Ear Infection in Children
Medically reviewed by Drugs.com. Last updated on Aug 4, 2025.
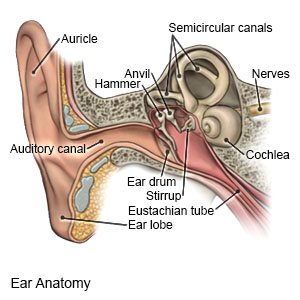
An ear infection is also called otitis media. Ear infections can happen any time during the year. They are most common during the winter and spring months. Your child may have an ear infection more than once.
 |
DISCHARGE INSTRUCTIONS:
Return to the emergency department if:
- Your child seems confused or cannot stay awake.
- Your child has a stiff neck, headache, and a fever.
Call your child's doctor if:
- You see blood or pus draining from your child's ear.
- Your child has a fever.
- Your child is still not eating or drinking 24 hours after he or she takes medicine.
- Your child has pain behind his or her ear or when you move the earlobe.
- Your child's ear is sticking out from his or her head.
- Your child still has signs and symptoms of an ear infection 48 hours after he or she takes medicine.
- You have questions or concerns about your child's condition or care.
Related medications
Treatment for an ear infection
may include any of the following:
- Medicines:
- Acetaminophen decreases pain and fever. It is available without a doctor's order. Ask how much to give your child and how often to give it. Follow directions. Read the labels of all other medicines your child uses to see if they also contain acetaminophen, or ask your child's doctor or pharmacist. Acetaminophen can cause liver damage if not taken correctly.
- NSAIDs , such as ibuprofen, help decrease swelling, pain, and fever. This medicine is available with or without a doctor's order. NSAIDs can cause stomach bleeding or kidney problems in certain people. If your child takes blood thinner medicine, always ask if NSAIDs are safe for him or her. Always read the medicine label and follow directions. Do not give these medicines to children younger than 6 months without direction from a healthcare provider.
- Ear drops help treat your child's ear pain.
- Antibiotics help treat a bacterial infection.
- Give your child's medicine as directed. Contact your child's healthcare provider if you think the medicine is not working as expected. Tell the provider if your child is allergic to any medicine. Keep a current list of the medicines, vitamins, and herbs your child takes. Include the amounts, and when, how, and why they are taken. Bring the list or the medicines in their containers to follow-up visits. Carry your child's medicine list with you in case of an emergency.
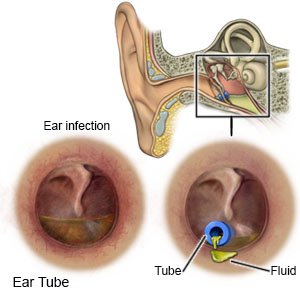
- Ear tubes are used to keep fluid from collecting in your child's ears. Your child may need these to help prevent ear infections or hearing loss. Ask your child's healthcare provider for more information on ear tubes.
Care for your child at home:
- Have your child lie with his or her infected ear facing down to allow fluid to drain from the ear.
- Apply heat on your child's ear for 15 to 20 minutes, 3 to 4 times a day or as directed. You can apply heat with an electric heating pad, hot water bottle, or warm compress. Always put a cloth between your child's skin and the heat pack to prevent burns. Heat helps decrease pain.
- Apply ice on your child's ear for 15 to 20 minutes, 3 to 4 times a day for 2 days or as directed. Use an ice pack, or put crushed ice in a plastic bag. Cover it with a towel before you apply it to your child's ear. Ice decreases swelling and pain.
- Ask about ways to keep water out of your child's ears when he or she bathes or swims.
Prevent an ear infection:
- Wash your and your child's hands often to help prevent the spread of germs. Ask everyone in your house to wash their hands with soap and water. Ask them to wash after they use the bathroom or change a diaper. Remind them to wash before they prepare or eat food.

- Keep your child away from people who are ill, such as sick playmates. Germs spread easily and quickly in daycare centers.
- If possible, breastfeed your baby. Your baby may be less likely to get an ear infection if he or she is breastfed.
- Do not give your child a bottle while he or she is lying down. This may cause liquid from the sinuses to leak into his or her eustachian tube.
- Keep your child away from cigarette smoke. Smoke can make an ear infection worse. Move your child away from a person who is smoking. If you currently smoke, do not smoke near your child. Ask your healthcare provider for information if you want help to quit smoking.
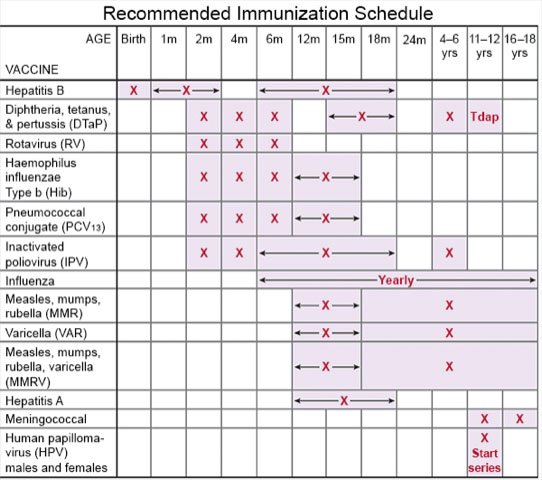
- Ask about vaccines. Vaccines may help prevent infections that can cause an ear infection. Have your child get a yearly flu vaccine as soon as recommended, usually in September or October. Ask about other vaccines your child needs and when he or she should get them.
Follow up with your child's doctor as directed:
Write down your questions so you remember to ask them during your visits.
© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.
Learn more about Ear Infection
- Antibiotics 101: Common Names, Types & Their Uses
- Can You Drink Alcohol with Antibiotics?
- Middle Ear Infection FAQs (Acute Otitis Media)
Treatment options
- Medications for Chronic Otitis Media
- Medications for Infection
- Medications for Otitis Media with Perforation of Ear Drum
Care guides
- Barotitis Media
- Ear Infection
- Ear Infection in Children
- Eustachian Tube Dysfunction
- Fluid in the Ear (Serous Otitis Media)
Symptoms and treatments
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
