Augmentin
Generic name: amoxicillin and clavulanate potassium [ am-OK-i-SIL-in-KLAV-ue-LAN-ate-poe-TAS-ee-um ]
Drug class: Beta-lactamase inhibitors
What is Augmentin?
Augmentin contains a combination of amoxicillin and clavulanate potassium. Amoxicillin is a penicillin antibiotic that fights bacteria in the body. Clavulanate potassium is a beta-lactamase inhibitor that helps prevent certain bacteria from becoming resistant to amoxicillin.
Augmentin is prescription antibiotic used to treat many different infections caused by bacteria, such as sinusitis, pneumonia, ear infections, bronchitis, urinary tract infections, and infections of the skin.
Warnings
You should not use Augmentin if you have severe kidney disease, if you have had liver problems or jaundice while taking amoxicillin and clavulanate potassium, or if you are allergic to any penicillin or cephalosporin antibiotic, such as Amoxil, Ceftin, Cefzil, Moxatag, Omnicef, and others.
If you switch from one tablet form to another (regular or extended-release tablet), take only the new tablet form and strength prescribed for you. Amoxicillin and clavulanate may not be as effective or could be harmful if you do not use the exact tablet form your doctor has prescribed.
Amoxicillin and clavulanate potassium can pass into breast milk and may harm a nursing baby. Do not use this medication without telling your doctor if you are breast-feeding a baby.
Augmentin can make birth control pills less effective. Ask your doctor about using a non-hormone method of birth control (such as a condom, diaphragm, spermicide) to prevent pregnancy while taking amoxicillin and clavulanate potassium.
Warnings
You should not use Augmentin if you have severe kidney disease, if you have had liver problems or jaundice while taking amoxicillin and clavulanate potassium, or if you are allergic to any penicillin or cephalosporin antibiotic,
Before taking this medicine
You should not use Augmentin if you are allergic to amoxicillin and clavulanate or if:
-
you have severe kidney disease (or if you are on dialysis);
-
you have had liver problems or jaundice while taking amoxicillin and clavulanate potassium; or
-
you are allergic to any penicillin or cephalosporin antibiotic, such as Amoxil, Ceftin, Cefzil, Moxatag, Omnicef, and others.
To make sure Augmentin is safe for you, tell your doctor if you have:
-
liver disease (hepatitis or jaundice);
-
kidney disease; or
The liquid may contain phenylalanine. Tell your doctor if you have phenylketonuria (PKU).
Tell your doctor if you are pregnant or breastfeeding.
Augmentin can make birth control pills less effective. Ask your doctor about using a non-hormonal birth control (condom, diaphragm, cervical cap, or contraceptive sponge) to prevent pregnancy.
Do not give this medicine to a child without medical advice.
How should I take Augmentin?
Take Augmentin exactly as prescribed by your doctor. Follow all directions on your prescription label and read all medication guides or instruction sheets.
Augmentin may work best if you take it at the start of a meal.
Take the medicine every 12 hours.
Do not crush or chew the extended-release tablet. Swallow the pill whole, or break the pill in half and take both halves one at a time. Tell your doctor if you have trouble swallowing a whole or half pill.
Shake the oral suspension (liquid) before you measure a dose. Use the dosing syringe provided, or use a medicine dose-measuring device (not a kitchen spoon).
This medicine can affect the results of certain medical tests. Tell any doctor who treats you that you are using Augmentin.
Use this medicine for the full prescribed length of time, even if your symptoms quickly improve. Skipping doses can increase your risk of infection that is resistant to medication. Augmentin will not treat a viral infection such as the flu or a common cold.
Store the tablets at room temperature away from moisture and heat.
Store the liquid in the refrigerator. Throw away any unused liquid after 10 days.
What happens if I miss a dose?
Take the medicine as soon as you can, but skip the missed dose if it is almost time for your next dose. Do not take two doses at one time.
What happens if I overdose?
Seek emergency medical attention or call the Poison Help line at 1-800-222-1222.
Overdose can cause nausea, vomiting, stomach pain, diarrhea, skin rash, drowsiness, hyperactivity, and decreased urination.
What to avoid
Avoid taking this medicine together with or just after eating a high-fat meal. This will make it harder for your body to absorb the medication.
Antibiotic medicines can cause diarrhea, which may be a sign of a new infection. If you have diarrhea that is watery or bloody, call your doctor before using anti-diarrhea medicine.
Augmentin side effects
Get emergency medical help if you have signs of an allergic reaction to Augmentin (hives, difficult breathing, swelling in your face or throat) or a severe skin reaction (fever, sore throat, burning eyes, skin pain, red or purple skin rash with blistering and peeling).
Stop using Augmentin and seek medical treatment if you have a serious drug reaction that can affect many parts of your body. Symptoms may include skin rash, fever, swollen glands, muscle aches, severe weakness, unusual bruising, or yellowing of your skin or eyes.
Call your doctor at once if you have:
-
severe stomach pain, diarrhea that is watery or bloody (even if it occurs months after your last dose);
-
pale or yellowed skin, dark colored urine, fever, confusion or weakness;
-
loss of appetite, upper stomach pain;
-
little or no urination; or
-
easy bruising or bleeding.
Common Augmentin side effects may include:
-
nausea, vomiting; diarrhea;
-
rash, itching;
-
vaginal itching or discharge; or
This is not a complete list of side effects and others may occur. Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
What other drugs will affect Augmentin?
Tell your doctor about all your other medicines, especially:
-
probenecid; or
This list is not complete. Other drugs may interact with amoxicillin and clavulanate potassium, including prescription and over-the-counter medicines, vitamins, and herbal products. Not all possible drug interactions are listed here.
Popular FAQ
From 5% to 10% of children will develop a rash from amoxicillin after taking it, which in most cases, is considered a side effect of amoxicillin and not an allergic rash. But in a small number of cases, the rash will be a sign of an allergic reaction which means the amoxicillin will need to be stopped right away. Continue reading
More FAQ
- Can you drink alcohol while taking Augmentin?
- What is the best antibiotic to treat a sinus infection?
- What are the best antibiotics for pneumonia?
- Does AMOX-CLAV treat an abcessed tooth?
- Can Amox-Clav tablets be crushed?
More about Augmentin (amoxicillin / clavulanate)
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (444)
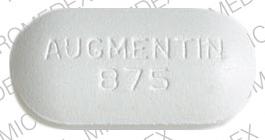
- Drug images
- Side effects
- Dosage information
- Patient tips
- During pregnancy
- Support group
- Drug class: beta-lactamase inhibitors
- En español
Patient resources
- Augmentin (Amoxicillin/Clavulanate Chewable Tablets) patient information
- Augmentin (Amoxicillin/Clavulanate Suspension)
- Augmentin (Amoxicillin/Clavulanate Tablets)
Other brands
Professional resources
- Augmentin prescribing information
- Augmentin Chewable (FDA)
- Augmentin Oral Suspension (FDA)
- Amoxicillin/Clavulanate (AHFS Monograph)
Other brands
Other formulations
Related treatment guides
Further information
- Your pharmacist or dcotor can provide more information about Augmentin.
Remember, keep this and all other medicines out of the reach of children, never share your medicines with others, and use Augmentin only for the indication prescribed.
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
Copyright 1996-2024 Cerner Multum, Inc. Version: 14.01.