Mitral Regurgitation
Medically reviewed by Drugs.com. Last updated on Aug 4, 2025.
What is mitral regurgitation (MR)?
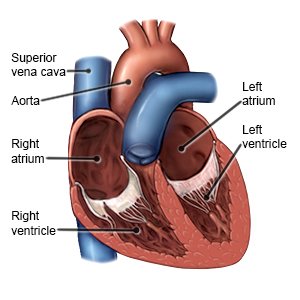
MR is also called mitral insufficiency. When your heart contracts, blood leaks backward into your left atrium. Normally, blood flows through the mitral valve from the left atrium to the left ventricle. Then the mitral valve closes. When your heart contracts, blood flows from the left ventricle out to your body.
 |
What increases my risk for MR?
MR is caused by damage or weakness of the mitral valve. Any of the following may increase your risk for these problems:
- Older age
- Being born with heart problems
- Rheumatic fever or infection of the mitral valve
- Heart attack, high blood pressure, or mitral valve prolapse
- Injury to the mitral valve from trauma, a heart procedure, or radiation
- A connective tissue disease such as lupus or Marfan syndrome
- Certain medicines, such as weight loss pills or medicines that treat migraines
What are the signs and symptoms of MR?
You may not have symptoms, or you may have symptoms that develop gradually:
- Shortness of breath that gets worse during activity or when you lie on your back
- Chest pain or discomfort
- A fast heartbeat or feeling your heartbeat flutter
- Weakness, dizziness, or fatigue
- Cough, especially when you lie down
- Swollen feet or ankles
How is MR diagnosed?
Your healthcare provider will examine you and listen to your heart. He or she will ask if you have ever had strep throat or rheumatic fever. Tell him or her if you have a family history of heart disease. You may also need any of the following:
- An echocardiogram is a type of ultrasound. It is used to show problems with your mitral valve and how blood flows through your heart. It may also show how well your heart is pumping. You may need a transthoracic or transesophageal echocardiogram. Ask your healthcare provider about these types of echocardiogram.
- X-ray, CT, or MRI pictures may show problems with your valve or an enlarged heart. These tests may also show fluid in your lungs. You may be given contrast liquid to help your heart and lungs show up better in the pictures. Tell the healthcare provider if you have ever had an allergic reaction to contrast liquid. Do not enter the MRI room with anything metal. Metal can cause serious injury. Tell the healthcare provider if you have any metal in or on your body.
- An EKG records the electrical activity of your heart. It is used to check for an abnormal heart rhythm caused by MR.
- A stress test helps healthcare providers see how well your mitral valve works under stress. Healthcare providers may place stress on your mitral valve with exercise or medicine.
- Cardiac catheterization is a procedure to check how well your heart is pumping blood. It is also used to measure pressure in different parts of your heart. A catheter (long thin tube) is inserted into your arm, neck, or groin and moved into your heart. An x-ray may be used to guide the tube to the right place. Contrast liquid may be used to help your heart show up better in the pictures. Tell the healthcare provider if you have ever had an allergic reaction to contrast liquid.
How is MR treated?
Treatment may not be needed if your condition does not cause symptoms.
- Medicines may be given to lower your blood pressure or to remove extra fluid.
- Surgery may be used to repair or replace your mitral valve if you have severe symptoms.
How can I manage MR?
- Maintain a healthy weight. Being overweight can increase your risk for high blood pressure, diabetes, and coronary artery disease. These conditions can make your symptoms worse. Ask your healthcare provider what a healthy weight is for you. Ask him or her to help you create a weight loss plan if you are overweight.
- Do not smoke. Nicotine and other chemicals in cigarettes and cigars can cause lung and heart damage. Ask your healthcare provider for information if you currently smoke and need help to quit. E-cigarettes or smokeless tobacco still contain nicotine. Talk to your healthcare provider before you use these products.
- Limit or do not drink alcohol. Ask your healthcare provider if it is okay for you to drink alcohol. Alcohol can increase your risk for high blood pressure and coronary artery disease. Your provider can tell you how many drinks are okay to have within 24 hours or within 1 week. A drink of alcohol is 12 ounces of beer, 5 ounces of wine, or 1½ ounces of liquor.
- Eat heart-healthy foods. Heart-healthy foods include salmon, tuna, walnuts, whole-grain breads, low-fat dairy products, beans, and oils such as olive or canola oil. A dietitian or your provider can give you more information on meal plans such as the DASH (Dietary Approaches to Stop Hypertension) eating plan. The DASH plan is low in sodium, processed sugar, unhealthy fats, and total fat. It is high in potassium, calcium, and fiber. These can be found in vegetables, fruit, and whole-grain foods.

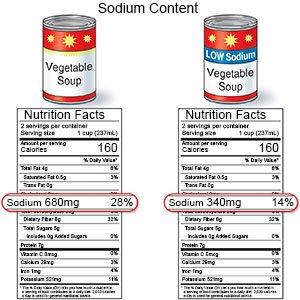
- Limit sodium (salt) as directed. Too much sodium can affect your fluid balance. Check labels to find low-sodium or no-salt-added foods. You can also make small changes to get less salt. For example, if you add salt while you cook, do not add more salt at the table. Ask your healthcare provider or dietitian for more ways to cut down on salt.
- Exercise as directed. Exercise can help keep your heart healthy. Ask your healthcare provider what activities are safe for you to do. The amount and type of exercise that is safe may depend on how severe your condition is.
- Talk to your healthcare provider about pregnancy. If you are a woman and want to get pregnant, talk to your healthcare provider. Pregnancy makes your heart work harder. You and your baby may need to be monitored by specialists during your pregnancy.
- Ask your healthcare provider if you should take antibiotics before certain procedures. Some procedures may allow bacteria to get into your blood and travel to your heart. This can make your condition worse.
- Ask about vaccines you may need. Certain diseases are dangerous for a person who has MR. Vaccines help lower your risk for infections that can lead to disease. Get a flu vaccine as soon as recommended each year, usually in September or October. Your healthcare provider can tell you if you also need other vaccines, and when to get them.
What can I do to prevent MR?
- Manage health conditions that can lead to MR. Your healthcare provider or a specialist can help you manage a condition such as lupus or Marfan syndrome.
- Get treatment for strep throat. Strep throat can lead to rheumatic fever, a cause of MR.
- Talk to your healthcare provider before you take any new medicine. Some medicines can increase your risk for MR.
Call your local emergency number (911 in the US) or have someone call if:
- You have any of the following signs of a heart attack:
- Squeezing, pressure, or pain in your chest
- You may also have any of the following:
- Discomfort or pain in your back, neck, jaw, stomach, or arm
- Shortness of breath
- Nausea or vomiting
- Lightheadedness or a sudden cold sweat
- You have any of the following signs of a stroke:
- Numbness or drooping on one side of your face
- Weakness in an arm or leg
- Confusion or difficulty speaking
- Dizziness, a severe headache, or vision loss
When should I seek immediate care?
- You have chest pain when you move around that goes away when you are still.
- You have increasing shortness of breath.
- You faint.
When should I call my doctor?
- The veins in your neck look swollen or are bulging.
- You have increased swelling in your legs or ankles.
- Your heart beats faster than usual.
- You feel your heart flutter often.
- You have questions or concerns about your condition or care.
Care Agreement
You have the right to help plan your care. Learn about your health condition and how it may be treated. Discuss treatment options with your healthcare providers to decide what care you want to receive. You always have the right to refuse treatment. The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
Learn more about Mitral Regurgitation
Treatment options
- Medications for Mitral Insufficiency
- Medications for Mitral Stenosis
- Medications for Valvular Heart Disease
Care guides
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
