Mitral Valve Repair
Medically reviewed by Drugs.com. Last updated on May 4, 2025.
What do I need to know about mitral valve repair (MVR)?
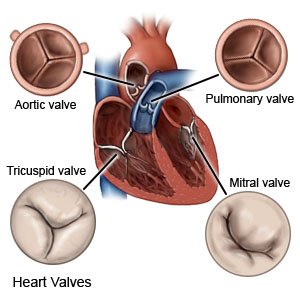
MVR is surgery to fix a damaged or diseased mitral valve. The mitral valve normally opens and closes to let blood pass through the heart. If your mitral valve is damaged, blood may not flow as it should through your heart.
 |
How do I prepare for MVR?
- Your surgeon will tell you how to prepare. Your surgeon may tell you not to eat or drink anything after midnight on the day of your surgery. Arrange to have someone drive you home when you are discharged.
- Tell your surgeon about all medicines you currently take. Your surgeon will tell you if you need to stop any medicine for the surgery, and when to stop. Your surgeon will tell you which medicines to take or not take on the day of surgery.
- Tell your surgeon about any allergies you have, including to anesthesia or medicines.
- You may need an echocardiogram (echo) before surgery. An echo is a type of ultrasound that uses sound waves to show the structure and function of your heart. This will help your surgeon plan your surgery.
- Your surgeon will tell you if you need any other tests before your surgery, and when to have them.
Drugs used to treat this and similar conditions
Paracetamol
Paracetamol (Panadol, Calpol, Alvedon) is a widely used over-the-counter painkiller and fever ...
Arcalyst
Arcalyst (rilonacept) is used to treat Cryopyrin-Associated Periodic Syndromes, Deficiency of ...
Ozempic
Learn about Ozempic (semaglutide) for type 2 diabetes treatment, weight management, cardiovascular ...
Tylenol
Tylenol is a pain reliever and a fever reducer used to treat many conditions such as headaches ...
Ancef
Ancef is used for bacterial endocarditis prevention, bacterial infection, bone infection ...
Rifadin
Rifadin is used for bartonellosis, endocarditis, haemophilus influenzae prophylaxis, legionella ...
Ceftazidime
Ceftazidime systemic is used for bacteremia, bladder infection, bone infection, endocarditis ...
Aspirin
Aspirin is used to treat mild to moderate pain and to reduce fever or inflammation. Learn about ...
Rilonacept
Rilonacept systemic is used for cryopyrin-associated periodic syndromes, familial cold ...
Metronidazole
Metronidazole is an antibiotic used to fight bacteria in your body. Learn about side effects ...
What will happen during MVR?
- You will be given general anesthesia to keep you asleep and free from pain during surgery. Your surgeon will make 1 or more incisions on your chest. The size and location of the incisions will depend on the type of repair and your risk for complications. Your heart will be connected to a bypass machine. This machine keeps blood out of your heart during surgery and pumps blood through your body.
- Your surgeon will use a device to tighten or strengthen the annulus (ring of tissue) around the valve. The device will be sewn into place. Your surgeon will then repair any other part of the valve that is damaged. Your surgeon may use echo during surgery to check the valve.
- Your surgeon will disconnect the bypass machine when the valve starts to work as it should. Your incisions will be closed with stitches or staples and covered with bandages.
What should I expect after MVR?
- You will be taken to a recovery room until you are fully awake. Healthcare providers will monitor you closely for any problems. You will need to stay in the hospital for up to a week, depending on your condition.
- Talk to healthcare providers before you get up the first time. They may need to help you stand up safely. When you are able to get up on your own, sit or lie down right away if you feel weak or dizzy. Then press the call light button to let healthcare providers know you need help. You may need to hold a pillow against your incision when you move in and out of bed. This will help decrease pain.
What are the risks of MVR?
You may bleed more than expected or develop an infection. Your repaired valve may stop working. The leaflets (flaps) of the valve may not move as they should. You may need more surgery to fix or replace the valve or leaflets. Your symptoms may return, even after surgery. You may have an increased risk of heart attack or stroke. You may develop a blood clot or irregular heartbeat. These can be life-threatening.
Care Agreement
You have the right to help plan your care. Learn about your health condition and how it may be treated. Discuss treatment options with your healthcare providers to decide what care you want to receive. You always have the right to refuse treatment. The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
