Venlafaxine Side Effects
Medically reviewed by Drugs.com. Last updated on Sep 23, 2024.
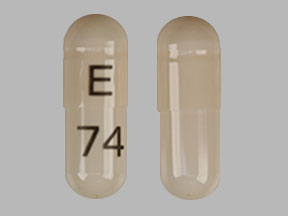
Applies to venlafaxine: oral capsule extended release, oral tablet, oral tablet extended release.
Important warnings
This medicine can cause some serious health issues
Oral route (capsule, extended release)
Antidepressants increased the risk of suicidal thoughts and behavior in pediatric and young adult patients in short-term studies.
Closely monitor all antidepressant-treated patients for clinical worsening, and emergence of suicidal thoughts and behaviors.
Venlafaxine hydrochloride is not approved for use in pediatric patients.
Oral route (tablet; tablet, extended release)
Antidepressants increased the risk compared to placebo of suicidal thinking and behavior (suicidality) in children, adolescents, and young adults in short-term studies of Major Depressive Disorder (MDD) and other psychiatric disorders.
Anyone considering the use of venlafaxine hydrochloride or any other antidepressant in a child, adolescent, or young adult must balance this risk with the clinical need.
Short-term studies did not show an increase in the risk of suicidality with antidepressants compared to placebo in adults beyond age 24; there was a reduction in risk with antidepressants compared to placebo in adults aged 65 and older.
Depression and certain other psychiatric disorders are themselves associated with increases in the risk of suicide.
Patients of all ages who are started on antidepressant therapy should be monitored appropriately and observed closely for clinical worsening, suicidality, or unusual changes in behavior.
Families and caregivers should be advised of the need for close observation and communication with the prescriber.
Venlafaxine is not approved for use in pediatric patients
Precautions
If you will be taking this medicine for a long time, it is very important that your doctor check you at regular visits. This will allow your doctor to see if the medicine is working properly and to decide if you should continue to take it.
Do not take venlafaxine with a monoamine oxidase (MAO) inhibitor (eg, isocarboxazid (Marplan®), phenelzine (Nardil®)], selegiline (Eldepryl®), tranylcypromine (Parnate®)). Do not start taking venlafaxine during the 14 days after you stop a MAO inhibitor and wait 7 days after stopping venlafaxine before you start taking a MAO inhibitor. If you take them together or do not wait the proper amount of time, you may develop confusion, agitation, restlessness, stomach or intestinal symptoms, a sudden high body temperature, an extremely high blood pressure, or severe seizures.
Venlafaxine may cause a serious condition called serotonin syndrome if taken together with certain medicines. Do not use venlafaxine with buspirone (Buspar®), fentanyl (Abstral®, Duragesic®), linezolid (Zyvox®), lithium (Eskalith®, Lithobid®), methylene blue injection, tryptophan, St John's wort, amphetamines, or some pain or migraine medicines (eg, meperidine, methadone, rizatriptan, sumatriptan, tramadol, Demerol®, Frova®, Imitrex®, Maxalt®, Methadose®, Relpax®, Ultram®, Zomig®). Check with your doctor first before taking any other medicines with venlafaxine.
This medicine may cause some teenagers and young adults to be agitated, irritable, or display other abnormal behaviors. It may also cause some people to have suicidal thoughts and tendencies or to become more depressed. Some people may have trouble sleeping, get upset easily, have a big increase in energy, or start to act reckless. If you or your caregiver notice any of these unwanted effects, tell your doctor right away. Let the doctor know if you or anyone in your family has bipolar disorder (manic-depressive) or has tried to commit suicide.
Do not suddenly Stop taking venlafaxine without checking first with your doctor. Your doctor may want you to gradually reduce the amount you are taking before stopping it completely. This will decrease the chance of side effects, including agitation, anxiety, blurred vision, confusion, diarrhea, dizziness, fast or irregular heartbeat, headache, irritability, nausea or vomiting, numbness or tingling feeling, restlessness, seizures, sweating, thoughts of hurting yourself or others, trouble sleeping, unusual dreams, or unusual drowsiness, tiredness, or weakness.
This medicine may cause hyponatremia (low sodium in the blood). This is more common in elderly patients, those who take diuretic medicines, or those who have a low amount of fluid in the body due to severe diarrhea or vomiting. Check with your doctor right away if you have a headache, trouble concentrating, memory problems, confusion, weakness, or feel unsteady when standing.
Venlafaxine may increase your risk for bleeding problems. Make sure your doctor knows if you are also using other medicines that thin the blood, including NSAIDs (eg, aspirin, diclofenac, ibuprofen, naproxen, Advil®, Aleve®, Celebrex®, Voltaren®) or warfarin (Coumadin®, Jantoven®).
Tell your doctor right away if you are having chest pain or discomfort, dry cough, fever, general feeling of tiredness or weakness, skin rash, or trouble breathing with this medicine. These might be symptoms of a serious lung problem, including interstitial lung disease and eosinophilic pneumonia.
Venlafaxine may cause some people to become drowsy or have blurred vision. Make sure you know how you react to this medicine before you drive, use machines, or do anything else that could be dangerous if you are not alert or able to see clearly. It is best to avoid alcohol with venlafaxine.
Before you have any medical tests, tell the medical doctor in charge that you are taking this medicine. The results of some tests may be affected by this medicine.
Check with your doctor right away if you have decreased interest in sexual intercourse, delayed or inability to have and orgasm in women, inability to have or keep an erection in men, or loss in sexual ability, desire, drive, or performance. These could be symptoms of sexual dysfunction.
Do not take other medicines unless they have been discussed with your doctor. This includes prescription or nonprescription (over-the-counter [OTC]) medicines and herbal or vitamin supplements.
Serious side effects of venlafaxine
Along with its needed effects, venlafaxine may cause some unwanted effects. Although not all of these side effects may occur, if they do occur they may need medical attention.
Check with your doctor immediately if any of the following side effects occur while taking venlafaxine:
More common side effects
- change or problem with discharge of semen
- decreased interest in sexual intercourse
- inability to have or keep an erection
- lack or loss of strength
- loss in sexual ability, desire, drive, or performance
- severe headache
- sweating
Less common side effects
- blurred vision
- chest pain
- delayed or inability to have an orgasm
- fast or irregular heartbeat
- mood or mental changes
- ringing or buzzing in the ears
- suicidal thoughts
Rare side effects
- actions that are out of control
- high fever
- irritability
- itching or skin rash
- lightheadedness or fainting, especially when getting up suddenly from a sitting or lying position
- menstrual changes
- nervousness
- problems with urinating or holding urine
- seizures
- severe muscle stiffness
- talking, feeling, and acting with excitement that you cannot control
- trouble breathing
- unusually pale skin
Incidence not known
- agitation
- bloody, black, or tarry stools
- bloody stool or urine
- dark urine
- decreased frequency or amount of urine
- diarrhea
- drowsiness
- fever
- general feeling of tiredness or weakness
- headache
- increased thirst
- light-colored stools
- muscle cramps, spasms, or pain
- nausea or vomiting
- nosebleeds
- overactive reflexes
- poor coordination
- red or purple spots on the skin
- restlessness
- shivering
- stomach pain on the upper right side
- swelling of the face, lower legs, ankles, hands, or fingers
- trembling or shaking that is hard to control
- twitching
- unusual bruising
- unusual tiredness or weakness
- vomiting of blood or material that looks like coffee grounds
- yellow eyes or skin
Other side effects of venlafaxine
Some side effects of venlafaxine may occur that usually do not need medical attention. These side effects may go away during treatment as your body adjusts to the medicine. Also, your health care professional may be able to tell you about ways to prevent or reduce some of these side effects.
Check with your health care professional if any of the following side effects continue or are bothersome or if you have any questions about them:
More common side effects
- abnormal dreams
- chills
- constipation
- decrease in sexual desire or ability
- diarrhea
- dry mouth
- heartburn
- increased sweating
- loss of appetite
- nausea
- stomach pain or gas
- stuffy or runny nose
- tingling, burning, or prickly sensations
- trouble sleeping
- vomiting
- weight loss
Less common side effects
- change in taste
- muscle tension
- yawning
Incidence not known
- decrease in smell
- loss of sense of smell
- night sweats
See also:
Auvelity
Auvelity (dextromethorphan and bupropion) is used to treat major depressive disorder. Includes ...
Paracetamol
Paracetamol (Panadol, Calpol, Alvedon) is a widely used over-the-counter painkiller and fever ...
Vraylar
Vraylar is a once a day antipsychotic medication used to treat mental health or mood disorders ...
Tylenol
Tylenol is a pain reliever and a fever reducer used to treat many conditions such as headaches ...
Cymbalta
Cymbalta (duloxetine) is used to treat major depressive disorder, general anxiety disorder and ...
Naproxen
Naproxen is a nonsteroidal anti-inflammatory drug used to treat pain or inflammation caused by ...
Oxycodone
Oxycodone is an opioid analgesic used to treat moderate to severe pain; it has a high potential for ...
Cyclobenzaprine
Cyclobenzaprine is a muscle relaxant and works by blocking pain sensations. Includes ...
Tramadol
Tramadol is an opioid medication that may be used to treat moderate to moderately severe chronic ...
For healthcare professionals
Applies to venlafaxine: oral capsule extended release, oral tablet, oral tablet extended release.
General adverse events
The most commonly reported side effects were nausea, headache, somnolence, and dizziness.[Ref]
Gastrointestinal
- Very common (10% or more): Nausea (up to 58%), dry mouth (up to 22%), constipation (up to 15%)
- Common (1% to 10%): Abdominal pain, diarrhea, dyspepsia, eructation, flatulence, vomiting
- Uncommon (0.1% to 1%): Circumoral paresthesia, colitis, dysphagia, esophagitis, gastritis, gastroenteritis, gastrointestinal hemorrhage, gastrointestinal ulcer, gingivitis, glossitis, hemorrhoids, melena, mouth ulceration, oral moniliasis, rectal hemorrhage, stomatitis, tongue edema
- Rare (less than 0.1%): Abdominal distention, buccoglossal syndrome, cheilitis, cholecystitis, cholelithiasis, duodenitis, esophageal spasm, gastroesophageal reflux disease, gum hemorrhage, hematemesis, hyperchlorhydria, ileitis, increased salivation, intestinal obstruction, pancreatitis, parotitis, periodontitis, proctitis, salivary gland enlargement, soft stools, tongue discoloration[Ref]
Nervous system
- Very common (10% or more): Headache (up to 38%), somnolence (up to 26.1%), dizziness (up to 23.9%), tremor (up to 10.2%)
- Common (1% to 10%): Akathisia, amnesia, dysgeusia, hypertonia, hypesthesia, increased muscle tone, migraine, paresthesia, sedation, taste perversion, vertigo
- Uncommon (0.1% to 1%): Abnormal coordination, abnormal speech, ataxia, balance disorder, central nervous system (CNS) stimulation, dyskinesia, hyperesthesia, hyperkinesia, hypotonia, incoordination, myoclonus, neuralgia, neuropathy, parosmia, seizure, syncope, stupor, taste loss, visual field defect
- Rare (0.1% to 0.01%): Abnormal gait, akinesia, aphasia, bradykinesia, cerebral ischemia, cerebrovascular accident, convulsion, dementia, dystonia, facial paralysis, Guillain-Barre Syndrome, hypokinesia, loss of consciousness, neuritis, neuroleptic malignant syndrome (NMS), nystagmus, paresis, reflexes decreased, reflexes increased, serotonin syndrome, torticollis
- Very rare (less than 0.01%): Extrapyramidal reactions, tardive dyskinesia
- Frequency not reported: Impaired coordination, sensory disturbance
- Postmarketing reports: Coordination abnormal, impaired balance, involuntary movements, NMS-like reactions, shock-like electrical sensations[Ref]
Psychiatric
- Very common (10% or more): Insomnia (up to 24%), nervousness (up to 21.3%), abnormal orgasm (up to 12.5%), anxiety (up to 11.2%)
- Common (1% to 10%): Abnormal dreams, abnormal thinking, agitation, anorgasmia, confusion, depersonalization, depression, libido decreased, orgasm disturbance, orgasmic dysfunction
- Uncommon (0.1% to 1%): Apathy, bruxism, derealization, emotional lability, euphoria, hallucination, hostility, hypomania, libido increased, mania, manic reaction, psychosis, suicidal ideation, suicide attempt, withdrawal syndrome
- Rare (less than 0.1%): Alcohol abuse, delirium, delusions, homicidal ideation, hysteria, impulse control difficulties, paranoid reaction, psychotic depression, psychomotor restlessness
- Frequency not reported: Aggression, delayed orgasm, increased dreaming, intense dreams, nightmares, other sleep disorders, self-harm, sleep disturbances, suicidal behaviors, vivid dreams, withdrawal symptoms
- Postmarketing reports: Catatonia, confusional state, panic, paranoia, psychotic disorder[Ref]
Dermatologic
- Very common (10% or more): Sweating (up to 19.3%), night sweats (up to 11.4%)
- Common (1% to 10%): Ecchymosis, hyperhidrosis, pruritus, rash
- Uncommon (0.1% to 1%): Acne, alopecia, brittle nails, contact dermatitis, dry skin, eczema, face edema, maculopapular rash, photosensitivity reaction, psoriasis, skin hypertrophy, urticaria
- Rare (less than 0.1%): Cellulitis, erythema multiforme, erythema nodosum, exfoliative dermatitis, furunculosis, granuloma, hair discoloration, hirsutism, leukoderma, lichenoid dermatitis, miliaria, mucocutaneous hemorrhage, petechial rash, pruritic rash, purpura, pustular rash, seborrhea, skin atrophy, skin discoloration, skin striae, Stevens-Johnson syndrome, sweating decreased, toxic epidermal necrolysis, vesiculobullous rash[Ref]
Metabolic
- Very common (10% or more): Anorexia (up to 20%)
- Common (1% to 10%): Blood cholesterol increased, decreased appetite, increased appetite, weight gain, weight loss
- Uncommon (0.1% to 1%): Dehydration, hyperglycemia, hyperlipemia, hyperlipidemia, hypokalemia, hyponatremia, increased alkaline phosphatase, thirst
- Rare (less than 0.1%): Alcohol intolerance, diabetes mellitus, gout, hemochromatosis, hypercholesteremia, hyperkalemia, hyperphosphatemia, hyperuricemia, hypocholesteremia, hypoglycemia, hypophosphatemia, hypoproteinemia
- Frequency not reported: Height changes, loss of appetite, weight changes
- Postmarketing reports: Lactate dehydrogenase (LDH) increased[Ref]
Other
- Very common (10% or more): Asthenia (up to 19%)
- Common (1% to 10%): Accidental injury, chills, fatigue, fever, tinnitus, trauma
- Uncommon (0.1% to 1%): Hyperacusis, intentional injury, malaise, otitis media
- Rare (less than 0.1%): Abortion, deafness, energy increased, feeling drunk, healing abnormal, labyrinthitis, menopause, motion sickness, otitis externa
- Frequency not reported: Discontinuation syndrome, pain
- Postmarketing reports: Congenital anomalies[Ref]
Genitourinary
- Very common (10% or more): Abnormal ejaculation (up to 16%)
- Common (1% to 10%): Albuminuria, enlarged prostate, erectile dysfunction, impotence, metrorrhagia, pollakiuria, prostatic disorder, prostatitis, urinary frequency, urinary hesitation, urinary retention, urination impaired, vaginitis
- Uncommon (0.1% to 1%): Amenorrhea, bladder pain, breast pain, cystitis, dysuria, hematuria, leukorrhea, menorrhagia, nocturia, pelvic pain, polyuria, prostate irritability, pyuria, urinary incontinence, urinary urgency, vaginal hemorrhage
- Rare (less than 0.1%): Balanitis, breast discharge, breast engorgement, breast enlargement, calcium crystalluria, cervicitis, endometriosis, galactorrhea, hypercalcinuria, hypomenorrhea, lactation (female), mastitis, menstrual disorders associated with increased bleeding or increased irregular bleeding, ovarian cyst, orchitis, prolonged erection, salpingitis, urolithiasis, uterine hemorrhage, uterine spasm, vaginal dryness
- Frequency not reported: Delayed ejaculation, dysmenorrhea
- Postmarketing reports: Proteinuria[Ref]
Cardiovascular
- Common (1% to 10%): Chest pain, edema, hot flashes/hot flush, hypertension/increased blood pressure, palpitation, postural hypotension, substernal chest pain, tachycardia, vasodilation
- Uncommon (0.1% to 1%): Angina pectoris, arrhythmia, bradycardia, cold feet, cold hands, extrasystoles, hypotension, orthostatic hypotension, peripheral vascular disorder, thrombophlebitis
- Rare (less than 0.1%): Aortic aneurysm, arteritis, bigeminy, bundle branch block, capillary fragility, cardiovascular disorder (mitral valve and circulatory disturbance), coronary artery disease, congestive heart failure, cyanosis, ECG QT prolonged, first-degree atrioventricular block, heart arrest, hematoma, myocardial infarct, pallor, sinus arrhythmia, torsade de pointes, ventricular fibrillation, ventricular tachycardia
- Postmarketing reports: Atrial fibrillation, deep vein thrombophlebitis, ECG abnormalities, stress cardiomyopathy, supraventricular tachycardia, Takotsubo cardiomyopathy, ventricular extrasystole[Ref]
Respiratory
- Common (1% to 10%): Bronchitis, cough increased, dyspnea, pharyngitis, sinusitis, yawn/yawning
- Uncommon (0.1% to 1%): Asthma, chest congestion, epistaxis, hyperventilation, laryngismus, laryngitis, pneumonia, voice alteration
- Rare (less than 0.1%): Atelectasis, hemoptysis, hypoventilation, hypoxia, interstitial lung disease, larynx edema, pleurisy, pulmonary embolus, pulmonary eosinophilia, sleep apnea
- Frequency not reported: Rhinitis, upper respiratory infection, upper respiratory tract infection[Ref]
Ocular
- Common (1% to 10%): Abnormality of accommodation, abnormal vision, blurred vision, mydriasis
- Uncommon (0.1% to 1%): Cataract, conjunctivitis, corneal lesion, diplopia, dry eyes, eye pain, photophobia
- Rare (less than 0.1%): Angle-closure glaucoma, blepharitis, chromatopsia, conjunctival edema, decreased pupillary reflex, exophthalmos, eye hemorrhage, keratitis, miosis, papilledema, retinal hemorrhage, scleritis, subconjunctival hemorrhage, uveitis
- Frequency not reported: Difficulty focusing eyes[Ref]
Musculoskeletal
- Common (1% to 10%): Neck pain, trismus, twitching
- Uncommon (0.1% to 1%): arthritis, arthrosis, bone pain, bone spurs, bursitis, leg cramps, myasthenia, neck rigidity, tenosynovitis
- Rare (less than 0.1%): Muscle cramp, muscle spasms, musculoskeletal stiffness, myopathy, osteoporosis, osteosclerosis, pathological fracture, plantar fasciitis, rhabdomyolysis, rheumatoid arthritis, tendon rupture
- Frequency not reported: Arthralgia, back pain, myalgia
- Postmarketing reports: Bone fracture, creatine phosphokinase (CPK) increased[Ref]
Immunologic
- Common (1% to 10%): Flu syndrome, infection
- Uncommon (0.1% to 1%): Moniliasis
- Rare (less than 0.1%): Appendicitis, bacteremia[Ref]
Hematologic
- Uncommon (0.1% to 1%): Anemia, leukocytosis, leukopenia, lymphadenopathy, mucous membrane bleeding, mucosal hemorrhage, thrombocythemia, thrombocytopenia
- Rare (less than 0.1%): Agranulocytosis, aplastic anemia, basophilia, blood dyscrasias, eosinophilia, lymphocytosis, neutropenia, pancytopenia, prolonged bleeding time
- Postmarketing reports: INR increased, prolonged partial thromboplastin time, prothrombin time increased[Ref]
Hepatic
- Uncommon (0.1% to 1%): Abnormal liver function tests, ALT increased, AST increased
- Rare (less than 0.1%): Biliary pain, bilirubinemia, cholecystitis, cholelithiasis, hepatitis, jaundice, liver tenderness
- Postmarketing reports: Fatty liver, GGT elevation, hepatic reactions, liver damage, liver failure, liver necrosis[Ref]
Renal
- Uncommon (0.1% to 1%): Kidney calculus, kidney pain
- Rare (less than 0.1%): Anuria, blood urea nitrogen (BUN) increased, creatinine increased, glycosuria, kidney function abnormal, oliguria, pyelonephritis, uremia
- Postmarketing reports: Renal failure[Ref]
Hypersensitivity
- Uncommon (0.1% to 1%): Angioedema
- Rare (less than 0.1%): Anaphylactic reaction, anaphylaxis
- Frequency not reported: Hypersensitivity[Ref]
Endocrine
- Rare (0.1% to 0.01%): Goiter, gynecomastia (male), hyperthyroidism, hypothyroidism, inappropriate antidiuretic hormone secretion (SIADH)/syndrome of inappropriate antidiuretic hormone secretion, thyroid nodule, thyroiditis
- Very rare (less than 0.01%): Blood prolactin increased[Ref]
Oncologic
- Rare (less than 0.1%): Carcinoma, fibrocystic breast, multiple myeloma[Ref]
References
1. (2001) "Product Information. Effexor (venlafaxine)." Wyeth-Ayerst Laboratories
2. (2002) "Product Information. Effexor XR (venlafaxine)." Wyeth-Ayerst Laboratories
3. Cerner Multum, Inc. "UK Summary of Product Characteristics."
4. Cerner Multum, Inc. "Australian Product Information."
Frequently asked questions
- How long do venlafaxine withdrawal symptoms last?
- SSRIs vs SNRIs - What's the difference between them?
- What drugs can cause serotonin syndrome?
More about venlafaxine
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (2,792)
- Drug images
- Dosage information
- Patient tips
- During pregnancy
- Support group
- Drug class: serotonin-norepinephrine reuptake inhibitors
- Breastfeeding
- En español
Patient resources
Other brands
Professional resources
Other brands
Related treatment guides
Further information
Venlafaxine side effects can vary depending on the individual. Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
Note: Medication side effects may be underreported. If you are experiencing side effects that are not listed, submit a report to the FDA by following this guide.