can occur many months after initiation of antiretroviral therapy.
Use of Fixed Combinations
Consider cautions, precautions, contraindications, and interactions associated with each component of doravirine/lamivudine/tenofovir DF. Consider cautionary information applicable to specific populations for each drug in the fixed combination.
Specific Populations
Pregnancy
Antiretroviral Pregnancy Registry at 800-258-4263 or [Web].
Doravirine/lamivudine/tenofovir DF: Insufficient data in pregnant women to assess the risk of birth defects and miscarriage.
Lactation
Doravirine: Not known whether distributed into human milk. Distributed into milk of lactating rats.
Lamivudine and tenofovir DF: Distributed into human milk.
Doravirine/lamivudine/tenofovir DF: Not known whether the fixed combination or individual drug components affect human milk production or affect the breast-fed infant.
The HHS perinatal HIV transmission guideline provides updated recommendations on infant feeding. The guideline states that patients with HIV should receive evidence-based, patient-centered counseling to support shared decision making about infant feeding. During counseling, patients should be informed that feeding with appropriate formula or pasteurized donor human milk from a milk bank eliminates the risk of postnatal HIV transmission to the infant. Additionally, achieving and maintaining viral suppression with antiretroviral therapy during pregnancy and postpartum reduces the risk of breastfeeding HIV transmission to <1%, but does not completely eliminate the risk. Replacement feeding with formula or banked pasteurized donor milk is recommended when patients with HIV are not on antiretroviral therapy and/or do not have a suppressed viral load during pregnancy (at a minimum throughout the third trimester), as well as at delivery.
Pediatric Use
Safety and efficacy established in pediatric patients who weigh ≥35 kg. Safety and efficacy not established in pediatric patients weighing <35 kg.
Geriatric Use
Experience in patients ≥65 years of age insufficient to determine whether they respond differently than younger adults.
Use with caution in geriatric patients because of age-related decreases in hepatic, renal, and/or cardiac function and potential for concomitant disease and drug therapy.
Hepatic Impairment
Doravirine: No clinically important differences in doravirine pharmacokinetics in patients with moderate hepatic impairment (Child-Pugh class B). Not studied in those with severe hepatic impairment (Child-Pugh class C).
Lamivudine: Pharmacokinetics not substantially affected by diminishing hepatic function. Safety and efficacy not established in patients with decompensated liver disease.
Tenofovir: Pharmacokinetics not substantially affected by any degree of hepatic impairment.
No dosage adjustment of doravirine/lamivudine/tenofovir DF required in patients with mild or moderate (Child-Pugh class A or B) hepatic impairment; no studies conducted in patients with severe (Child-Pugh class C) hepatic impairment.
Renal Impairment
Not recommended in patients with estimated Clcr <50 mL/minute because dosage of lamivudine and tenofovir DF (components of doravirine/lamivudine/tenofovir DF) cannot be adjusted for renal impairment.
Common Adverse Effects
Adverse effects reported in ≥5% of patients receiving doravirine/lamivudine/tenofovir DF include dizziness, nausea, and abnormal dreams.
Drug Interactions
The following drug interactions are based on studies using the individual components of doravirine/lamivudine/tenofovir DF. Consider interactions associated with each drug in the fixed combination.
Drugs Affecting or Metabolized by Hepatic Microsomal Enzymes
Doravirine: Primarily metabolized by CYP3A. Concomitant use of doravirine and CYP3A inducers may decrease doravirine plasma concentrations and may reduce efficacy of doravirine. Concomitant use of doravirine/lamivudine/tenofovir DF with CYP3A inhibitors may increase doravirine plasma concentrations. In vitro, does not inhibit CYP1A2, 2B6, 2C8, 2C9, 2C19, 2D6, or 3A4; not likely to induce CYP1A2, 2B6, or 3A4. Not likely to have a clinically important effect on the exposure of drugs metabolized by CYP isoenzymes.
Lamivudine: Not substantially metabolized by CYP isoenzymes; does not inhibit or induce CYP isoenzymes. Clinically important CYP-mediated drug interactions unlikely.
Tenofovir DF: Pharmacokinetic interactions with inhibitors or substrates of CYP isoenzymes unlikely.
Drugs Affecting or Metabolized by UGT
Doravirine: In vitro, does not inhibit UGT1A1.
Drugs Affecting or Affected by Other Transporters
Doravirine: Based on in vitro studies, not likely to inhibit P-glycoprotein (P-gp) transport system, organic anion transport polypeptide (OATP) 1B1, OATP1B3, bile salt export pump (BSEP), organic anion transporter (OAT) 1, OAT3, organic cation transporter (OCT) 2, multidrug and toxin extrusion transporter (MATE) 1, or MATE2K.
Drugs Affecting Renal Function
Drugs that reduce renal function or compete for active tubular secretion (e.g., acyclovir, aminoglycosides, cidofovir, ganciclovir, valacyclovir, valganciclovir, high-dose or multiple NSAIAs): Potential increased concentrations of lamivudine, tenofovir, and/or concomitant drug.
Specific Drugs
|
Drug |
Interaction |
Comments |
|---|---|---|
|
Antacids |
Antacid containing aluminum hydroxide, magnesium hydroxide, and simethicone: No clinically important effect on doravirine concentrations |
|
|
Anticonvulsants |
Carbamazepine, oxcarbazepine, phenobarbital, phenytoin: Decreased doravirine concentrations expected; possible decreased doravirine efficacy |
Carbamazepine, oxcarbazepine, phenobarbital, phenytoin: Concomitant use contraindicated; do not initiate doravirine/lamivudine/tenofovir DF until ≥4 weeks after anticonvulsant discontinued; |
|
Antimycobacterials (rifamycins) |
Rifabutin: Decreased doravirine AUC and trough plasma concentrations; peak plasma concentrations not affected Rifampin: Decreased doravirine AUC, peak plasma concentrations, and trough plasma concentrations; possible decreased doravirine efficacy Rifapentine: Decreased doravirine concentrations expected; possible decreased efficacy of doravirine |
Rifabutin: Increase doravirine dosage by using doravirine/lamivudine/tenofovir DF in conjunction with single-entity doravirine Rifampin, rifapentine: Concomitant use contraindicated; do not initiate doravirine/lamivudine/tenofovir DF until ≥4 weeks after rifampin or rifapentine discontinued |
|
Antiretroviral agents |
Doravirine/lamivudine/tenofovir DF is a complete regimen; concomitant use with other antiretroviral agents not recommended |
|
|
Atorvastatin |
No clinically important pharmacokinetic interactions with doravirine |
|
|
Co-trimoxazole |
Increased lamivudine AUC and decreased lamivudine oral clearance; no effect on pharmacokinetics of trimethoprim or sulfamethoxazole |
|
|
Elbasvir and grazoprevir |
No clinically important pharmacokinetic interactions with doravirine |
|
|
Entecavir |
No clinically important pharmacokinetic interactions with tenofovir DF |
|
|
Enzalutamide |
Decreased doravirine concentrations expected; possible decreased doravirine efficacy |
Concomitant use contraindicated; do not initiate doravirine/lamivudine/tenofovir DF until ≥4 weeks after enzalutamide discontinued |
|
Estrogens and progestins |
Contraceptives containing ethinyl estradiol and levonorgestrel (oral): No effect on ethinyl estradiol or levonorgestrel concentrations expected if used with doravirine Contraceptives containing ethinyl estradiol and norgestimate (oral): No clinically important pharmacokinetic interaction with tenofovir DF |
|
|
Ketoconazole |
Increased doravirine exposures and peak plasma concentrations; not considered clinically important |
|
|
Ledipasvir and sofosbuvir |
Fixed combination of ledipasvir and sofosbuvir (ledipasvir/sofosbuvir): No clinically important pharmacokinetic interactions with doravirine; increased tenofovir DF exposures |
Monitor for tenofovir-associated adverse effects |
|
Metformin |
No clinically important pharmacokinetic interactions with doravirine |
|
|
Methadone |
No clinically important effects of doravirine or tenofovir DF on pharmacokinetics of methadone or either antiretroviral |
|
|
Midazolam |
No clinically important pharmacokinetic interactions with doravirine |
|
|
Mitotane |
Decreased doravirine concentrations expected; possible decreased doravirine efficacy |
Concomitant use contraindicated; do not initiate doravirine/lamivudine/tenofovir DF until ≥4 weeks after mitotane discontinued |
|
Proton-pump inhibitors |
Pantoprazole: No clinically important effect on doravirine concentrations |
|
|
St. John's wort (Hypericum perforatum) |
Decreased doravirine concentrations expected; possible decreased doravirine efficacy |
Concomitant use contraindicated; do not initiate doravirine/lamivudine/tenofovir DF until ≥4 weeks after St. John's wort discontinued |
|
Sofosbuvir |
No clinically important pharmacokinetic interactions with tenofovir DF |
|
|
Sofosbuvir and velpatasvir |
Fixed combination of sofosbuvir and velpatasvir (sofosbuvir/velpatasvir): Possible increased tenofovir concentrations and AUC |
Sofosbuvir/velpatasvir: Monitor for tenofovir-associated adverse effects |
|
Sorbitol |
Decreased lamivudine AUC and peak plasma concentrations |
Avoid concomitant use of doravirine/lamivudine/tenofovir DF and sorbitol-containing drugs |
|
Tacrolimus |
No clinically important pharmacokinetic interactions with tenofovir DF |
Doravirine, Lamivudine, and Tenofovir Disoproxil Pharmacokinetics
Absorption
Bioavailability
Doravirine: 64%.
Lamivudine: 86%.
Tenofovir DF: 25%.
Food
Relative to fasting state, administration of doravirine, lamivudine, and tenofovir DF with high-fat meal increases AUC of doravirine and tenofovir by 10 and 27%, respectively, and decreases lamivudine AUC by 7%.
Effect of food not considered clinically important.
Plasma Concentrations
Fixed-combination tablet containing doravirine 100 mg, lamivudine 300 mg, and tenofovir DF 300 mg is bioequivalent to a 100-mg tablet of doravirine, 300-mg tablet of lamivudine, and 300-mg tablet of tenofovir DF given simultaneously.
Peak plasma concentrations of doravirine and tenofovir occur 2 hours and 1 hour, respectively, after oral administration.
Distribution
Extent
Doravirine: Distributed into milk in rats; not known whether distributed into human milk.
Lamivudine and tenofovir DF: Distributed into human milk.
Plasma Protein Binding
Doravirine: 76%.
Lamivudine: <35%.
Tenofovir: <0.7%.
Elimination
Metabolism
Doravirine: Primarily metabolized by CYP3A.
Lamivudine: Metabolized by CYP isoenzymes only to a minor extent.
Tenofovir DF: Does not undergo hepatic metabolism.
Elimination Route
Doravirine: Approximately 6% of oral dose eliminated in urine as unchanged doravirine; unchanged drug also eliminated to a minor extent by biliary and/or fecal routes.
Lamivudine: Eliminated by glomerular filtration and active tubular secretion.
Tenofovir: Eliminated by glomerular filtration and active tubular secretion.
Half-life
Doravirine: 15 hours.
Lamivudine: 5–7 hours.
Tenofovir: 17 hours.
Special Populations
Hepatic impairment: Doravirine pharmacokinetics not substantially affected by moderate hepatic impairment (Child-Pugh class B). Lamivudine pharmacokinetics not substantially affected by diminishing hepatic function. Tenofovir pharmacokinetics not substantially affected by any degree of hepatic impairment.
Renal impairment: Doravirine exposure not significantly impacted in mild to severe renal impairment (Clcr >15 mL/minute); insufficient data in patients with end-stage renal disease and not studied in patients receiving dialysis. Lamivudine exposures, peak plasma concentrations, and half-life increased and clearance decreased to a clinically important extent with diminishing renal function (Clcr 111 to < 10 mL/minute). Tenofovir exposures and peak plasma concentrations substantially increased in those with Clcr <50 mL/minute or with end-stage renal disease requiring dialysis.
No clinically important differences in pharmacokinetics based on age in adults (doravirine), race (doravirine, lamivudine), BMI (doravirine), or sex (doravirine, lamivudine, tenofovir DF).
Doravirine, lamivudine, and tenofovir DF exposures in pediatric patients 12 to <18 years of age weighing ≥35 kg similar to those in adults.
Stability
Storage
Oral
Tablets
20–25°C (excursions permitted between 15–30°C).
Store in original bottle. Protect from moisture; do not remove desiccant and keep bottle tightly closed.
Actions and Spectrum
-
Doravirine/lamivudine/tenofovir DF is a fixed-combination antiretroviral containing doravirine, lamivudine, and tenofovir DF.
-
Doravirine is a pyridinone HIV NNRTI antiretroviral. Inhibits replication of HIV-1 by interfering with viral polymerase activities of reverse transcriptase. Active against HIV-1, including certain strains resistant to some other NNRTIs.
-
Lamivudine is an HIV NRTI. Converted intracellularly to an active 5′-triphosphate metabolite (lamivudine triphosphate). After conversion, acts as a reverse transcriptase inhibitor via DNA chain termination after incorporation of the nucleotide analogue. Active against HIV-1.
-
Tenofovir DF is a nucleotide reverse transcriptase inhibitor antiretroviral classified as an HIV NRTI. Prodrug that is inactive until it undergoes diester hydrolysis in vivo to tenofovir and is subsequently metabolized to the active metabolite (tenofovir diphosphate).
-
HIV-1 strains resistant to doravirine, lamivudine, or tenofovir produced in vitro and have emerged during doravirine/lamivudine/tenofovir DF therapy. One or more primary mutations associated with resistance to doravirine identified in HIV-1 isolates from patients who received doravirine/lamivudine/tenofovir DF and were included in the resistance analysis subset (i.e., those with plasma HIV-1 RNA levels exceeding 400 copies/mL at virologic failure or early study discontinuation with resistance data); genotypic resistance against lamivudine and tenofovir DF also identified.
-
Cross-resistance occurs among HIV NNRTIs (e.g., efavirenz, etravirine, nevirapine, rilpivirine). Treatment-emergent doravirine resistance-associated substitutions can confer cross-resistance to other NNRTIs; however, treatment-emergent doravirine resistance-associated substitution Y318F does not appear to confer reduced susceptibility to efavirenz, etravirine, or rilpivirine. Cross-resistance also occurs among HIV NRTIs.
Advice to Patients
-
Stress the importance of taking as prescribed; do not alter or discontinue antiretroviral regimen without consulting clinician.
-
Advise the patient to read the patient information provided by the manufacturer.
-
Advise patients to take doravirine/lamivudine/tenofovir DF once every day at a regularly scheduled time with or without food.
-
Advise patients not to miss or skip doses since this can result in development of resistance. If a patient forgets to take doravirine/lamivudine/tenofovir DF, tell the patient to take the missed dose right away, unless it is almost time for the next dose. Advise the patient not to take 2 doses at one time and to take the next dose at the regularly scheduled time.
-
Inform patients that testing for HBV infection is recommended before antiretroviral therapy is initiated. Also advise patients that severe acute exacerbations of HBV infection have been reported following discontinuance of lamivudine or tenofovir DF (components of doravirine/lamivudine/tenofovir DF) in HIV-infected patients coinfected with HBV. Stress importance of not discontinuing doravirine/lamivudine/tenofovir DF without consulting a clinician.
-
Inform patients that renal impairment, including cases of acute renal failure or Fanconi syndrome, has occurred in association with use of tenofovir DF (a component of doravirine/lamivudine/tenofovir DF). Stress importance of not using doravirine/lamivudine/tenofovir DF concomitantly with or shortly after nephrotoxic agents (e.g., high-dose or multiple NSAIAs).
-
Inform patients that decreased BMD has occurred with the use of tenofovir DF (a component of doravirine/lamivudine/tenofovir DF) and that assessment of BMD should be considered in those with a history of pathologic bone fracture or other risk factors for osteoporosis or bone loss.
-
Advise patients that doravirine/lamivudine/tenofovir DF may interact with certain other drugs. For patients receiving rifabutin, stress importance of taking one 100-mg tablet of single-entity doravirine each day approximately 12 hours after taking doravirine/lamivudine/tenofovir DF.
-
Stress importance of informing clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs and herbal supplements (e.g., St. John’s wort), as well as any concomitant illnesses
-
Inform patients that signs and symptoms of inflammation from other previous infections may occur soon after initiation of antiretroviral therapy in some patients with advanced HIV infection. These symptoms may be due to an improvement in immune response, enabling the body to fight infections that may have been present with no obvious symptoms. Stress importance of immediately informing a clinician if any symptoms of infection occur.
-
Stress importance of patients informing clinicians if they are or plan to become pregnant or plan to breast-feed.
-
Inform patients of other important precautionary information.
Additional Information
The American Society of Health-System Pharmacists, Inc. represents that the information provided in the accompanying monograph was formulated with a reasonable standard of care, and in conformity with professional standards in the field. Readers are advised that decisions regarding use of drugs are complex medical decisions requiring the independent, informed decision of an appropriate health care professional, and that the information contained in the monograph is provided for informational purposes only. The manufacturer’s labeling should be consulted for more detailed information. The American Society of Health-System Pharmacists, Inc. does not endorse or recommend the use of any drug. The information contained in the monograph is not a substitute for medical care.
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
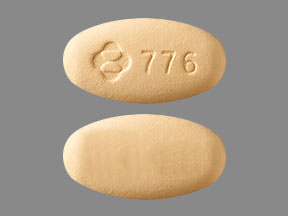
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Tablets, film-coated |
Doravirine 100 mg, Lamivudine 300 mg, and Tenofovir Disoproxil Fumarate 300 mg |
Delstrigo |
Merck |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions May 10, 2025. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
Reload page with references included
Related/similar drugs
Frequently asked questions
More about doravirine / lamivudine / tenofovir disoproxil
- Check interactions
- Compare alternatives
- Reviews (8)
- Side effects
- Dosage information
- During pregnancy
- Drug class: antiviral combinations
- En español
Patient resources
- Doravirine, lamivudine, and tenofovir drug information
- Doravirine, lamivudine, and tenofovir (Advanced Reading)
- Doravirine, Lamivudine, and Tenofovir Disoproxil Fumarate