Mitral Valve Replacement
Medically reviewed by Drugs.com. Last updated on Aug 4, 2025.
AMBULATORY CARE:
What you need to know about mitral valve replacement:
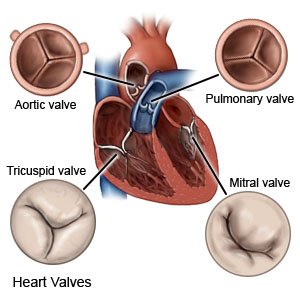
Mitral valve replacement is open heart surgery to replace all or part of the mitral valve. The mitral valve normally opens and closes to let blood pass through the heart. If your mitral valve is damaged, blood may not flow as it should through your heart. Full recovery may take from weeks to months.
 |
How to prepare for mitral valve replacement:
Your healthcare provider will tell you how to prepare for your valve replacement surgery. Make arrangements to be in the hospital for up to 2 weeks after surgery. You may be admitted to the hospital the day before your surgery is scheduled. You will have tests to help healthcare providers plan for your surgery. Your surgeon will talk to you about the surgery and what to expect. You will not be able to eat or drink after midnight the night before your surgery.
What will happen during your surgery:
- You will be given general anesthesia medicine to make you sleep. One or more incisions will be made in your chest. Healthcare providers will connect your heart to a heart-lung bypass machine. This machine does the work of your heart and lungs during surgery.
- Part or all of your mitral valve will be removed. Your mitral valve will be replaced with a tissue valve or mechanical valve and sewn in place. Healthcare providers may put wires your chest that stay in for a short time after surgery. The wires can be used to improve your heartbeat. The bypass machine will be removed, and your own heart and lungs will start working again. The incision in your chest will be closed with stitches or staples and covered with a bandage. The bandage keeps the area clean and dry to help prevent infection.
What to expect after your surgery:
- You will be monitored until you are awake.
- You will spend up to 2 days in the intensive care unit (ICU).
- A physical therapist will help you get up and walk after your surgery.
- You will need tests to make sure your heart is working properly.
Risks of mitral valve replacement surgery:
- You may bleed or get an infection during or after surgery. After surgery, your new valve may not work or your heart may not beat as it should. Over time the new valve or area around it may become damaged. Symptoms you had before the surgery may come back or get worse after surgery. You may need to have heart valve surgery again.
- You may get a blood clot in your arm or leg. This may become life-threatening. You may need medicine to prevent blood clots for the rest of your life after your surgery.
Call your local emergency number (911 in the US) for any of the following:
- You have any of the following signs of a heart attack:
- Squeezing, pressure, or pain in your chest
- You may also have any of the following:
- Discomfort or pain in your back, neck, jaw, stomach, or arm
- Shortness of breath
- Nausea or vomiting
- Lightheadedness or a sudden cold sweat
- You have any of the following signs of a stroke:
- Numbness or drooping on one side of your face
- Weakness in an arm or leg
- Confusion or difficulty speaking
- Dizziness, a severe headache, or vision loss
Seek care immediately if:
- Your arm or leg feels warm, tender, and painful. It may look swollen and red.
- You have chest pain when you take a deep breath or cough. You may cough up blood.
Related medications
Treatment options
The following list of medications are related to or used in the treatment of this condition.
Call your cardiologist or doctor if:
- You have a fever.
- Your heart is beating faster or slower than normal.
- Your hands, ankles, or feet are swollen.
- You urinate less, or not at all.
- You feel extremely tired or weak.
- You have questions or concerns about your condition or care.
Medicines:
- Blood thinners help prevent blood clots. Clots can cause strokes, heart attacks, and death. Many types of blood thinners are available. Your healthcare provider will give you specific instructions for the type you are given. The following are general safety guidelines to follow while you are taking a blood thinner:
- Watch for bleeding and bruising. Watch for bleeding from your gums or nose. Watch for blood in your urine and bowel movements. Use a soft washcloth on your skin, and a soft toothbrush to brush your teeth. This can keep your skin and gums from bleeding. If you shave, use an electric shaver. Do not play contact sports.
- Tell your dentist and other healthcare providers that you take a blood thinner. Wear a bracelet or necklace that says you take this medicine.
- Do not start or stop any other medicines or supplements unless your healthcare provider tells you to. Many medicines and supplements cannot be used with blood thinners.
- Take your blood thinner exactly as prescribed by your healthcare provider. Do not skip a dose or take less than prescribed. Tell your provider right away if you forget to take your blood thinner, or if you take too much.
- Take your medicine as directed. Contact your healthcare provider if you think your medicine is not helping or if you have side effects. Tell your provider if you are allergic to any medicine. Keep a list of the medicines, vitamins, and herbs you take. Include the amounts, and when and why you take them. Bring the list or the pill bottles to follow-up visits. Carry your medicine list with you in case of an emergency.
Care for your incision site:
Ask your healthcare provider when your site can get wet. Carefully wash around the site with soap and water. Do not scrub the area. You can let soap and water gently run over your incision site. Gently pat dry the area and put on new, clean bandages as directed. Check your site every day for signs of infection, such as swelling, pus, or redness. Do not put lotions or powders on the site. Do not take a bath or swim until your healthcare provider says it is okay. These activities can increase your risk for an infection.
Go to cardiac rehabilitation (rehab), if directed:
Cardiac rehab is a program supervised by healthcare providers. A cardiac rehab team includes doctors, nurses, exercise specialists, physical and occupational therapists, dietitians, and mental health providers. The providers will teach you ways to strengthen your heart and prevent future heart problems. The program can help you recover from your surgery and manage your heart condition. Cardiac rehab may last for several weeks or months, depending on your condition.
Activity:
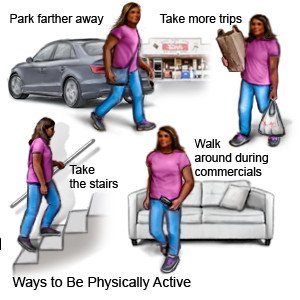
Your healthcare provider will give you specific instructions. You may also get instructions if you go to cardiac rehab. The following is a general guideline to help reduce your risk for problems after your procedure:
- Do not lift objects heavier than 5 pounds.
- Do not do activities that cause you to hold your breath, grunt, or strain.
- Take short walks around the house several times a day. This will help prevent blood clots.
- Ask your healthcare provider what other activities are safe for you to do. Also ask when you can return to your normal activities.
Self-care:
- Tell healthcare providers about your valve replacement. You may need to take antibiotics before certain medical and dental procedures. Antibiotics will reduce your risk for infection.
- Eat heart-healthy foods. You may need to eat foods that are low in salt, fat, or cholesterol. Healthy foods include fruits, vegetables, whole-grain breads, low-fat dairy products, beans, lean meats, and fish. Ask your healthcare provider for more information about a heart healthy diet.

- Do not smoke. Nicotine and other chemicals in cigarettes and cigars can cause heart and lung damage. Nicotine can also slow healing. Ask your healthcare provider for information if you currently smoke and need help to quit. E-cigarettes or smokeless tobacco still contain nicotine. Talk to your healthcare provider before you use these products.
- Do not drink alcohol. Ask your cardiologist if it is safe for you to drink alcohol. Alcohol can increase your risk for high blood pressure, diabetes, and coronary artery disease.
- Maintain a healthy weight. Ask your healthcare provider what a healthy weight is for you. Extra weight can increase the stress on your heart. Ask him or her to help you create a weight loss plan if you are overweight.
- Exercise as directed after you recover. Your healthcare provider can help you create an exercise plan that is right for you. Exercise will help keep your heart healthy.
Follow up with your cardiologist or doctor as directed:
You will need to have repeat tests. You may also need staples or stitches removed. Your provider will make sure the valve is working properly. Write down your questions so you remember to ask them during your visits.
© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.
Learn more about Mitral Valve Replacement
Treatment options
Symptoms and treatments
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
