Pancreaticoduodenectomy
Medically reviewed by Drugs.com. Last updated on Aug 4, 2025.
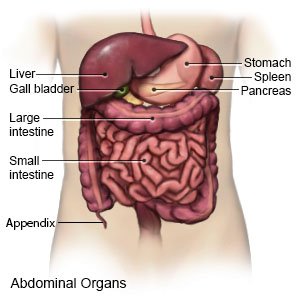
Pancreaticoduodenectomy is surgery to remove the head of your pancreas, your duodenum, the end of your bile duct, and your gallbladder. Part of your stomach may also be removed. The surgery is also called a Whipple procedure. This surgery is done when a cancerous tumor has been found in the head of your pancreas. The tumor may also be at the place where your bile duct and pancreatic duct meet, or the first part of your duodenum.
 |
WHILE YOU ARE HERE:
Before your surgery:
- Informed consent is a legal document that explains the tests, treatments, or procedures that you may need. Informed consent means you understand what will be done and can make decisions about what you want. You give your permission when you sign the consent form. You can have someone sign this form for you if you are not able to sign it. You have the right to understand your medical care in words you know. Before you sign the consent form, understand the risks and benefits of what will be done. Make sure all your questions are answered.
- An IV is a small tube placed in your vein that is used to give you medicine or liquids.
- General anesthesia will keep you asleep and free from pain during surgery. Anesthesia may be given through your IV. You may instead breathe it in through a mask or a tube placed down your throat. The tube may cause you to have a sore throat when you wake up.
During your surgery:
- Your surgeon will make an incision in your abdomen. He or she will remove parts of your pancreas and bile duct, and your duodenum and gallbladder. Part of your stomach may also be removed. Your surgeon will then reconnect your stomach, pancreas, bile duct, and jejunum.
- A feeding tube may be inserted into your intestines. A drain may be placed to remove extra blood or fluid from the surgery area. Your incision will be closed with stitches or surgical tape and covered with bandages.
Related medications
After your surgery:
You will be taken to a room to rest until you are fully awake. You will be monitored closely for any problems. Do not get out of bed until your healthcare provider says it is okay. You will then be able to go home or be taken to a hospital room.
- Drains will be removed when your surgery area stops draining blood and fluid.
- A nasogastric (NG) tube is put into your nose and down into your stomach. The tube may be attached to suction to keep your stomach empty. You may have an NG tube after surgery to prevent you from vomiting. An NG tube may help get your bowels working. The NG tube is normally removed a day after surgery.
- A Foley catheter may be placed for a few days after your surgery. A Foley catheter is a tube that is put into your bladder to drain your urine into a bag. Keep the bag of urine below your waist. Do not pull on the catheter because this may cause pain and bleeding, and the catheter may come out. Do not allow the catheter tubing to kink because this will block the flow of urine.
- Intake and output may be measured. Healthcare providers will keep track of the amount of liquid you are getting. They also may need to know how much you are urinating. Ask healthcare providers if they need to measure or collect your urine.
- You will be helped to walk around after surgery. Movement will help prevent blood clots. You may also be given exercises to do in bed. Do not get out of bed on your own until your healthcare provider says you can. Talk to a healthcare provider before you get up the first time.
- You will be able to have liquids and foods when your stomach function returns. You may be given ice chips at first. Then you will get liquids such as water, broth, juice, and clear soft drinks. You may then be given soft foods, such as cooked cereal and applesauce. You may need to be on a pureed or soft diet for a few days to a couple of weeks after your surgery.
- Pneumatic boots are inflatable boots that are put on your legs. They are connected to an air pump that tightens and loosens different areas of the boots. This helps improve blood flow to prevent clots.
- Medicines may be given to prevent or treat pain, nausea, or a bacterial infection. You may also need medicine to stop your skin from itching.
RISKS:
Surgery may damage to your pancreas, stomach, small intestines, and other organs, blood vessels, or nerves. It may increase your risk for bleeding or an infection. Bile and other digestive juices may leak into your abdomen. You may have trouble absorbing food and nutrients after your surgery. A fistula (abnormal connection between organs) may form. You may develop diabetes. Even after surgery, the tumor may spread. You may develop a life-threatening blood clot.
CARE AGREEMENT:
You have the right to help plan your care. Learn about your health condition and how it may be treated. Discuss treatment options with your healthcare providers to decide what care you want to receive. You always have the right to refuse treatment.© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
