Heart valve problems
Medically reviewed by Drugs.com. Last updated on Mar 4, 2025.
What are Heart valve problems?

The heart has four valves – the aortic, mitral, tricuspid and pulmonary valves. Like valves used in house plumbing, the heart valves open to allow fluid (blood) to be pumped forward, and they close to prevent fluid from flowing backward. Human heart valves are flaps of tissue called leaflets or cusps.
Heart valve problems fall into two major categories:
- Stenosis – The opening of the valve is too narrow, and this interferes with the forward flow of blood.
- Regurgitation – The valve doesn't close properly. It leaks, sometimes causing a significant backflow of blood.
Heart valve problems can be congenital, which means present at birth, or acquired after birth. A heart valve problem is classified as congenital when some factor during fetal development causes the valve to form abnormally. Congenital heart valve disease affects about 1 in 1,000 newborns. Most of these infants have stenosis of either the pulmonary or the aortic valve.
A heart valve problem is acquired if it occurs in a valve that was structurally normal at birth. Some causes of acquired heart valve problems include:
- Rheumatic fever, an inflammatory illness that may follow an untreated strep throat infection
- Endocarditis, inflammation and infection of the heart valves
- Idiopathic calcific aortic stenosis, a degenerative condition seen primarily in the elderly, in which the aortic valve cusps become thickened, fused and infiltrated with calcium
- Syphilis
- Connective tissue disorders, such as Marfan's syndrome.
Heart valve problems affect each valve in a slightly different way.
Aortic valve
The aortic valve opens to allow blood to pass from the left ventricle to the aorta, the massive blood vessel that directs oxygenated blood from the heart to the rest of the body. Disorders of this valve include:
- Congenital aortic stenosis – When a child is born with congenital aortic stenosis, the problem is usually a bicuspid aortic valve, meaning the valve has two flaps instead of the usual three. In about 10% of affected newborns, the aortic valve is so narrow that the child develops severe cardiac symptoms within in the first year of life. In the remaining 90%, congenital aortic stenosis is discovered when a heart murmur is found during a physical examination or a person develops symptoms later in life.
- Acquired aortic stenosis – In adulthood, aortic stenosis typically is caused by rheumatic fever or idiopathic calcific aortic stenosis. Some recent research suggests that the same processes that cause atherosclerosis in the arteries of the heart may contribute to the development of aortic stenosis.
- Aortic regurgitation – In aortic regurgitation, the aortic valve does not close properly, allowing blood to flow backward into the left ventricle. This decreases the forward flow of oxygenated blood through the aorta, while the backflow into the ventricle eventually dilates (stretches) the ventricle out of shape. In the past, adults with aortic regurgitation often had rheumatic fever in childhood. Today, other causes are more common, such as congenital heart disease, infection called endocarditis and connective tissue disorders.
Aortic valve problems in adults are more common in men than women.
Mitral valve
The mitral valve opens to allow blood to pass from the left atrium to the left ventricle. Disorders of this valve include:
- Mitral stenosis – Congenital mitral stenosis is rare. The typical adult patient is a woman whose mitral valve was damaged by rheumatic fever.
- Mitral valve prolapse – In this condition, the leaflets of the mitral valve fail to close properly. It is a common condition, particularly among women between the ages of 14 and 30. The underlying cause is unknown, and the majority of patients never have symptoms. In most women with this condition, mitral valve prolapse has no significance. However, in men, the prolapse is more often related to abnormalities of the valve leaflets that tend to get worse over time. This can lead to severe mitral regurgitation.
- Mitral regurgitation – In the past, rheumatic fever was the most often cause of mitral regurgitation. Today, mitral valve prolapse in men, endocarditis, ischemic heart disease and dilated cardiomyopathy are the most common causes.
Pulmonary valve
The pulmonary valve, or pulmonic valve, is located between the right ventricle and the pulmonary artery. It allows oxygen-poor blood to flow from the right side of the heart to the lungs for oxygenation. Disorders of this valve include:
- Congenital pulmonic stenosis – In the relatively few newborns with severe congenital pulmonic stenosis, the child develops heart failure or cyanosis (a bluish color to the lips, fingernails and skin) within the first month of life. In most cases, the valve is deformed, with two or three leaflets partially fused.
- Adult disorders of the pulmonic valve – In adults, the pulmonic valve most often is damaged because of pulmonary hypertension (abnormally high pressure within the blood vessels in the lungs). Pulmonary hypertension can be related to chronic obstructive pulmonary disease or severe sleep apnea. It can also develop without any known underlying cause (called primary pulmonary hypertension). Damage from rheumatic fever or endocarditis is relatively rare.
Tricuspid valve
The tricuspid valve allows blood to flow from the right atrium to the right ventricle. Disorders of this valve include:
- Tricuspid stenosis – This usually is caused by an episode of rheumatic fever, which often damages the mitral valve at the same time. Tricuspid stenosis is rare in North America and Europe.
- Tricuspid regurgitation – Tricuspid regurgitation typically occurs because of pulmonary hypertension, but it also can be caused by heart failure, myocardial infarction, endocarditis or trauma.
Symptoms
Many people with mild heart valve problems do not have any symptoms, and the abnormal valve is discovered only when a heart murmur is heard during a physical examination. For more severe heart valve problems, symptoms vary slightly depending on which valve is involved.
- Congenital heart valve problems – Severe valve narrowing can cause a condition called cyanosis, in which the skin becomes bluish, and symptoms of heart failure.
- Aortic stenosis – Aortic stenosis usually does not cause symptoms until the valve opening narrows to about one-third of normal. Symptoms include shortness of breath during exertion (exertional dyspnea), heart-related chest pain (angina pectoris) and fainting spells (syncope).
- Aortic regurgitation – A patient can have significant aortic regurgitation for 10 to 15 years without developing significant symptoms. When symptoms begin, there may be palpitations; cardiac arrhythmias; shortness of breath during exertion; breathlessness while lying down (orthopnea); sudden, severe shortness of breath during the middle of the night (paroxysmal nocturnal dyspnea); sweating; angina; and symptoms of heart failure.
- Mitral stenosis – Symptoms include shortness of breath on exertion; sudden, severe shortness of breath during the middle of the night; cardiac arrhythmias, especially atrial fibrillation; and coughing up blood (hemoptysis). In some patients, blood clots (thrombi) form in the left atrium. These clots can travel through blood vessels and damage the brain, spleen or kidneys.
- Mitral regurgitation – Symptoms include fatigue, shortness of breath during exertion and breathlessness while lying down.
- Pulmonic valve problems – Symptoms include fatigue, fainting spells and symptoms of heart failure.
- Tricuspid regurgitation – This does not usually cause symptoms unless it is severe and associated with pulmonary hypertension. Leg swelling and more generalized fluid retention can occur.
Diagnosis
If you are having symptoms, your doctor will begin by evaluating your risk of heart valve problems. Your doctor will ask questions about your family history of heart problems; your personal history of rheumatic fever, syphilis, hypertension, arteriosclerosis or connective tissue disorders; and your risk of endocarditis caused by intravenous (IV) drug use or a recent medical or dental procedure. If the patient is an infant, the doctor will ask about the mother's health or environmental risk factors during pregnancy.
Your doctor may suspect that you have a heart valve problem based on your specific symptoms and medical history. To support the diagnosis, your doctor will examine you, paying special attention to your heart. Your doctor will evaluate the size of your heart (to check for enlargement) and use a stethoscope to listen for heart murmurs. Because specific heart valve problems produce specific types of heart murmurs, your doctor often can make a tentative diagnosis based on your murmur's distinctive sound and whether the murmur occurs when the heart is contracting (a systolic murmur) or relaxing (a diastolic murmur).
To confirm the diagnosis of a heart valve problem and to evaluate its effects on your heart, your doctor will order diagnostic tests. Initial testing usually includes an electrocardiogram (EKG) and an echocardiogram. Additional testing may include a chest X-ray, blood tests to check for infection in patients with suspected endocarditis, and sometimes cardiac catheterization.
Expected duration
In general, heart valve problems often persist throughout life and may gradually worsen with time. Those caused by endocarditis sometimes may produce severe symptoms and rapid deterioration within a few days.
Prevention
There is no way to prevent the majority of congenital heart valve problems. Pregnant women should have regularly scheduled prenatal care and should avoid using alcohol.
You can prevent certain acquired heart valve abnormalities by preventing rheumatic fever. To do this, take antibiotics exactly as prescribed whenever you have strep throat.
Treatment
If you have a mild heart valve problem without any symptoms, your doctor may simply monitor your condition.
If you have moderate or severe symptoms, your treatment will be determined by the severity of your symptoms and the results of diagnostic tests. Although your doctor can give you medications to temporarily treat symptoms such as angina, cardiac arrhythmias and heart failure, you eventually may need to have the abnormal valve repaired or replaced. This can be done in several different ways:
- Percutaneous balloon valvuloplasty (for stenosis) – In this procedure, a tiny catheter with a balloon at its tip is passed through the narrowed heart valve. The tiny balloon then is inflated and pulled back through the narrowed valve to widen it.
- Valvotomy using traditional surgery (for stenosis) – In this procedure, the surgeon opens the heart and separates valve leaflets that are fused together.
- Valve repair (for regurgitation) – In this procedure, the surgeon opens the heart and repairs the valve leaflets so that they close more effectively.
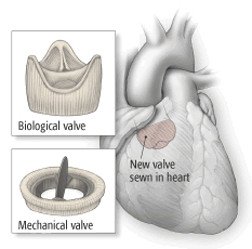
- Valve replacement using traditional surgery – Defective heart valves can be replaced with a mechanical heart valve made of plastic or Dacron, or a biological valve made of tissue taken from a pig, cow or deceased human donor. After surgery, patients with mechanical valves must take anticoagulant medications to prevent blood clots.
|
|
- Transcutaneous aortic valve replacement (TAVR) -- A more recent option for replacement of an aortic valve does not involve surgery. Instead, the replacement valve is crimped onto a deflated balloon. This assembly sits at the tip of a wire called a catheter. The catheter is inserted into a blood vessel in the groin or arm and carefully maneuvered into the heart. Once the assembly is inside the aortic valve, the balloon is inflated. This expands the new valve and wedges it into place. The catheter is then removed, leaving the new valve in place.
When to call a professional
Call your doctor immediately if you begin to experience any symptoms that may be related to a heart problem, especially shortness of breath, chest pain, rapid or irregular heartbeat, or fainting spells.
If you have been diagnosed with a heart valve problem, ask your doctor whether you are at risk of endocarditis. If so, you will need to take antibiotics before undergoing any medical or dental procedure in which bacteria may enter your blood and infect your abnormal valve.
Prognosis
Among patients who undergo surgical treatments for heart valve problems, the major risks occur during and immediately after surgery. After that, the outlook is usually excellent. People that have had surgery are at higher risk of developing an infection on the heart valve (endocarditis) throughout life.
Additional info
American Heart Association (AHA)
https://www.heart.org/
National Heart, Lung, and Blood Institute (NHLBI)
https://www.nhlbi.nih.gov/
American College of Cardiology
https://www.acc.org/
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.