Paliperidone (Monograph)
Brand name: Invega
Drug class: Atypical Antipsychotics
VA class: CN709
Chemical name: (±)-3-[2-[4-(6-fluoro-1,2-benzisoxazol-3-yl)-1-piperidyl]ethyl]-6,7,8,9-tetrahydro-9-hydroxy-2-methyl-4H-pyrido[1,2-a]pyrimidin-4-one
Molecular formula: C23H27FN4O3
CAS number: 144598-75-4
Warning
- Increased Mortality in Geriatric Patients
-
Substantially higher mortality rate (4.5%) in geriatric patients with dementia-related psychosis† receiving atypical antipsychotic agents (e.g., risperidone, aripiprazole, olanzapine, quetiapine) compared with those receiving placebo (2.6%).
-
Most fatalities resulted from cardiac-related events (e.g., heart failure, sudden death) or infections (mostly pneumonia).
-
Atypical antipsychotics are not approved for the treatment of dementia-related psychosis. (See Increased Mortality in Geriatric Patients with Dementia-related Psychosis under Cautions.)
Introduction
Atypical or second-generation antipsychotic agent.
Uses for Paliperidone
Schizophrenia
Acute and maintenance treatment of schizophrenia.
The American Psychiatric Association (APA) considers most atypical antipsychotic agents first-line drugs for the management of the acute phase of schizophrenia (including first psychotic episodes).
Paliperidone Dosage and Administration
Administration
Oral Administration
Administer orally once daily in the morning without regard to meals.
Paliperidone extended-release tablets should be swallowed whole, with fluids; do not chew, divide, or crush.
Dosage
Adults
Schizophrenia
Oral
6 mg once daily; dosage titration is not required.
If required, may increase dosage in increments of 3 mg daily at intervals of >5 days to a maximum dosage of 12 mg once daily; increase dosage only after clinical reassessment.
Maximal efficacy generally observed at dosage of 6 mg daily; dosages >6 mg trended toward greater clinical effects; however, weigh potential increased clinical efficacy against the potential for increased adverse effects.
Optimum duration of therapy is not known, but maintenance therapy with antipsychotics is well established. In responsive patients, continue as long as clinically necessary and tolerated, but at lowest possible effective dosage; periodically reassess need for continued therapy.
In patients with remitted first or multiple episodes, the APA recommends either indefinite maintenance therapy or gradual discontinuance of the antipsychotic with close follow-up and a plan to reinstitute treatment upon symptom recurrence. Consider antipsychotic therapy discontinuance only after ≥1 year of symptom remission or optimal response while taking antipsychotic. Indefinite maintenance treatment is recommended if multiple previous psychotic episodes or 2 episodes within 5 years.
Prescribing Limits
Adults
Schizophrenia
Oral
Maximum 12 mg once daily.
Special Populations
Hepatic Impairment
No dosage adjustment required in patients with mild to moderate hepatic impairment (Child-Pugh class A and B); not studied in patients with severe hepatic impairment. (See Distribution: Special Populations under Pharmacokinetics.)
Renal Impairment
Mild renal impairment (Clcr 50–79 mL/minute): Maximum 6 mg once daily.
Moderate to severe renal impairment (Clcr 10–49 mL/minute): Maximum 3 mg once daily. (See Elimination: Special Populations under Pharmacokinetics.)
Geriatric Patients
No dosage adjustments except those related to renal impairment. (See Renal Impairment under Dosage and Administration.)
Gender, Race, or Smoking Status
No dosage adjustment required.
Cautions for Paliperidone
Contraindications
-
Known hypersensitivity to paliperidone, risperidone, or any ingredient in the formulation.
Warnings/Precautions
Warnings
Increased Mortality in Geriatric Patients with Dementia-related Psychosis
Possible increased risk of death with use of atypical antipsychotics in geriatric patients with dementia-related psychosis.
Atypical antipsychotics, including paliperidone, are not approved for the treatment of dementia-related psychosis. (See Increased Mortality in Geriatric Patients in Boxed Warning and see Geriatric Use under Cautions.)
Prolongation of QT Interval
Paliperidone causes a modest increase in the corrected QT (QTc) interval.
Avoid use in patients with congenital prolonged QT interval, bradycardia, uncorrected electrolyte disorders (e.g., hypokalemia, hypomagnesemia), or a history of cardiac arrhythmias. Also avoid use in those receiving other drugs known to prolong the QTc interval. (See Drugs that Prolong QT Interval and also Specific Drugs under Interactions.)
Neuroleptic Malignant Syndrome
Neuroleptic malignant syndrome (NMS), a potentially fatal syndrome requiring immediate discontinuance of the drug and intensive symptomatic treatment, reported in patients receiving antipsychotic agents, including paliperidone.
Tardive Dyskinesia
Tardive dyskinesia, a syndrome of potentially irreversible, involuntary dyskinetic movements, reported. The APA recommends assessing patients receiving second-generation antipsychotic agents for abnormal involuntary movements every 12 months; for patients at increased risk for tardive dyskinesia, assess every 6 months. Consider discontinuance of paliperidone if signs and symptoms of tardive dyskinesia appear.
Hyperglycemia and Diabetes Mellitus
Severe hyperglycemia, sometimes associated with ketoacidosis, hyperosmolar coma, or death, reported in patients receiving atypical antipsychotic agents.
Closely monitor patients with preexisting diabetes mellitus for worsening of glucose control and perform fasting glucose tests at baseline and periodically for patients with risk factors for diabetes (e.g., obesity, family history of diabetes). If manifestations of hyperglycemia occur, perform fasting blood glucose testing.
GI Effects
Extended-release paliperidone tablets are a nondeformable material that does not appreciably change shape in the GI tract. Rare cases reported of obstructive symptoms in patients with known strictures in association with nondeformable, controlled-release formulations. Avoid administration to patients with severe, preexisting GI narrowing (either pathologic or iatrogenic).
Esophageal dysmotility and aspiration possible; use caution in patients at risk for aspiration pneumonia (e.g., those with advanced Alzheimer’s dementia).
General Precautions
Orthostatic Hypotension
Orthostatic hypotension and syncope reported. Use with caution in geriatric patients and in patients with known cardiovascular (e.g., heart failure, history of MI or ischemia, conduction abnormalities) or cerebrovascular disease or other conditions (e.g., dehydration, hypovolemia, concomitant antihypertensive therapy) that would predispose them to hypotension. Consider monitoring orthostatic vital signs in patients vulnerable to hypotension. (See Geriatric Use under Cautions.)
Nervous System Effects
Seizures may occur; use with caution in patients with a history of seizures or other conditions that may lower the seizure threshold (e.g., dementia of the Alzheimer’s type, geriatric patients). (See Geriatric Use under Cautions.)
Disruption of ability to regulate core body temperature possible. Use caution in patients exposed to conditions that may contribute to an elevation in core body temperature (e.g., dehydration, extreme heat, strenuous exercise, concomitant use of anticholinergic agents.)
Somnolence reported; potential impairment of judgment, thinking, or motor skills.
Antiemetic effect demonstrated in animals; also may occur in humans and mask manifestations of overdosage with certain drugs or of underlying conditions (e.g., intestinal obstruction, Reye’s syndrome, brain tumor).
Hematologic Effects
Thrombotic thrombocytopenic purpura reported in association with risperidone therapy; however, currently no reports of this effect with paliperidone.
Suicide
Attendant risk with psychotic illnesses; closely supervise high-risk patients. Prescribe in the smallest quantity consistent with good patient management to reduce the risk of overdosage.
Hyperprolactinemia
Elevated prolactin concentrations possible; may persist during chronic administration.
Concomitant Illnesses
Experience in patients with certain concomitant diseases is limited.
Possible increased risk of NMS and increased sensitivity to antipsychotic agents in patients with parkinsonian syndrome or dementia with Lewy bodies; manifestations of sensitivity may include confusion, obtundation, postural instability with more frequent falling, or extrapyramidal adverse effects. (See Geriatric Use under Cautions.)
Specific Populations
Pregnancy
Category C.
Risk for extrapyramidal and/or withdrawal symptoms (e.g., agitation, hypertonia, hypotonia, tardive dyskinetic-like symptoms, tremor, somnolence, respiratory distress, feeding disorder) in neonates exposed to antipsychotic agents during the third trimester; monitor neonates exhibiting such symptoms. Symptoms were self-limiting in some neonates but varied in severity; some infants required intensive support and prolonged hospitalization.
Lactation
Distributed into milk. Caution if used in nursing women.
Pediatric Use
Safety and efficacy not established in children <18 years of age.
Geriatric Use
No substantial differences in safety and efficacy relative to younger adults; however, manufacturer states greater sensitivity of some older individuals cannot be ruled out. Use with caution due to greater frequency of decreased hepatic, renal, and/or cardiac function and of concomitant disease and drug therapy observed in elderly patients. (See Concomitant Illnesses and also Nervous System Effects under Cautions and see Renal Impairment under Dosage and Administration.)
Consider monitoring orthostatic vital signs and renal function in geriatric patients. (See Orthostatic Hypotension under Cautions.)
Possible increased risk of death in geriatric patients with dementia-related psychosis. Substantial (1.6- to 1.7-fold) increase in mortality rate reported in geriatric patients with dementia who received atypical antipsychotic agents (i.e., risperidone, aripiprazole, olanzapine, quetiapine) for treatment of behavioral disorders; most fatalities resulted from cardiac-related events (e.g., heart failure, sudden death) or infections (e.g., pneumonia). In addition, adverse cerebrovascular effects, sometimes fatal, reported in geriatric patients with dementia-related psychosis receiving atypical antipsychotic agents (i.e., risperidone, aripiprazole, olanzapine). Paliperidone is not approved for the treatment of dementia-related psychosis. (See Increased Mortality in Geriatric Patients in Boxed Warning and see Increased Mortality in Geriatric Patients with Dementia-related Psychosis under Warnings in Cautions.)
Common Adverse Effects
Tremor, headache, orthostatic hypotension, tachycardia, somnolence, akathisia, insomnia, anxiety, extrapyramidal reaction, dizziness, dystonia, QTc interval prolongation, nausea, dyspepsia, weight gain.
Drug Interactions
In vivo results indicate that CYP2D6 and CYP3A4 play a limited role in overall elimination of paliperidone.
Drugs Affecting Hepatic Microsomal Enzymes
Inhibitors or inducers of CYP isoenzymes 2D6, 3A4, 1A2, 2A6, 2C9, and 2C19: Pharmacokinetic interaction unlikely.
Drugs Metabolized by Hepatic Microsomal Enzymes
Substrates of CYP isoenzymes 1A2, 2A6, 2C8/9/10, 2D6, 2E1, 3A4, or 3A5: Pharmacokinetic interaction unlikely.
Drugs Inhibiting P-glycoprotein Transport System
Does not inhibit P-glycoprotein; clinically relevant interactions unlikely.
Drugs that Prolong QT Interval
Potential pharmacologic interaction (additive effect on QT-interval prolongation); avoid concomitant use with drugs known to prolong the QT interval. (See Prolongation of QT Interval under Cautions.)
Protein-bound Drugs
Pharmacokinetic interactions unlikely.
Specific Drugs
|
Drug |
Interaction |
Comments |
|---|---|---|
|
Alcohol |
Possible additive CNS effects |
Avoid concomitant use |
|
Amiodarone |
Possible additive QT prolongation effects |
Avoid concomitant use |
|
Antiarrhythmics (e.g., procainamide, quinidine, sotalol) |
Possible additive QT prolongation effects |
Avoid concomitant use |
|
Chlorpromazine |
Possible additive QT prolongation effects |
Avoid concomitant use |
|
CNS agents |
Additive CNS effects |
Use with caution |
|
Dopamine agonists (e.g., levodopa) |
Potential antagonistic effects |
|
|
Fluoroquinolones (e.g., moxifloxacin, gatifloxacin) |
Possible additive QT prolongation effects |
Avoid concomitant use |
|
Hypotensive agents |
Additive hypotensive effects |
Use with caution; monitor for orthostatic hypotension in susceptible patients |
|
Paroxetine |
Possible increased paliperidone AUC in CYP2D6 extensive metabolizers |
Clinical importance unknown |
|
Risperidone |
Paliperidone is principal active metabolite of risperidone; possible additive paliperidone exposure |
|
|
Thioridazine |
Possible additive QT prolongation effects |
Avoid concomitant use |
Paliperidone Pharmacokinetics
Absorption
Bioavailability
Absolute oral bioavailability is 28%; single-dose peak plasma concentrations attained approximately 24 hours after dosing.
Food
Food increases rate and extent of absorption, and possible increase in exposure.
Special Populations
Decreased bioavailability in patients with decreased GI transit time (e.g., diarrhea); increased bioavailability in patients with increased GI transit time (e.g., GI neuropathy, diabetic gastroparesis). Changes in bioavailability more likely when transit time changes occur in the upper GI tract. (See GI Effects under Cautions.)
Distribution
Extent
Not known whether paliperidone crosses the placenta. Risperidone (the parent drug of paliperidone) crosses the placenta in rats. Paliperidone is distributed into human milk.
Plasma Protein Binding
74%.
Special Populations
In mild to moderate hepatic impairment (Child-Pugh class B); decreased total paliperidone exposure due to decreased protein binding. (See Hepatic Impairment under Dosage and Administration.)
Elimination
Metabolism
In vitro studies suggested a role for CYP2D6 and CYP3A4; however, in vivo results suggest a limited role.
Elimination Route
Paliperidone and its metabolites excreted in urine (80%), mainly as unchanged drug, and in the feces (11%).
Half-life
Terminal half-life is approximately 23 hours.
Special Populations
In patients with renal impairment, mean plasma terminal half-life is 24, 40, and 51 hours in individuals with mild, moderate, and severe renal impairment, respectively. (See Renal Impairment under Dosage and Administration.)
No difference in exposure or clearance of paliperidone between extensive metabolizers and poor metabolizers of CYP2D6.
Stability
Storage
Oral
Extended-release Tablets
25°C (may be exposed to 15–30°C); protect from moisture.
Actions
-
Benzisoxazole derivative; major active metabolite of risperidone.
-
Exact mechanism of antipsychotic action has not been fully elucidated; may involve antagonism of central dopamine type 2 (D2) receptors and serotonin type 2 (5-hydroxytryptamine [5-HT2A]) receptors.
-
Antagonism at other receptors (e.g., α1- and α2-adrenergic receptors, histamine H1 receptors) may contribute to other therapeutic and adverse effects.
-
Paliperidone possesses no affinity for cholinergic, muscarinic, or β1- and β2-adrenergic receptors.
Advice to Patients
-
Risk of orthostatic hypotension. Importance of using nonpharmacologic methods (e.g., sitting on edge of bed for several minutes upon waking, slowly rising from sitting to standing position) to minimize effects.
-
Risk of somnolence. Importance of avoiding driving, operating machinery, or performing hazardous tasks until the patient gains experience with the drug’s effects.
-
Importance of avoiding alcohol during paliperidone therapy.
-
Importance of informing clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs, dietary supplements, and/or herbal products, as well as any concomitant illnesses (e.g., cardiovascular disease, diabetes mellitus, seizures).
-
Importance of women informing clinicians if they are or plan to become pregnant or plan to breast-feed. Importance of clinicians informing patients about the benefits and risks of taking antipsychotics during pregnancy (see Pregnancy under Cautions). Importance of advising patients not to stop taking paliperidone if they become pregnant without consulting their clinician; abruptly stopping antipsychotic agents may cause complications.
-
Importance of avoiding overheating or dehydration.
-
Importance of swallowing paliperidone tablets whole with the aid of liquids; do not chew, divide, or crush tablets. Patients should not be concerned if they notice a tablet-like substance in their stool.
-
Importance of informing patients of other important precautionary information. (See Cautions.)
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
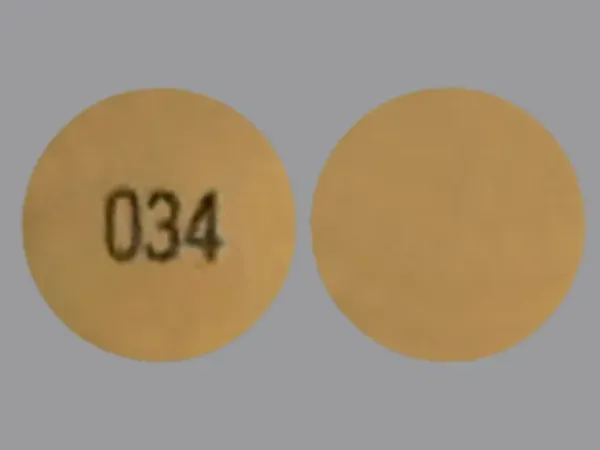
Oral |
Tablets, extended-release |
3 mg |
Invega (with povidone and propylene glycol) |
Janssen |
|
6 mg |
Invega (with povidone and propylene glycol) |
Janssen |
||
|
9 mg |
Invega (with povidone and propylene glycol) |
Janssen |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions March 30, 2017. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
Reload page with references included
Related/similar drugs
Frequently asked questions
- Can you drink alcohol while taking Invega Sustenna?
- Invega Sustenna vs Invega Trinza vs Invega Hafyera. What's the difference?
- How to transition to Invega Trinza from Invega Sustenna ?
- How do you give an Invega Sustenna injection?
- How to transition to Invega Hayfera from Invega Trinza or Invega Sustenna?
- How is Invega Trinza administered?
- What drugs cause tardive dyskinesia?
More about paliperidone
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (651)
- Drug images
- Side effects
- Dosage information
- During pregnancy
- Drug class: atypical antipsychotics
- Breastfeeding
Patient resources
Professional resources
Other brands
Invega, Invega Sustenna, Invega Trinza, Erzofri, Invega Hafyera