Left Atrial Appendage Closure
Medically reviewed by Drugs.com. Last updated on Apr 6, 2025.
AMBULATORY CARE:
What you need to know about left atrial appendage closure (LAAC):
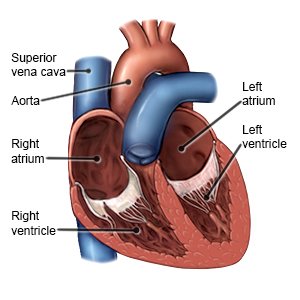
LAAC is a procedure to block or close the left atrial appendage. The appendage is a small pouch in the heart muscle that is connected to your left atrium. Blood clots may form in the appendage if you have atrial fibrillation. This increases your risk for stroke. LAAC helps prevent blood clots from entering your bloodstream and lowers your risk for stroke.
 |
How to prepare for LAAC:
- Your healthcare provider will tell you how to prepare. You may be told not to eat or drink anything after midnight on the day of your procedure. Arrange to have someone drive you home when you are discharged.
- Tell your provider about all medicines you currently take. Your provider will tell you if you need to start or stop any medicine for the procedure, and when to do so. You may need to take a blood thinner before your procedure. Your provider will tell you which medicines to take or not take on the day of the procedure.
- Tell your provider about any allergies you have, including to anesthesia or medicines. You may be given an antibiotic to help prevent a bacterial infection.
- Your provider will tell you if you need any tests before your procedure, and when to have them. You may need an echocardiogram, CT, or MRI. These tests help show the structure of your heart so your provider can plan your procedure.
What will happen during LAAC:
- You will be given general anesthesia to keep you asleep and free from pain during the procedure. Your provider will insert a catheter into a vein near your groin or under your sternum (breastbone). The catheter will be guided to your heart using fluoroscopy (continuous x-rays).
- A hole will be made in the wall that separates your right and left atria. The catheter will go through the hole so it can reach the left appendage. Your provider will insert a device into the opening of the appendage. The device may have netting or mesh to block blood clots. Your provider may instead use a suture or other device to close or clamp the opening.
- Imaging tests will be done to make sure the device completely blocks the opening. Your provider will make sure the device is secure and stays in place. Your provider will then remove the catheter. The catheter site will be closed and covered with a bandage.
What to expect after LAAC:
You may need to stay in the hospital overnight or longer. You may need to take blood thinners and aspirin. Your healthcare provider will tell you how long you will need these medicines.
Risks of LAAC:
You may bleed more than expected or develop an infection. You may develop a blood clot near the device. Your device may move out of place. You may need another procedure or surgery to fix this. The hole between the atria in your heart may not close. You may have a stroke during the procedure. The outer wall of your heart could be punctured. You will need immediate surgery to fix this. You may have a buildup of fluid around your heart that prevents it from pumping correctly. This can be life-threatening.
Drugs used to treat this and similar conditions
Aspirin
Aspirin is used to treat mild to moderate pain and to reduce fever or inflammation. Learn about ...
Plavix
Plavix (clopidogrel) is used to prevent blood clots after a recent heart attack or stroke. Includes ...
Otezla
Otezla (apremilast) is used to treat plaque psoriasis, psoriatic arthritis, and oral ulcers ...
Bayer Aspirin
Bayer Aspirin is used for angina, angina pectoris prophylaxis, ankylosing spondylitis ...
Easprin
Easprin is used for angina, angina pectoris prophylaxis, ankylosing spondylitis, antiphospholipid ...
Ecotrin
Ecotrin is used for angina, angina pectoris prophylaxis, ankylosing spondylitis, antiphospholipid ...
Aspir-Low
Aspir-Low is used for angina, angina pectoris prophylaxis, heart attack, ischemic stroke, ischemic ...
Arthritis Pain
Arthritis Pain is used for angina, angina pectoris prophylaxis, ankylosing spondylitis ...
Vazalore
Vazalore is used for angina, angina pectoris prophylaxis, ankylosing spondylitis, antiphospholipid ...
Call your local emergency number (911 in the US), or have someone call if:
- You have any of the following signs of a heart attack:
- Squeezing, pressure, or pain in your chest
- You may also have any of the following:
- Discomfort or pain in your back, neck, jaw, stomach, or arm
- Shortness of breath
- Nausea or vomiting
- Lightheadedness or a sudden cold sweat
- You have any of the following signs of a stroke:
- Numbness or drooping on one side of your face
- Weakness in an arm or leg
- Confusion or difficulty speaking
- Dizziness, a severe headache, or vision loss
- You have shortness of breath and sharp chest pain.
- You have lightheadedness, dizziness, or confusion.
Seek care immediately if:
- Your heart is beating faster or slower than usual.
- Your catheter site has increased bruising or swelling.
Call your doctor if:
- You have questions or concerns about your condition or care.
Medicines:
Blood thinners help prevent blood clots. Clots can cause strokes, heart attacks, and death. Many types of blood thinners are available. Your healthcare provider will give you specific instructions for the type you are given. The following are general safety guidelines to follow while you are taking a blood thinner:
- Watch for bleeding and bruising. Watch for bleeding from your gums or nose. Watch for blood in your urine and bowel movements. Use a soft washcloth on your skin, and a soft toothbrush to brush your teeth. This can keep your skin and gums from bleeding. If you shave, use an electric shaver. Do not play contact sports.
- Tell your dentist and other healthcare providers that you take a blood thinner. Wear a bracelet or necklace that says you take this medicine.
- Do not start or stop any other medicines or supplements unless your healthcare provider tells you to. Many medicines and supplements cannot be used with blood thinners.
- Take your blood thinner exactly as prescribed by your healthcare provider. Do not skip a dose or take less than prescribed. Tell your provider right away if you forget to take your blood thinner, or if you take too much.
Follow up with your doctor as directed:
You will need imaging tests to make sure the closure is not leaking. Your doctor will also help manage your medicines after the procedure. Write down your questions so you remember to ask them during your visits.
© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
