Dexlansoprazole (Monograph)
Brand name: Dexilant (formerly Kapidex)
Drug class: Proton-pump Inhibitors
Introduction
Acid- or proton-pump inhibitor; gastric antisecretory agent. The R-isomer of lansoprazole.
Uses for Dexlansoprazole
Gastroesophageal Reflux (GERD)
Short-term treatment of all grades of erosive esophagitis.
Maintenance therapy following healing of erosive esophagitis to reduce recurrence of the disease.
Short-term management of symptoms (e.g., heartburn) of GERD in patients without erosive esophagitis.
Crohn’s Disease-associated Ulcers
Some evidence for use of proton-pump inhibitors (e.g., omeprazole) for gastric acid suppressive therapy as an adjunct in the management of upper GI Crohn’s disease† [off-label], including esophageal, gastroduodenal, and jejunoileal disease.
Dexlansoprazole Dosage and Administration
General
Dispensing and Administration Precautions
-
The 2023 American Geriatrics Society (AGS) Beers Criteria for Potentially Inappropriate Medication (PIM) Use in Older Adults includes dexlansoprazole on the list of PIMs that are best avoided by older adults in most circumstances or under specific situations, such as certain diseases, conditions, or care settings. The criteria are intended to apply to adults 65 years of age and older in all ambulatory, acute, and institutional settings of care, except hospice and end-of-life care settings. For proton-pump inhibitors including dexlansoprazole, the Beers Criteria Expert Panel recommends that scheduled use for more than 8 weeks generally be avoided with certain exceptions.
Administration
Oral Administration
Administer orally once daily.
Administer without regard to food; however, if symptoms after a meal do not respond adequately to postprandial administration, consider preprandial administration (because the effect on gastric pH during the initial 4 hours after a dose may be decreased slightly when dexlansoprazole is taken after a meal).
Swallow capsules whole; alternatively, open capsule and sprinkle contents on a tablespoonful of applesauce and swallow immediately without chewing.
Dosage
Adults
Gastroesophageal Reflux
Chronic, lifelong therapy with a proton-pump inhibitor is appropriate for many GERD patients.
Treatment of Erosive Esophagitis
Oral60 mg once daily for up to 8 weeks.
Maintenance of Healing of Erosive Esophagitis
Oral30 mg once daily. Controlled studies beyond 6 months not performed.
GERD without Erosive Esophagitis
Oral30 mg once daily for 4 weeks.
Special Populations
Hepatic Impairment
No dosage adjustment necessary in mild hepatic impairment (Child-Pugh class A). Consider maximum dosage of 30 mg daily in moderate hepatic impairment (Child-Pugh class B). Not studied in severe hepatic impairment (Child-Pugh class C).
Renal Impairment
No dosage adjustment necessary.
Geriatric Patients
No dosage adjustment necessary.
Cautions for Dexlansoprazole
Contraindications
-
Known hypersensitivity to dexlansoprazole or any ingredient in the formulation.
Warnings/Precautions
Sensitivity Reactions
Hypersensitivity Reactions
Hypersensitivity reactions (e.g., anaphylaxis, toxic epidermal necrolysis, Stevens-Johnson syndrome) reported.
Gastric Malignancy
Response to dexlansoprazole therapy does not preclude presence of occult gastric neoplasm.
Clostridium difficile Infection
Proton-pump inhibitors associated with possible increased (1.4–2.75 times) risk of Clostridium difficile infection, including C. difficile-associated diarrhea and colitis (CDAD; also known as antibiotic-associated diarrhea and colitis or pseudomembranous colitis). Many patients also had other risk factors for CDAD. May be severe; colectomy and, rarely, death reported.
Use the lowest effective dosage and shortest duration of therapy appropriate for the patient's clinical condition.
Consider CDAD if persistent diarrhea develops and manage accordingly; initiate supportive therapy (e.g., fluid and electrolyte management), anti-infective therapy directed against C. difficile (e.g., metronidazole, vancomycin), and surgical evaluation as clinically indicated.
Bone Fracture
Several observational studies suggest that use of proton-pump inhibitors, particularly in high dosages (i.e., multiple daily doses) and/or for prolonged periods of time (i.e., ≥1 year), may be associated with increased risk of osteoporosis-related fractures of the hip, wrist, or spine. Magnitude of risk is unclear; causality not established. FDA is continuing to evaluate this safety concern.
Use the lowest effective dosage and shortest duration of therapy appropriate for the patient’s clinical condition.
Individuals at risk for osteoporosis-related fractures should receive an adequate intake of calcium and vitamin D; assess and manage these patients’ bone health according to current standards of care.
Hypomagnesemia
Hypomagnesemia, symptomatic and asymptomatic, reported rarely in patients receiving long-term therapy (≥3 months or, in most cases, >1 year) with proton-pump inhibitors, including dexlansoprazole. Serious adverse effects include tetany, seizures, tremors, carpopedal spasm, arrhythmias (e.g., atrial fibrillation, supraventricular tachycardia), and abnormal QT interval. Paresthesia, muscle weakness, muscle cramps, lethargy, fatigue, and unsteadiness may occur. Most patients required magnesium replacement and discontinuance of the proton-pump inhibitor. Hypomagnesemia resolved within 1 week (median) following discontinuance and recurred within 2 weeks (median) of rechallenge.
In patients expected to receive long-term proton-pump inhibitor therapy or in patients currently receiving digoxin or drugs that may cause hypomagnesemia (e.g., diuretics), consider measuring serum magnesium concentrations prior to initiation of prescription proton-pump inhibitor therapy and periodically thereafter.
Respiratory Effects
Administration of proton-pump inhibitors has been associated with an increased risk for developing certain infections (e.g., community-acquired pneumonia).
Possible Prescribing and Dispensing Errors
Ensure accuracy of prescription; similarity in spelling of Kapidex (former trade name for dexlansoprazole) and Casodex (trade name for bicalutamide, a nonsteroidal antiandrogenic antineoplastic agent ) or Kadian (a trade name for morphine sulfate, an opiate agonist analgesic ) may result in errors. In April 2010, manufacturer changed trade name for dexlansoprazole from Kapidex to Dexilant to avoid future errors.
Also be aware of potential for Kapidex to be confused with Capadex (fixed-combination propoxyphene/acetaminophen preparation that is available via the Internet and is marketed in certain other countries [e.g., Australia]).
Specific Populations
Pregnancy
Category B.
Lactation
Not known whether dexlansoprazole is distributed into milk; however, lansoprazole and its metabolites are distributed into milk in rats. Discontinue nursing or the drug.
Pediatric Use
Safety and efficacy not established in children <18 years of age.
Geriatric Use
No substantial differences in safety and efficacy relative to younger adults, but increased sensitivity of some older patients cannot be ruled out.
Hepatic Impairment
Systemic exposure to dexlansoprazole is increased approximately twofold in individuals with moderate hepatic impairment. Not studied in severe hepatic impairment. (See Hepatic Impairment under Dosage and Administration.)
Common Adverse Effects
Diarrhea, abdominal pain, nausea, upper respiratory infection, vomiting, flatulence.
Drug Interactions
Metabolized by CYP2C19 and CYP3A4.
Unlikely to inhibit CYP isoenzymes 1A1, 1A2, 2A6, 2B6, 2C8, 2C9, 2C19, 2D6, 2E1, or 3A4.
Drugs Metabolized by Hepatic Microsomal Enzymes
Substrates of CYP isoenzymes 1A1, 1A2, 2A6, 2B6, 2C8, 2C9, 2C19, 2D6, 2E1, or 3A: Pharmacokinetic interaction unlikely.
Drugs that Cause Hypomagnesemia
Potential pharmacologic interaction (possible increased risk of hypomagnesemia). Consider monitoring magnesium concentrations prior to initiation of prescription proton-pump inhibitor therapy and periodically thereafter. (See Hypomagnesemia under Cautions.)
Specific Drugs
|
Drug |
Interaction |
Comments |
|---|---|---|
|
Atazanavir |
Possible altered oral absorption of atazanavir, resulting in decreased plasma atazanavir concentrations; possible loss of virologic response |
Manufacturer of dexlansoprazole states that concomitant administration with atazanavir is not recommended Antiretroviral treatment-naive patients: If a proton-pump inhibitor is used concomitantly with atazanavir, administer ritonavir-boosted atazanavir (atazanavir 300 mg and ritonavir 100 mg once daily with food); administer the proton-pump inhibitor approximately 12 hours before ritonavir-boosted atazanavir For treatment-naive patients, dosage of proton-pump inhibitor should not exceed omeprazole 20 mg daily (or equivalent) Antiretroviral treatment-experienced patients: Concomitant use of proton-pump inhibitors with atazanavir not recommended |
|
Clopidogrel |
Certain CYP2C19 inhibitors (e.g., omeprazole, esomeprazole) reduce exposure to clopidogrel’s active metabolite and decrease platelet inhibitory effect; potentially may reduce clopidogrel’s clinical efficacy Dexlansoprazole, lansoprazole, or pantoprazole had less effect on clopidogrel's antiplatelet activity than did omeprazole or esomeprazole; Dexlansoprazole decreased exposure to the metabolite by about 9%; observed effects on metabolite exposure and clopidogrel-induced platelet inhibition not considered clinically important |
Manufacturer of dexlansoprazole states clopidogrel dosage adjustment not required if used with recommended dexlansoprazole dosages Assess risks and benefits of concomitant proton-pump inhibitor and clopidogrel use in individual patients American College of Cardiology Foundation/American College of Gastroenterology/American Heart Association (ACCF/ACG/AHA) states that GI bleeding risk reduction with concomitant proton-pump inhibitor in patients with risk factors for GI bleeding (e.g., advanced age; concomitant use of warfarin, corticosteroids, or NSAIAs; H. pylori infection) may outweigh potential reduction in cardiovascular efficacy of antiplatelet treatment associated with a drug-drug interaction. In patients without such risk factors, ACCF/ACG/AHA states that risk/benefit balance may favor use of antiplatelet therapy without a proton-pump inhibitor. If concomitant therapy with a proton-pump inhibitor and clopidogrel is deemed necessary, consider using an agent with little or no CYP2C19-inhibitory activity; alternatively, consider using a histamine H2-receptor antagonist (ranitidine, famotidine, nizatidine) but not cimetidine (also a potent CYP2C19 inhibitor) |
|
Diazepam |
Effect on diazepam pharmacokinetics unlikely |
|
|
Digoxin |
Hypomagnesemia (e.g., resulting from long-term use of proton-pump inhibitors) sensitizes the myocardium to digoxin and, thus, may increase risk of digoxin-induced cardiotoxic effects See table entry for gastric pH-dependent drugs |
Consider monitoring magnesium concentrations prior to initiation of prescription proton-pump inhibitor therapy and periodically thereafter |
|
Diuretics (i.e., loop or thiazide diuretics) |
Possible increased risk of hypomagnesemia |
Consider monitoring magnesium concentrations prior to initiation of prescription proton-pump inhibitor therapy and periodically thereafter |
|
Fosamprenavir |
Use of esomeprazole with fosamprenavir (with or without ritonavir) did not substantially affect concentrations of amprenavir (active metabolite of fosamprenavir) |
No dosage adjustment required when proton-pump inhibitors used with fosamprenavir (with or without ritonavir) |
|
Gastric pH-dependent drugs (e.g., ampicillin esters, digoxin, iron salts, ketoconazole) |
Dexlansoprazole may alter drug absorption |
|
|
Lopinavir |
Lopinavir/ritonavir: Omeprazole had no clinically important effect on plasma concentrations or AUC of lopinavir |
No dosage adjustment required when proton-pump inhibitors used with lopinavir/ritonavir |
|
Methotrexate |
Possible delayed clearance and increased serum concentrations of methotrexate and/or its metabolite hydroxymethotrexate; possible methotrexate toxicity Reported mainly with high-dose methotrexate (300 mg/m2 to 12 g/m2), but also reported with low dosages (e.g., 15 mg per week) |
Manufacturer of dexlansoprazole recommends considering temporary discontinuance of proton-pump inhibitor therapy in some patients receiving high-dose methotrexate Some clinicians recommend withholding the proton-pump inhibitor for several days before and after administration of either high-dose or low-dose methotrexate or, alternatively, substituting a histamine H2-receptor antagonist for the proton-pump inhibitor |
|
Phenytoin |
Effect on phenytoin pharmacokinetics unlikely |
|
|
Raltegravir |
Omeprazole increased peak plasma concentration and AUC of raltegravir |
No dosage adjustment recommended when proton-pump inhibitors used with raltegravir |
|
Rilpivirine |
Omeprazole decreased plasma concentrations and AUC of rilpivirine |
Concomitant use of rilpivirine and proton-pump inhibitors contraindicated |
|
Saquinavir |
Ritonavir-boosted saquinavir: Omeprazole increased peak plasma concentration and AUC of saquinavir |
Caution advised if proton-pump inhibitor used with ritonavir-boosted saquinavir; monitor for saquinavir toxicity |
|
Tacrolimus |
Possible increase in whole blood tacrolimus concentrations, particularly in transplant patients with intermediate or poor metabolizer phenotypes for CYPC19 |
|
|
Theophylline |
Effect on theophylline pharmacokinetics unlikely |
|
|
Warfarin |
No change in warfarin pharmacokinetics or INR observed in healthy individuals given warfarin 25 mg on day 6 of an 11-day course of dexlansoprazole 90 mg once daily; however, increased PT and INR reported in patients receiving warfarin concomitantly with proton-pump inhibitors |
May need to monitor PT and INR |
Dexlansoprazole Pharmacokinetics
Absorption
Bioavailability
Commercially available capsules contain 2 types of enteric-coated granules that dissolve at different pH values. Following oral administration, an initial (smaller) peak plasma concentration occurs at 1–2 hours followed by a second (larger) peak concentration at 4–5 hours.
Duration
Following once-daily administration for 5 days, gastric pH is >4 for 17 hours per day with dexlansoprazole 60 mg versus 14 hours per day with lansoprazole 30 mg.
Food
Administration in fed versus fasted state not associated with significant difference in mean gastric pH; however, effect on gastric pH during initial 4 hours after a dose may be decreased slightly when dexlansoprazole is taken after a meal. (See Oral Administration under Dosage and Administration.)
Distribution
Plasma Protein Binding
96–99%.
Elimination
Metabolism
Extensively metabolized in the liver by oxidation, reduction, and subsequent formation of inactive sulfate, glucuronide, and glutathione conjugates. CYP2C19 and CYP3A4 are involved.
Major circulating metabolite varies depending on CYP2C19 phenotype, but dexlansoprazole is the major circulating form of the drug regardless of CYP2C19 phenotype.
Elimination Route
Eliminated in urine (51%) and feces (48%); unchanged drug is not recovered in urine.
Half-life
Approximately 1–2 hours.
Special Populations
Intermediate or poor metabolizers of CYP2C19 substrates: Systemic exposure to dexlansoprazole generally is increased. In Japanese men, AUC increased twofold in intermediate metabolizers and up to 12-fold in poor metabolizers compared with extensive metabolizers.
Moderate hepatic impairment: Twofold increase in AUC.
Renal impairment: Pharmacokinetic alterations not expected.
Geriatric individuals: Half-life of 2.2 hours (versus 1.5 hours in younger individuals); not considered clinically important.
Stability
Storage
Oral
Capsules
25°C (may be exposed to 15–30°C).
Compatibility
Oral
Capsules
Immediately use extemporaneous mixtures of capsule contents and applesauce.
Actions
-
Dexlansoprazole is the R-isomer of lansoprazole (a racemic mixture of R- and S-isomers). Both isomers inhibit hydrogen-potassium ATPase, but plasma clearance of dexlansoprazole is slower than that of S-lansoprazole.
-
Proton-pump inhibitors inhibit basal and stimulated gastric acid secretion.
-
Dexlansoprazole binds to and inactivates hydrogen-potassium ATPase (proton, hydrogen, or acid pump) in gastric parietal cells, blocking the final step in secretion of hydrochloric acid; results in potent, long-lasting inhibition of gastric acid secretion.
Advice to Patients
-
Importance of swallowing capsule whole or, alternatively, of opening capsule and sprinkling contents on a tablespoonful of applesauce and swallowing immediately without chewing. Dexlansoprazole may be administered without regard to food (see Oral Administration under Dosage and Administration).
-
Importance of continuing therapy for the entire treatment course, unless directed otherwise.
-
Importance of advising patients that use of multiple daily doses of the drug for an extended period of time may increase the risk of fractures of the hip, wrist, or spine.
-
Risk of hypomagnesemia; importance of immediately reporting and seeking care for any cardiovascular or neurologic manifestations (e.g., palpitations, dizziness, seizures, tetany).
-
Importance of informing clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs and herbal supplements, as well as any concomitant illnesses.
-
Possible increased risk of Clostridium difficile infection; importance of contacting a clinician if persistent watery stools, abdominal pain, and fever occur.
-
Importance of informing clinicians of any symptoms suggestive of an allergic reaction (e.g., facial swelling, rash).
-
Importance of women informing their clinicians if they are or plan to become pregnant or plan to breast-feed.
-
Importance of informing patients of other important precautionary information. (See Cautions.)
Additional Information
The American Society of Health-System Pharmacists, Inc. represents that the information provided in the accompanying monograph was formulated with a reasonable standard of care, and in conformity with professional standards in the field. Readers are advised that decisions regarding use of drugs are complex medical decisions requiring the independent, informed decision of an appropriate health care professional, and that the information contained in the monograph is provided for informational purposes only. The manufacturer’s labeling should be consulted for more detailed information. The American Society of Health-System Pharmacists, Inc. does not endorse or recommend the use of any drug. The information contained in the monograph is not a substitute for medical care.
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Capsules, delayed-release (containing enteric-coated granules) |
30 mg |
Dexilant |
Takeda |
|
60 mg |
Dexilant |
Takeda |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions June 10, 2025. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
† Off-label: Use is not currently included in the labeling approved by the US Food and Drug Administration.
Reload page with references included
Related/similar drugs
More about dexlansoprazole
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (253)
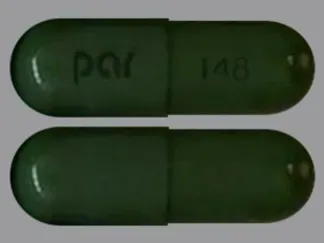
- Drug images
- Side effects
- Dosage information
- During pregnancy
- Drug class: proton pump inhibitors
- Breastfeeding
- En español